

Context
Up until September, when the number of COVID-19 cases began to quickly rise again, the NHS was broadly sustaining its recovery trajectory across all services. In July, mental health services received more referrals and delivered more care contacts than ever before. In addition, the number of emergency admissions, diagnostic tests and elective operations all increased month on month since April. The NHS was certainly on track to deliver the ambitious targets set by NHS England and NHS Improvement as part of the phase 3 recovery plan.
In response to the rise in COVID-19 infections, England is currently in a national lockdown period to help reduce transmissions in the community and COVID-19 hospital admissions, and prevent more COVID-19 deaths. While it will take some weeks to see the impact of the lockdown on these pandemic markers, the data over the past few weeks has confirmed that we are moving through the second wave of the pandemic.
Trusts have been working extremely hard to restore non-COVID services while factoring in the need to redesign services, change hospital configurations, increase infection control measures and implement social distancing. Although there were very few COVID-19 hospitalisations over the summer, COVID-19 activity has rapidly increased again and this second wave is important context when discussing or evaluating the restoration of non-COVID services.
The data published today covers September and October. This data, as well as some more up to date real time information published in a press statement from NHS E/I, shows that the NHS is responding incredibly well to the increase in COVID-19 presentations.
COVID-19 is not impacting the NHS in a uniform way and there is significant local and regional variation in the experiences of providers. We know the regional variation will include some localised stepping down of some services, but broadly speaking, September activity levels are being maintained. This suggests that at a macro national level, the second wave is yet to push the recovery trajectory further back.
This month’s performance figures
Each month NHS England and Improvement publishes statistics looking at performance across a range of services including urgent and emergency care, routine care, cancer, and mental health.
Below we highlight some of the latest trends and figures across NHS activity and performance:
NHS activity
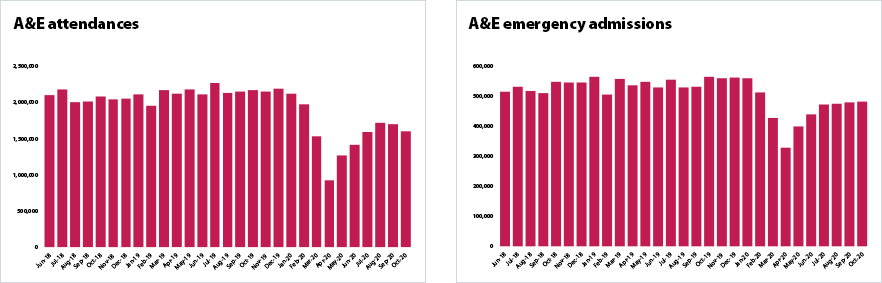
- In October, A&E departments saw a further reduction in attendances. A&E attendances fell slightly by 5.5% from last month to 1.59million – 26.3% lower than in September 2019. This could be a direct result of local lockdowns and the surge of COVID-19 infections across the country.
- Emergency admissions have risen each month since April. Emergency admissions increased marginally from September levels to 481,846 but remain 14.4% lower than in October 2019. Since the peak of the first wave in April 2020, admissions have increased by 47.5%.
- The number of NHS 111 calls offered remains well above levels observed this time last year. Although the 1.67 million calls offered in October was a small decrease on the number offered the month before compared to October 2019 there were 18.8% more calls offered (264,176 more calls).
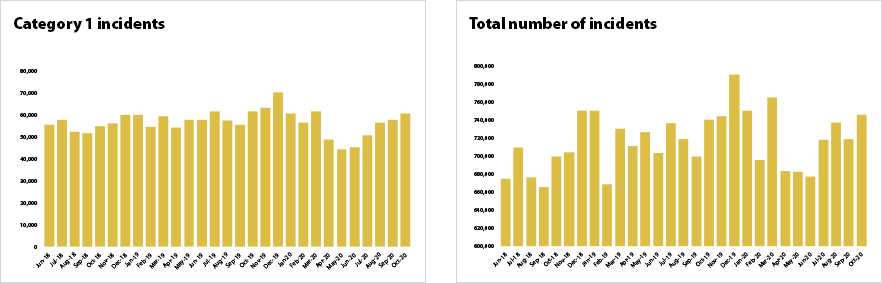
- Ambulance activity continues to increase with more serious incidents than the previous month. There were 745,327 total ambulance incidents in October, an increase of 3.7% since the previous month with Category 1 incidents continuing to increase for the fifth consecutive month.
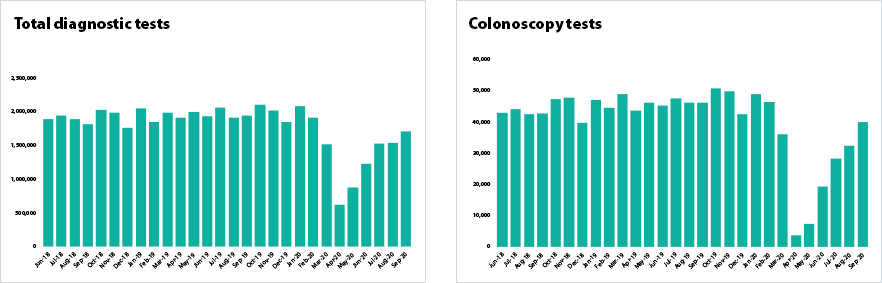
- Diagnostics activity picked up in September but remains 12% below the levels carried out a year ago. 7 million diagnostic tests were carried out in September, an increase of 12% on the previous month after activity had levelled off the previous month. There were some significant improvements in colonoscopy activity with an additional 24% carried out compared to August. There have also been more CT scans completed in September 2020 than in September 2019 showing that the service is doing all it can to recover pre-COVID activity levels.
