NHS activity tracker
Introduction
As the summer comes to an end COVID-19 pressures are slowing beginning to rise once again. There are now over 6,300 COVID-19 positive patients in hospitals across England and many trust leaders are concerned that with schools and universities returning we may continue to see further increases in community infections like last year.
With more COVID-19 patients being admitted each day trusts are still having to manage their capacity effectively to treat both COVID -19 patients and carry out non-COVID care. This week’s NHS and social care funding announcement also sharpens the focus on the operational challenge ahead. The figures published today show that the NHS has had a very busy summer with significant pressure across the urgent and emergency care pathway and more people in touch with mental health services than ever before.
This month’s performance figures
Each month NHS England and NHS Improvement publish statistics looking at activity and performance across a range of services including urgent and emergency care, routine care, cancer, and mental health. Below we set out the latest trend for each clinical area:
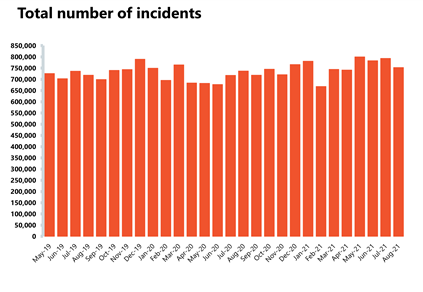
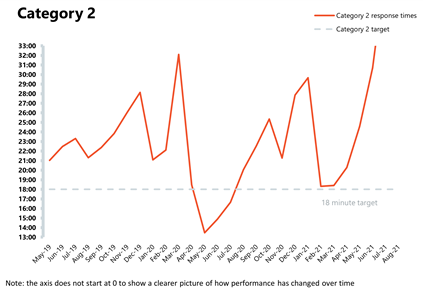
NHS 111 and ambulance: Ambulance category 1 incidents have fallen in the latest month, however demand and pressures remain high across the urgent and emergency care pathway compared to pre-pandemic levels.
- Ambulance category 1 incidents, those requiring immediate intervention and resuscitation, decreased by 9.3% since last month to 74,096 (7,589 fewer incidents). However, compared to two years ago, before the pandemic, they have increased by 28.7% which means demand pressures remain high.
- The ambulance service has missed the average response time target of seven minutes for category 1 calls for the fourth consecutive month with a national average of 8 minutes 28 seconds. The average response time for category 2 calls also deteriorated further, missing the 18-minute target with an average time of 39 minutes. This is the second worst performance on record after last month.
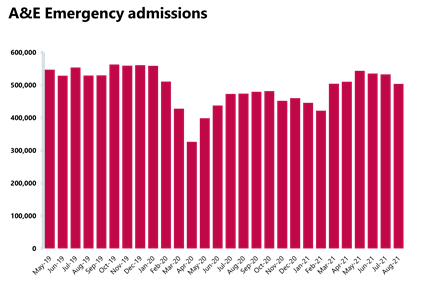
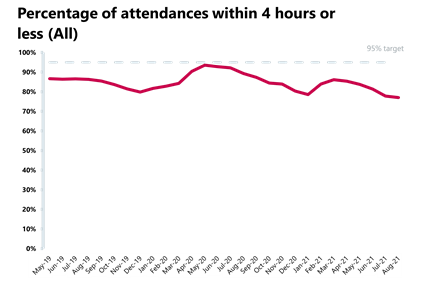
A&E and emergency care: activity across emergency departments dipped slightly this month, falling below levels seen before the pandemic, but performance against national targets continues to deteriorate and has reached the worst performance ever registered.
- In August 2021, there were 2.03 million A&E attendances, a decrease of 4.1% compared to two years ago before the pandemic.
- There were 503,871 emergency admissions in August 2021, a decrease of 5.4% since the previous month but 18.6% higher than one year ago (August 2020). However, this figure is 4.1% lower than two years ago in August 2019 before the pandemic.
- Performance against the 95% target continues to deteriorate and reached 77%, meaning it is the worst performance on record.
- The number of patients waiting longer than 4 hours has increased this month by 7% to 96,013 (6,245 more), whereas the number of patients waiting more than 12 hours also increased by 26% on last month to 2,794 (579 more).
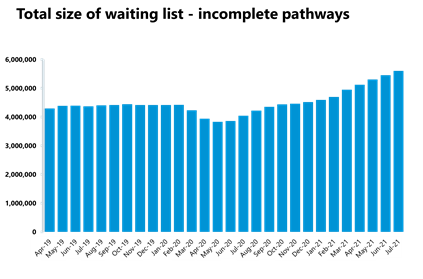
Elective care: referrals are still outstripping activity as the waiting list continues to grow to the highest level seen in the last 10 years, reaching 5.61 million. Trusts continue to reduce the number of long waits, with patients waiting 52 weeks or more decreasing for the fourth consecutive month.
- In July 2021, the size of the elective care waiting list increased by 2.8% to 5.61 million (152,410 more) since June 2021. This is the highest level seen in the current records over the last decade.