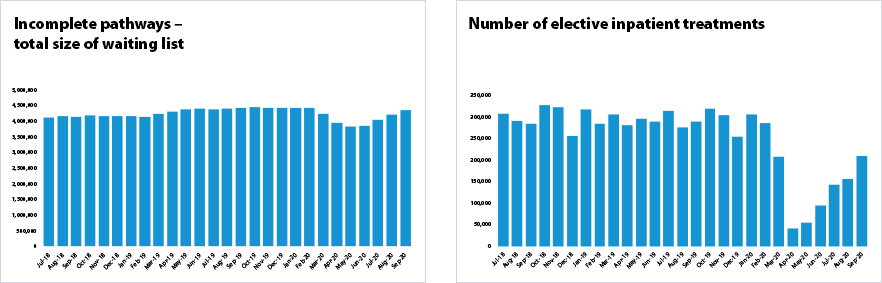
- The number of completed elective care pathways continues to rise. In September the NHS completed 80% of the elective activity it was carrying out in September 2019, therefore meeting the phase 3 target. This included the NHS delivering an additional 55,773 admitted completed pathways and an additional 180,388 non-admitted completed pathways on the previous month – rises of 34.5% and 27% respectively. The number of completed in-patient pathways has increased by 409% since April when the elective care pathway was under the most strain.
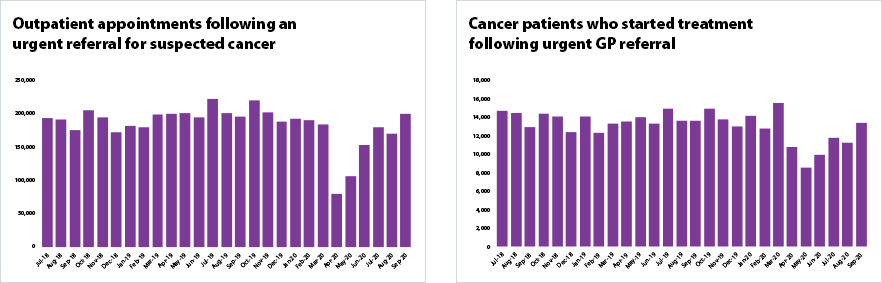
- Cancer activity has picked up significantly from last month and is now similar to pre-pandemic levels. In September there was an 18% increase in the number of people who attended an outpatient appointment following an urgent referral by their GP for suspected cancer (two-week standard) – reaching nearly 200,000. This is also 2% higher than in September 2019. Similarly, there was a 20% increase in the number of patients with cancer who started treatment following receipt of an urgent GP referral for suspected cancer, taking levels to just 1% shy of the activity in September 2019.
- Demand and activity for mental health services remains high. In August 2020, mental health referrals decreased by 10.8% to 302,759 (36,763 fewer referrals) since the previous month but this is still 5% higher than the number of referrals in August 2019. The number of care contacts attended fell in August 2020 to 1,797,935. This is a decrease of 14.2% since the previous month. However, care contacts remain 8.1% higher than in August 2019.
NHS waiting times
- Performance against the 95% A&E standard has slipped by three percentage points to 84.4% in October. In addition, the number of people waiting longer than 12 hours from the decision to admit to admission has nearly tripled, reaching 1,267.
- The number of people waiting over 52 weeks continues to grow but the waiting size is still smaller than it was before the pandemic or at the same time last year. The size of the elective care waiting list increased by 134,769 to 4.35 million, 3.2% since August 2020. But this is still smaller than 4.43 million in February and in September 2019 when it was 4.42.
- As activity increases, performance against the 18 week elective care standard has slightly improved to 60.6%.
- The ambulance services missed both category 1 and 2 time standards. The service missed the category 1 target of 7 mins with a national time of 7 minutes and 29 seconds. This is a deterioration on last month and the worst performance in six months. Average category 2 response times are currently 25 minutes and 21 seconds.
- Waiting times for diagnostic tests are improving. 33% of patients were waiting six weeks or longer, an improvement of five percentage points from last month but a long way off the operational standard of less than 1%.
- Although activity is increasing, performance against key cancer standards slipped, with the sector missing some of the main waiting time standards. 2% of people were seen within two weeks following a suspected cancer referral, missing the 93% standard. Similarly, 94.5% of people started cancer treatment within 31 days following a decision to treat, missing the 96% standard and 74.7% of people started treatment within 62 days following an urgent GP referral, missing the 85% standard.
- Out of area placements (OAPs) began to increase and more people are commencing talking therapies within six weeks from referral. In August 2020, OAPs increased by 14.4% to 675 since the previous month. This is an increase of 19.5% since March 2020 but down by 10.6% since August 2019 when we saw concerted efforts to reduce this figure. In August 2020, 89.1% started Improving Access to Psychological Therapies treatment within 6 weeks, an increase of 1.6 percentage points since the previous month and an improvement of 1.8 percentage points since August 2019.
Our view
Trusts continue to do extremely well in relation to activity levels and are in a better position than they thought they would be at this point of the year in restoring non-COVID services.
Nationally trusts met the ambitious phase 3 targets for September by delivering around 80% of the activity carried out last September. These were stretching targets and it is a huge achievement that providers have managed to step up services at this rate.
The data covering September is very promising. More recent real time information from our members suggests that, as the second wave progresses, the recovery trajectory has slowed and levelled off throughout October. Importantly, however, activity levels are being maintained at September levels, with the data showing trusts are holding current levels of activity despite the increase in COVID-19 patients they are seeing. Of course, we know there is some regional variation, and trusts in the North West, North East and Midlands are working particularly hard with local partners to keep as much elective and outpatient care running as possible
However, the national trend is very promising at this juncture and is testament to the dedication of clinical teams and managers across the country who are doing all they can to ensure they keep services open and running for all those who need treatment.
Diagnostic and elective care
While acknowledging the real urgency of addressing delays reflected in today’s figures, it’s important too to recognise that the NHS has managed to keep a great deal of work on track while dealing with the second spike in COVID-19 cases.
It is really promising to see the continued increases in diagnostic tests and the number of operations. The recent focus by providers and NHS E/I on increasing the number of colonoscopies is reflected in the data and it is really positive to see the number of CT scans is higher than the same time last year. These gains are the result of targeted work and should be recognised as successes.
However, trust leaders remain extremely concerned about the time people are waiting for tests and elective care. Unfortunately, there is another increase in the number of people waiting more than 52 weeks to receive consultant led care. The whole system is working incredibly hard to reduce the elective backlog with increased regional monitoring, sharing of waiting lists, reconfiguring of services and use of the independent sector all being deployed to tackle the problem.
Long waits cause distress and anxiety and tackling them is a top priority for trust leaders. It is particularly concerning that, in some cases, cancer treatment has had to be delayed due to the pandemic. More encouragingly, the waiting list hasn’t ballooned to anywhere near the ‘10 million by October’ figure that some had forecasted. GP activity and referrals have both picked up and trusts are confident that there will not be the previously predicted tsunami of elective patients over winter.
The data published today shows clearly that the NHS has been far from a ‘COVID-19 only service’ throughout and after the first wave. It is clear that non-COVID activity is being restored and positive changes and learning are being locked in across the breadth of the NHS. This is further illustrated in the case studies we are publishing today.
Community services in the pandemic
Due to the lack of nationally available data, it has been harder to track the impact of the pandemic on community services. But we know from our members that, throughout the COVID-19 pandemic, community health services have played a crucial role in delivering essential care in patients’ homes and other community settings, as well as maintaining patient flow to support the wider health and care system.
Despite many pre-pandemic pressures , including increased demand, workforce shortages and funding squeezes, community services quickly adapted to the first wave of COVID-19; for instance, prioritising services in line with national guidance, moving consultations online and implementing new discharge to assess policies to help people get home as quickly and safely as possible and free up hospital bed capacity.
Once the peak of the first wave had passed, community providers set about restoring services as soon as local capacity and resources allowed. Having fully – or almost fully – restored services to pre-pandemic levels, at the same time as providing additional COVID-19 services and managing more complex demand in the community, providers and their staff were feeling the strain. As the second wave of COVID-19 gathers momentum across the country, community providers continue to grapple with a series of competing pressures.
After all these efforts to restore services, community providers now face significant challenges in managing increased demand and competing pressures. Community providers are gearing up for the usual increase in seasonal illnesses as we move into winter and will continue to provide essential support to care homes, the clinically vulnerable and those waiting for elective care.
While we do not currently expect any new national guidance for the prioritisation of community health services, and support this shift to decisions being taken locally based on capacity and local leadership, we can expect that some services may need to be scaled back to manage this latest wave of the pandemic.
Indeed, challenges are already emerging around the implementation of new and more complex discharge requirements; including the need to create designated isolation spaces for COVID-19 positive patients being discharged to care homes.
Furthermore, community providers are taking a leading role in the ambition to roll out a COVID-19 vaccine to all NHS staff before Christmas.
Winter 2020/21
With winter fast approaching, it’s worrying to see early signs of congestion to patient flow including the number of people waiting longer than 12 hours in emergency departments after the decision to admit.
We know the pressures are likely to intensify in the coming weeks as winter makes its mark across the health and care system. The top priorities for the sector over the coming months will be treating COVID-19 patients, reducing the elective long wait backlog, minimising blocks in emergency departments, securing the right mental health services for people in crisis and protecting staff from further burnout.
We also know the acute and community bed base has been significantly impacted by trusts needing to implement COVID-19 and non-COVID areas and social distancing. Furthermore, staffing constraints also limit bed availability and the number of open beds this winter will be subject to the usual localised outbreaks of norovirus which can reduce capacity at a moment’s notice.
All these challenges will require acute, ambulance, mental health and community trusts to work with partners across primary and social care to ensure patients are treated in the most appropriate setting.
It is going to be extremely tough, particularly on frontline staff, many of whom are exhausted and some of them traumatised by their experiences of the pandemic. We owe them so much.