- The number of patients waiting more than 18 weeks increased by 4.4%. With 75,168 more people waiting over 18 weeks, performance against the 18 weeks standard worsened, falling by 0.5 percentage points to 68.3%.
- The number of people waiting over 52 weeks has decreased for the fourth month running. The number of long waits fell by 11,701 to 293,102, a decrease of 3.8% from June 2021 but an increase of 252% compared to last year.
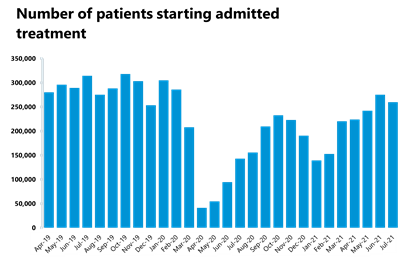
- Inpatient care activity decreased slightly in July 2021 compared to last month. The number of admitted inpatient pathways decreased by 5.7% compared to the previous month, meaning that a total of 259,642 inpatient treatments were carried out.
- Non-admitted pathways also decreased from last month, with the NHS delivering 999,991 elective non-admitted pathways – a decrease of 5.8% on the previous month.
- There was a slight decrease of new RTT pathways in June, with 1.6 million new ones, resulting in the overall size of the waiting list growing as new referrals are still outstripping activity.
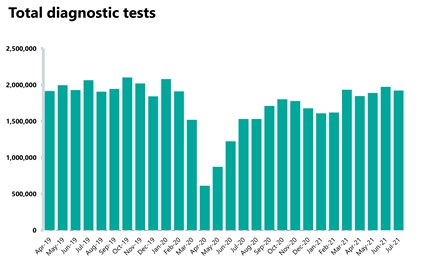
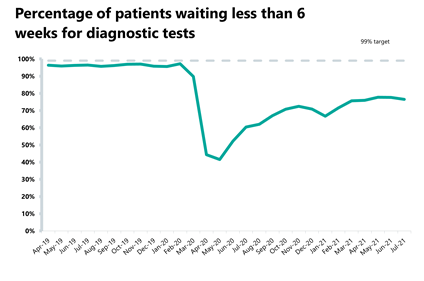
Diagnostics: diagnostic activity decreased in July 2021 and remains below pre-pandemic levels.
- The number of tests carried out in July 2021 has decreased by 2.5% to 1.92 million (49,951 fewer) compared to June 2021. Compared to two years ago before the pandemic, there are now 6.8% fewer tests carried out (140,567 fewer).
- Compared to last year, the number of MRI, CT and colonoscopy tests all increased by 21.6%, 14.1% and 69.5%, respectively. When looking at diagnostic activity from July 2019, before the pandemic, the number of MRI tests is down by 4.6% (14,510 fewer), the number CT tests increased by 8.7% (47,102 more), and the number of colonoscopy tests increased by 0.9% (428 more).
- The diagnostic waiting list has decreased by 3.3% to 1.33 million since the previous month, with 23.5% of people waiting six weeks or more for a test in July. This figure is slightly up from 22.4% last month but still missing the 1% target again this month.
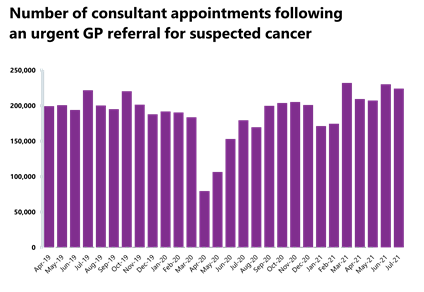
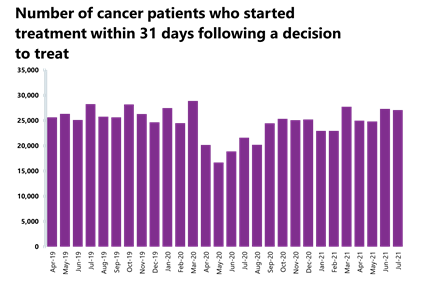
Cancer: Cancer activity is now at pre-pandemic levels but both activity and performance have deteriorated since last month and all targets have been missed.
- A total of 224,086 people were seen within two weeks of an urgent referral for a suspected cancer – this is down by 2.6% from the previous month, meaning 6,024 fewer consultations. Nevertheless, it is still 1% greater than two years ago, meaning activity is at pre-pandemic levels. 85.6% of urgent GP referrals were seen within two weeks, missing the 93% standard.
- The number of people on the 31-day pathway, which aims for one month between starting treatment following a decision to treat, also fell by 0.8% this month with 221 fewer people. 94.7% of people started treatment within one month of the decision to treat, representing a slight increase in performance compared to the previous month, but falling short of the 96% standard.
- The number of people waiting 62 days from urgent GP referral to starting treatment also improved since the previous month, with a 1.2% increase to 14,386 people. This is a decrease of 3.6% from two years ago before the pandemic. 72.1% of the people who started treatment have done so within 62 days of their urgent GP referral, representing a 1.2% point decrease from the previous month and missing the 85% standard.