But there is a glimmer of good news as we go into winter. It is looking as if the second wave hasn’t set back the recovery trajectory for non-COVID services as much as had been feared. This is down to the hard work and dedication of trusts over recent months, as illustrated in our case studies below.
NHS activity tracker
Mental health services

Cancer services
Elective care
Diagnostic testing
Urgent and emergency care
Ambulance services
Case studies
Barking, Havering and Redbridge University Hospitals NHS Trust
Alix Holmes, Macmillan information and support manager
Lucy Brooks, Macmillan living with and beyond cancer lead
No part of the NHS (or the world) has remained untouched by the COVID-19 pandemic. However, for our Living with and beyond cancer team, which supports cancer patients through their diagnosis, treatment, and life after treatment, it meant completely reconsidering how they provided their service.
Finding alternative ways to support our patients, other than face-to-face, resulted in phone calls to over 800 patients to see how they were doing. These calls didn’t just occur once - our patients received several calls throughout their treatment and for up to a month afterwards.
These telephone check-ins had such positive feedback from patients that they will continue to be provided, albeit in a slightly more streamlined format.
Alix Holmes, our Macmillan cancer information and support manager, said: “The service was set up to check on patients who were receiving active chemotherapy, some whose treatment was paused or stopped, and for those shielding. We know this was a difficult time for our patients and some were left feeling vulnerable and isolated because they were shielding and unable to have face-to-face appointments with their clinicians.
It was a real team effort as our complementary therapists, alongside Daphne Birmingham, our Macmillan support worker (who only joined us in January) moved to this new way of delivering the service. Some of our patient partners who couldn’t be on site also helped by making calls from home.
We also put together a holistic assessment form which was a lifeline for some people. This helped us to check whether patients were supported while being isolated at home, including practical support for tasks like shopping, emotional support and advice on keeping active under the current COVID-19 guidelines. We also signposted patients to appropriate services within our trust and the community.
Our complementary therapists even made up support packs to help patients manage side effects from their treatment, including relaxation leaflets and aromatherapy sticks, which were hugely valued by our patients.
With complementary therapy now restarted and more face-to-face patient support and care being provided, the telephone support service will continue to run in a more efficient and sustainable format. This means all patients on chemotherapy will now get a call after their first course of treatment, another call around half-way through their treatment and a holistic needs assessment via the telephone once they’ve finished their course of treatment. This is something we wouldn’t have thought possible before the pandemic."
The Living with and beyond cancer team have also had to look at innovative ways of providing other aspects of their service, including workshops and events for patients which have always attracted high attendance. These include our EMPOWER programme (a health and wellbeing event for those newly diagnosed with cancer), quarterly post-treatment events, Look good, feel better make-up masterclasses, and the HOPE programme (a six-week resilience course following treatment).
Our Macmillan Living with and beyond cancer lead Lucy Brooks, said: “Initially everything had to grind to a halt when COVID-19 hit and while our patients were really understanding, we wanted to find new ways to support them.
We have held a couple of Look good, feel better sessions virtually and have also filmed our EMPOWER programme with our medical photography team. We plan to share this with patients via a link, so they don’t lose out during the pandemic. We’re also planning to film the information talks covered in our post-treatment event. In each case, there will be a virtual event set up to allow people to ask questions and meet each other online. We had planned to launch a carers’ support group when the pandemic started but, instead, we’re hoping to get a group up and running via Microsoft Teams. “
Alix and support worker Daphne also provide support and advice to patients and their families on any aspects related to living with and beyond cancer. This was something they’ve been able to continue to provide over the phone and email during the pandemic.
Lucy added: "We’re hoping that by filming some of our sessions and sharing these with our patients, we may actually be able to reach more people as they don’t have to take the time out to attend in person.
It’s been a really interesting time, especially in how we’ve found lots of ways to do things differently. We’re looking forward to the launch of the virtual EMPOWER sessions next month."
East Sussex Healthcare NHS Trust
Karen Poole, consultant therapist (rehabilitation)
At East Sussex Healthcare NHS Trust, our aim has always been to provide the best possible care to our patients, whether this is in our hospitals or in a community setting such as in a patient home. As the COVID-19 pandemic developed and the restrictions came into play, we were faced with the challenge of how we delivered the same excellent care for our patients under the new government guidelines.
Although we already had a quality improvement process underway for our rehabilitation pathways prior to the pandemic, the pandemic allowed us to adapt our processes and redesign our pathways for the better by looking at them through a new lens. This meant working in an iterative and collaborative way to tackle future capacity challenges effectively to support our patients in the best way possible.
At the start of the pandemic, our existing rehabilitation stratification tool, which allowed us to map, measure and understand community rehabilitation within the East Sussex area, was redesigned to take into account the new COVID-19 challenges we faced. This meant that we could use it to help colleagues better manage complex patients within the system while also upholding care for patients with the lowest rehabilitation needs.
The tool allowed us to shift clinical dependence and complexity along the pathway by redeploying our allied health professional workforce in an innovative way. This allowed us to move our staff from the musculoskeletal outpatient service, which had largely shut down during the early COVID-19 crisis, to our bedded rehabilitation units and community pathways. It also enabled us to have clinical oversight and embed a regional sitrep for specialist rehabilitation. The tool has helped us to transform the care that we provide by increasing patient access and has given staff the confidence to decide whether patients need to be moved on to the next stage of the pathway. It has also improved system flow and reduced excess bed days while in turn increasing staff morale.
At the peak of the pandemic, we saw an emergence of patients with more complex disability management requirements within the region. This was often due to care being paused and a lack of accessibility to definitive services during the lockdown period. In response to this we implemented the multi-agency multi-disciplinary team (MDT) approach where colleagues from different areas of care such as primary, secondary and social care and tertiary agencies could refer a complex patient to a virtual MDT via a direct email address. The system also has the ability to log patient records and the various clinical decisions that have been made across the different agencies in one space. This new system has helped to manage patient handovers effectively and has improved multi-agency collaboration with a single shared purpose of improving the patient’s health and wellbeing.
We also introduced a new rehabilitation advice line which was initially used to serve our patients who had been discharged home with low level rehabilitation needs during the height of the pandemic. The service was offered through the community stroke team where patients could call for advice specific to their condition five days a week. This reduced the demand on acute colleagues and provided vital support for our patients when they needed it the most. The service has since expanded to the musculoskeletal (MSK) service team and the podiatry team. The MSK team use the service to help patients manage mild to moderate back pain whereas the podiatry team use the service alongside their self-made YouTube videos to support patients in foot self-care while at home. To ensure that patients are supported by the right approach, each service also has an embedded virtual triage process.
The rehabilitation advice line is now in the process of being expanded towards a self-supported pathway, where every patient that comes through the system will have access to the advice line. This means there will be a single point of contact for each pathway, a COVID-19 screening tool, and a dedicated rehabilitation page on the trust website where patients can get advice specific to their condition.
We have also implemented the rehab recovery forum which allowed colleagues across the patch to come together virtually and discuss what has worked well, what hasn’t and what steps can be taken in the future to improve the service. Using quality improvement methodology and a real collaborative approach, we were able to successfully upscale the changes that we had made during the first wave of the pandemic into this new phase and hope to do the same for the future.
While services have bounced back, we are keen to retain much of the learning through the pandemic to support different ways of managing patients at every rehabilitation level, from those with lower level needs to patients with the most complex disabilities. The changes we have made and implemented during the period wouldn’t have been possible without our hard-working staff who have adapted in the hardest of times while always putting patients first, so we would like to take this opportunity to thank them for their dedication and effort.
Frimley Health NHS Foundation Trust
Neil Dardis, chief executive
Frimley Health NHS Foundation Trust (FHFT) admitted its first COVID-19 patient on 26 February. From this point on, COVID-19 activity built rapidly, and, at the height of the crisis, there were 394 COVID-19 positive patients being treated across the trust. Along with many other providers, FHFT rapidly scaled back its planned care activity in order to support the management of COVID-19 patients and by mid-March the trust was only treating the most urgent planned care patients.
From very early on in the pandemic, the trust was considering how best it could serve its most vulnerable patient groups and in particular patients who were receiving, or needed to receive, care for cancer. The potential for physical and mental harm in this group of patients from delays in diagnosis and treatment was significant.
The trust continued to provide outpatient chemotherapy for our patients throughout the pandemic period, but it was recognised that the location of this treatment, based as it was on the trusts’ two acute sites, was not the safest option available. Thanks to the efforts of our staff and the staff of a local independent sector provider, the trusts two chemotherapy units were successfully combined and relocated onto the site of the local independent sector provider. This allowed for an isolated COVID-19 secure environment to be created with a dedicated group of staff who had been tested for the virus. This new centre opened on 12 April and has since treated over 2,700 patients. The majority of patients have therefore continued to receive neo-adjuvant and adjuvant chemotherapy in line with national guidelines. Following national guidelines, a number of patients received modified less immunosuppressive-intensive regimens. Patient feedback for the new service has been extremely positive, with patients satisfied with the service and facilities provided at the new location, and happy that they were still being treated by the same staff.
While the trust continued to treat patients requiring urgent (priority 1) planned care, many patients who required surgery for cancer were having their surgery delayed. The trust worked rapidly through the peak of the pandemic to develop dedicated and protected ‘green’ surgical pathways in order to allow the majority of cancer surgery to restart. A 'green' surgical hub was created utilising what was originally a day case area in order to allow patients requiring inpatient colorectal, renal and gynaecological cancer surgery to be managed safely with extended PACU and critical care support as required. Colorectal and gynaecological surgery was combined from both acute sites into this one planned care area, with all patients prioritised following the Royal College of Surgeons guidelines for surgical prioritisation during the coronavirus pandemic. This unit was opened on 12 May, and on 18 May a second ‘green’ elective surgical area was opened at the trust’s non-acute site at Heatherwood Hospital to manage day case patients. Patients were asked to self-isolate and were then tested for the virus before admission, while staff were cohorted to these ‘green’ areas and also regularly tested for COVID-19. We were able to run these isolated ‘green’ sites safely throughout the height of the pandemic until the government guidelines around infection prevention and control around planned care at the end of the first peak were relaxed.