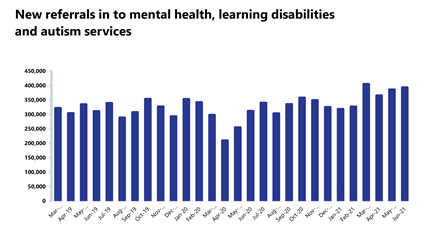
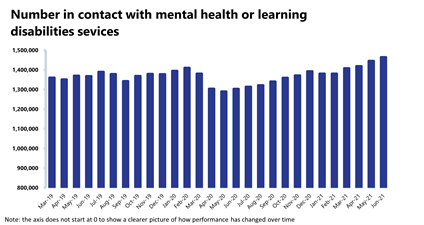
Mental health: The number of people in contact with mental health services continues to rise each month as contacts are at the highest level since records began. New referrals also continue to rise and remain considerably higher than pre-pandemic levels.
- In June 2021, mental health referrals increased by 1.9% to 392,703 (7,273 more referrals). Compared to a year ago, referrals have increased by 26.1% (81,310 more referrals). Compared to June 2019, referrals have increased by 26.6% (82,505 more referrals) which means that demand pressures remain high on mental health services.
- The number of people in contact with mental health services has increased by 1.3% to 1.46 million (19,059 more people in contact). This is the highest number of people in contact since records began. Compared to a year ago, there are 12.4% more people in contact with mental health services (161,351 more people).
- In June 2021, there were 2.1 million care contacts attended (up by 3.2% and 65,676 more than the previous month). In comparison to a year ago, there are now 2.3% more care contacts attended (46,477 more care contacts).
- In June 2021, the number of out of area placements (OAPs) decreased to 695 (50 fewer OAPs than last month). Compared to a year ago, OAPs have increased by 13.9% (85 more OAPs). In comparison to two years ago there are 13.7% fewer OAPs (110 fewer OAPs).
Our view
This month’s data shows that staff are working tirelessly across physical and mental health services to treat as many patients as possible. The urgent and care pathway still remains very busy, with more incidents requiring an ambulance than before the pandemic and long waits of over 12 hours in A&E continue to increase for a small proportion of patients.
Across a few areas there was an expected small fall in activity. Trust leaders predicted they would not be able to continue with month on month increases in elective care and diagnostics due to staff taking well deserved annual leave over the summer. Cancer services continue to deliver activity akin to pre-pandemic levels and mental health services are now in contact with more people than ever before.
The NHS is continuing to claw back progress to meet the day to day needs of patients, while still treating a once again growing COVID-19 patient presence across wards and intensive care units.
In the short-term, the risk trusts will carry is only going to rise as we head into the winter months. Trust leaders are extremely concerned about further rises in demand, the predicted increases in respiratory syncytial virus infections and the addition of seasonal flu and norovirus which were largely absent last year.
It is against this backdrop that this week’s funding announcements for the NHS took place, providing a much needed boost to resources. This additional resource is critical to meeting patients’ needs – reflecting the rising cost of frontline care driven by COVID-19 and the very real need to tackle the backlog of care.
But even with this extra funding, we must be honest about the scale of the challenge ahead for the NHS.
A&E
Cancer
RTT
Diagnostic tests
Ambulance indicators
Mental health
No let-up in challenges facing the NHS as waiting list hits record high
Responding to the latest monthly combined performance data from NHS England and NHS Improvement, the deputy chief executive of NHS Providers, Saffron Cordery said: "Today’s figures confirm there has been no let-up in the demand facing the NHS. A staggering 5.6million patients are now waiting to start planned treatment- the highest since records began in August 2007.
"Urgent and emergency care services face “winter conditions”, with incredibly high demand for ambulance services and rocketing numbers of patients waiting longer than 12 hours to be admitted. And the number of people in contact with mental health services – almost one-and-a-half million – is at record levels. Frontline trusts and staff have been working exceptionally hard to meet the demands presented by COVID-19 and non-COVID care in incredibly challenging circumstances.
"It is of great credit to them that the numbers of people starting cancer treatment are now back to pre-pandemic levels. But we cannot escape the fact that the NHS continues to face a multitude of challenges as we head into the difficult winter months. These include continuing COVID-19 pressures, with daily infections rising. As night follows day, we know that as cases rise, so do hospital admissions.
"Trust leaders are looking on anxiously as the number of people admitted to hospitals with COVID has increased by over 1000 in the space of a month with no signs of easing. It is against this daunting backdrop that this week’s funding announcements for the NHS took place, providing a much needed boost. This additional resource is critical to meeting patients’ needs – reflecting the rising cost of frontline care driven by COVID-19 and the very real need to tackle the backlog of care. But even with this extra funding, we must be honest with the public about the scale of the challenge ahead for the NHS. We are in this for the long haul".