Thanks to the efforts of our staff we actually saw unexpected benefits from combining colorectal and renal cancer services on the single site, with a significant reduction in mean length of stay over the period. Cancer referrals dropped significantly during the peak of the pandemic but have now recovered to pre-pandemic levels.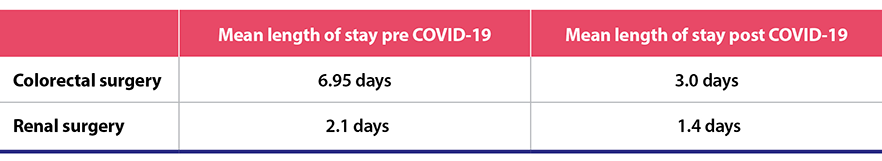
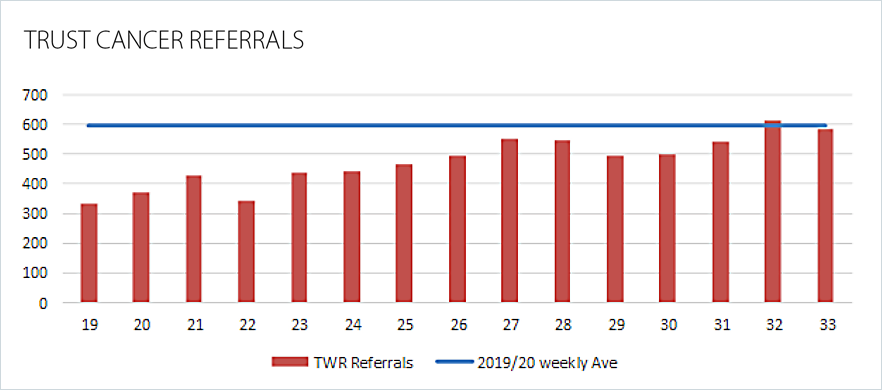
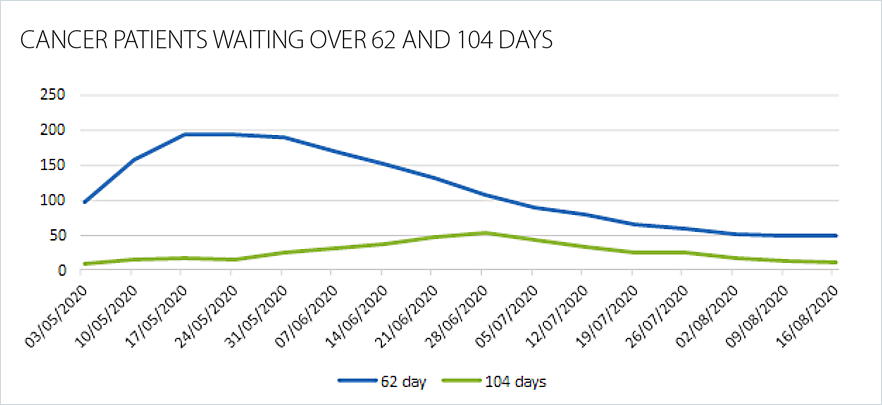
As a result of the virus, the reduction in planned care activity led to a significant rise in the number of patients experiencing waits of over 62 and 104 days. This is especially true compared to usual trust performance which has consistently met the 62 and 104 day performance targets. The majority of the waits were associated with patients choosing to delay their care along with reduced access to diagnostic procedures such as endoscopy. The introduction of an innovative pathway in colorectal surgery with the application of the FIT test across the integrated care system (ICS) has allowed the prioritisation of patients and reduced waiting times. Performance is returning rapidly to base line for both diagnostics and treatment across all cancer pathways.
Throughout the pandemic, our staff have continued to work enormously hard and in innovative ways to ensure that our patients have been able to access the care that they need with as little delay as possible. Our patients have also proven to be extremely resilient, accepting changes in practice around isolation, understanding the need for virus testing, visiting limitations and delays in non-urgent care while also being open to the relocation of services, and embracing virtual outpatient appointment.
Modality LLP
Dr Naresh Rati, executive partner
The COVID-19 pandemic led Modality LLP to rapidly redesign the way in which dermatology outpatient services were provided, enabling routine outpatient care to continue safely and effectively using video, photographic and telephone consultations. Modality provides up to 20,000 dermatology consultations each year for patients registered across 150 GP practices, on behalf of hospital providers and clinical commissioning groups (CCGs). Prior to the pandemic, only 5-10% of dermatology appointments were provided digitally, by video or telephone consultation. From March 2020, however, 100% of dermatology cases were initially assessed by telephone or video consultation. This ensured that service provision continued safely during the initial lockdown period.
An analysis of data from 1,034 consultations over March and April 2020 revealed that 50% of first outpatient consultations were successfully assessed, diagnosed and discharged following an initial telephone, photographic or video consultation. 49% of patients required a face-to-face review appointment and the remaining 1% were managed by a follow up telephone/video consultation.
The 50% of patients discharged at the first outpatient consultation were diagnosed with benign lesions or skin rashes and did not require further follow up. Patients were suitably reassured by the specialist without the need to be subsequently seen.
Better use of digital technology has not only meant care has continued to be delivered for patients but has also improved convenience for patients resulting in reduced ‘did not attend’ (DNA) rates. Prior to the introduction of the ‘digital first’ model, the average DNA rate within the service was 19%. This has steadily decreased as the new model has been embedded, with the current DNA rate now averaging at 8%, reducing the number of missed NHS outpatient appointments.
This use of technology has helped ensure continuity of routine outpatient care while minimising unnecessary face-to-face encounters and has provided a safe and convenient approach to appointments for many patients. Furthermore, this service redesign has demonstrated the key role technology can play in effectively managing a substantial proportion of the outpatient caseload during and post COVID-19.
The learnings from dermatology have been applied across other specialty areas delivered by Modality LLP ensuring that outpatient care can continue safely throughout the COVID-19 pandemic with patients receiving early diagnosis and treatment of their conditions.
Moorfields Eye Hospital NHS Foundation Trust
Louisa Wickham, consultant ophthalmic surgeon
Amid the pandemic, Moorfields Eye Hospital NHS Foundation Trust has had to adapt in order to provide essential eye treatment services to its many patients. We’ve done this by holding an innovative ‘cataract drive’, which enabled us to deliver more than four times the usual number of cataract operations. This helped us clear out our surgical waiting lists, which have been significantly affected by COVID-19. After a number of successful pilots, we were able to safely offer many more patients the chance to have this surgery without further delay.
The cataract drive started on 14 September and was the first of its kind in the UK. Eight operating theatres at Moorfields provided 725 cataract procedures in six days. This is significantly more than our weekly average of around 120 cataract procedures.
To make this possible, theatres at Moorfields Private Hospital only provided emergency surgeries that week to free up more theatre space. We were able to hold so many pre-operative assessments in such a short space of time by having several dedicated Saturday clinics. The process for day surgery was also adapted so that patients spent just over an hour on site, with staggered arrival times throughout the day. All patients were COVID-19 tested and instructed to self-isolate prior to their procedure and all staff were also tested regularly.
The cataract drive needed a great deal of planning. We had to rethink how we do almost everything to make this possible and I am incredibly proud of the adaptability and creativity of staff at Moorfields. We are delighted to have helped so many of our patients in such a short time and hope that this project could be an example to the rest of the NHS as a new way to clear waiting lists in the wake of COVID-19.
This project was supported by over 80 volunteers covering nearly 200 shifts kindly provided by St John Ambulance. The trained first aiders assisted patients through every step of their surgery, including helping with pre-operative assessments, accompanying and reassuring them during their surgery, and assisting with their discharge. The project was also supported by long-standing industry partner Alcon, who provided intraocular lenses, equipment and technical service support.
One of our patients on the cataract drive, Brenda , said: "I am delighted that I got to have my cataract surgery as part of the Moorfields cataract drive as it has allowed me to get back to doing everything I enjoy, with no further delay. Our sight is something we should never take for granted and I am grateful to Moorfields for continuing to help patients like me during these strange times."
Moorfields provides care for many other conditions besides cataract, and we have made adaptations throughout the entire trust to restore our services safely. These measures include following or exceeding all national guidelines, giving all patients and staff face masks to wear on site (unless exempt), a one-way system in corridors and reduced capacity in waiting rooms to allow social distancing, alongside plastic protective screens at all reception desks.
We look forward to hearing from other trusts who are planning to apply our cataract drive model in more settings and specialties across the NHS and hope that it can help many more people to be treated without further delay.
Royal Surrey NHS Foundation Trust
Jane Fagan, associate director of operations, adult community services
As an integrated care trust, providing acute and community healthcare services, we were faced with the task of changing our care models at a rapid pace under the growing pressures of COVID-19. This is something that we didn’t think would be possible at such a pace. However, the quick thinking, willingness and commitment of our staff and the understanding of patients and the public have enabled us to implement and embrace such change.
One of the first changes we made due to the social distancing restrictions was to move some of our services that were once face-to-face to virtual. Community speech and language therapy and musculoskeletal (MSK) rehabilitation services embraced virtual appointments using Attend anywhere software, enabling patients to still get the care that they needed. The new mode of care was well received by our patients and staff alike.
The pandemic led to the national mandate to implement the discharge to assess (D2A) process. This was already in place in our system but the new national guidance acted as a positive catalyst to this work, which ensures patients who no longer need to be in an inpatient bed are discharged home, and only those suitable for a rehabilitation inpatient stay would be admitted to a community hospital. Once at home, our therapy staff would assess patients and provide the care that they needed in their own homes. This meant patients could stay safe at home with their families while continuing to receive essential care and rehabilitation. By driving the D2A process early on in the pandemic, we more than doubled the number of patients going home and our system had one of the lowest number of medically fit for discharge patients in inpatient beds.
The success of D2A was also due to there being a reorganisation of staff whereby more care workers and therapists were assigned to provide assessments and care at home rather than on site. While the pandemic allowed for us to put these processes in place in a way and at a speed that we didn’t think would be possible, we plan to make our processes more efficient and seamless in the future, so we are now taking a quality improvement approach to do so.
We changed the medical model at one of our community sites, Milford, to be led by acute geriatricians and we enhanced the level of acuity at the site. This meant that nursing staff that had spent a number of years working in frailty and rehabilitation care were quickly trained to take on more acute work. This included delivery of IV antibiotics, blood transfusions and oxygen therapy from our newly added oxygen concentrators in our community site.
Re-defining Milford beds to acute beds allowed us to minimise the number of people at our main site. This enabled us to continue our elective cancer work and we cleared our robotic prostate surgery backlog during this time.
We also expanded the hours of our minor injuries unit, so that we could see more complex cases with the help of our orthopaedic surgeons, who were redeployed to support the unit as they had stopped elective work during the COVID-19 crisis.
Louise Stead, chief executive at Royal Surrey NHS Foundation Trust said: “During the first wave of the COVID-19 pandemic we saw, not for the first time, the fantastic benefits of being an integrated Trust able to deploy acute and community teams to suit the needs of our patients. I am incredibly proud of all of our staff and the way they have adapted to what was required of them in unprecedented times.”
South West Yorkshire Partnership NHS Foundation Trust
Gill Stansfield, deputy director of operations
This has been a year unlike any other for the NHS. Our teams have had to work hard in the face of the additional challenges brought by COVID-19 to deliver the same high-standard of service that ensures people stay well in their communities. The way we work has changed dramatically throughout 2020, and in many cases, this has had positive outcomes.
In Barnsley community service, our teams made nearly 5,000 essential home visits providing a variety of care and treatments to vulnerable patients. They also carried out around 10,500 telephone/video consultations, recorded 2,500 patient interactions on our stroke and neurological rehabilitation units and held more than 50 management meetings – all in the space of a week.
Our teams also stepped up to support each other in busy times. When schools closed, the trust’s school immunisation team, who work tirelessly to consistently achieve high levels of uptake for all school vaccination programmes, were re-deployed to support the neighbourhood nursing teams.
With fewer people being detained by police, our liaison and diversion staff found that they had capacity to support colleagues on the front line. They turned their hand to making PPE kits and completed refresher training to work in a completely different role in the district nursing team.
Digital communication has been essential for many people throughout the pandemic, and it became a lifeline for many of our service users too. Our virtual visitor scheme enables inpatients on the trust’s mental health units to stay in touch with their friends, family and loved ones by using technology such as Zoom. Zoom has enabled service users to see and speak to their nearest and dearest while visiting on wards was restricted to minimise the spread of the virus.
The trust has also introduced Cards of kindness, which help friends and family of inpatients to send messages to loved ones on wards. By simply filling in an online form, friends and family can send a personalised message which is printed out and delivered safely to the ward within a couple of days.
We also introduced a new feature into our patient record system which allowed electronic prescribing and administration of medications (EPMA). This enabled us to prescribe, supply and administer medicines electronically and brought a significant range of safety, quality and financial benefits. Our paper drug charts have been replaced with electronic processes in our patient record system, meaning we have complete records that can be accessed remotely.
Unfortunately, but understandably, the coronavirus pandemic has had a huge impact on people’s mental health. With an even bigger focus on keeping ourselves mentally, physically and emotionally well, it’s important that the right support is there for people to access quickly and easily. Our recovery colleges in Barnsley, Calderdale and Kirklees, and Wakefield launched brand new websites this year. They offer courses and workshops designed and delivered by professionals and people with real life experience with the aim of supporting recovery, increasing knowledge and skills, and expanding interests.
We’re currently carrying out a project to look at the successful changes we have made and how we can take these forward. Coronavirus has changed our lives in many ways but our staff’s endless passion for caring, helping, and making a difference has remained the same.
Press statement
Once again trusts are rising to the challenge
Responding to the latest monthly combined performance data from NHS England and Improvement, NHS Providers chief executive, Chris Hopson said:
"With the milestone of 50,000 COVID-related deaths this week, no one should be in any doubt about the scale of the challenges trusts and frontline staff face as they deal with renewed COVID-19 pressures and work to restore services disrupted by the pandemic.
"Trust leaders are keenly aware of the inconvenience, anxiety and distress for patients caused by any delays for diagnostic tests, treatment or consultations.
"“But what we see in these figures is real evidence that once again the NHS is responding in extraordinarily difficult circumstances to provide the best possible care for patients, COVID-19 and non-COVID.
"Despite dealing with the second wave of the virus, trusts managed to meet the ambitious target for routine planned operations in September, reaching 80% of last year’s levels. That’s an extraordinary achievement.
"Trusts tell us they are determined to keep as much of this work going as possible, and we see no sign of waiting lists spiralling up to 10 million by October, as some predicted.
"With winter fast approaching, it’s worrying to see the number of people waiting longer than 12 hours in emergency departments before being admitted is beginning to rise.
"It’s important for the public to understand that the NHS was, is and never will be a COVID-19 only service. If people have concerns they should seek help.
"We know the pressures are likely to intensify in the coming weeks as winter makes its mark across the health and care system. This will require acute, ambulance, mental health and community trusts to work with partners across primary and social care to ensure patients are treated in the most appropriate setting.
"It is going to be extremely tough, particularly on frontline staff, many of whom are exhausted and some of them traumatised by their experiences of the pandemic. We owe them so much.
"But while acknowledging the real urgency of addressing delays reflected in these figures, it’s important too to recognise that the NHS has managed to keep a great deal of work on track while dealing with the second spike in COVID-19 cases.
"Today we highlight seven case studies from a range of settings that exemplify the ingenuity, skills and commitment of trusts and frontline staff in the final edition of our NHS activity tracker."