
Introduction
As winter fast approaches and COVID-19 pressures continue, the NHS is preparing for the months ahead. Many trust leaders have noted their concerns around potential rises in COVID-19 cases alongside seasonal infections, as well as concerns about capacity to meet demand over the coming months.
The statistics published today highlight an extremely busy month with increases in activity in many parts of the service. Significant pressures have been felt in many clinical areas, particularly in the urgent and emergency care pathway which saw record numbers of category 1 incidents.
This month's performance figures
Each month, NHS England and NHS Improvement publish statistics looking at activity and performance across a range of services including urgent and emergency care, routine care, cancer, and mental health. Below we set out the latest trend for each clinical area.
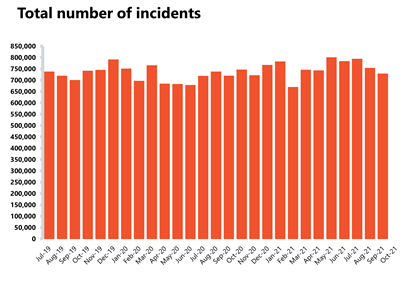
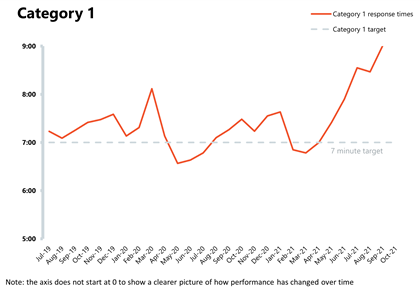
NHS 111 and ambulance: Ambulance category 1 incidents continue to rise as they reach the highest levels since records began. This highlights the increased demand and pressures across the urgent and emergency care pathway.
- Ambulance category 1 incidents (those requiring immediate intervention and resuscitation) increased by 7.9% to 82,129 since the previous month (6,006 more incidents). Compared to two years ago, incidents have increased by 33.4% which underlines the increase in demand pressures on frontline ambulance staff.
- The ambulance service has missed the average response time target of seven minutes for category 1 calls for the sixth consecutive month at 9 minutes, 20 seconds. The average response time for category 2 calls also deteriorated further, missing the 18 minutes target at 53 minutes, 54 seconds.
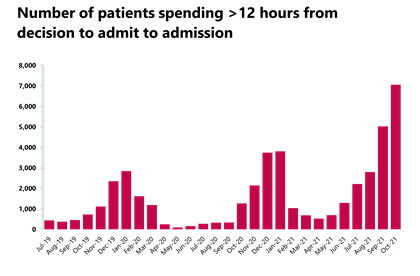
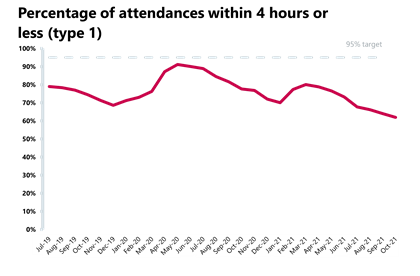
A&E and emergency care: activity across emergency departments increased this month but remains around or below levels seen before the pandemic. Performance against national targets continued to deteriorate, with the service registering the worst performance on record.
- In October 2021, there were 2.17 million A&E attendances, an increase of 1.8% from the previous month and very similar (-0.1%) to two years ago before the pandemic.
- There were 517,062 emergency admissions in October 2021, a small increase of 2% from the previous month but lower (-8.2%) than two years ago before the pandemic.
- Performance against the 95% target dropped again (1.3 percent points) to 73.9%, representing the worst performance on record.
- The number of patients waiting for longer than four hours has increased by 15.6% from the previous month and the number of patients waiting for more than 12 hours has also increased by 40.5%.
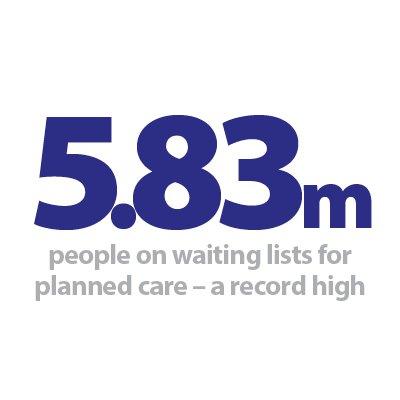
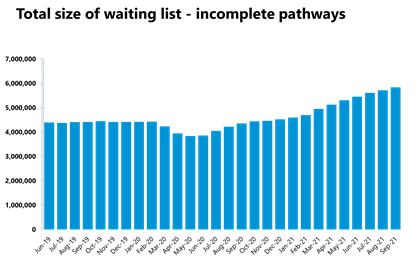
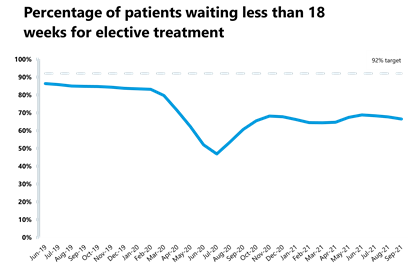
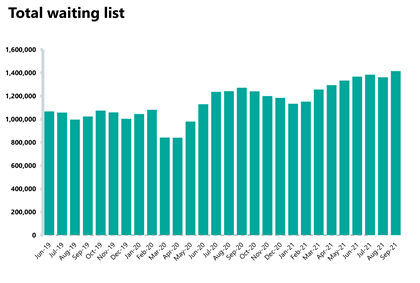
Elective care: referrals continue to outstrip activity as the waiting list has grown again in September 2021, reaching a record high of 5.83 million. This month, the number of patients waiting for longer than 18 and 52 weeks has also increased.
- In September 2021 the size of the elective care waiting list increased by 2.1% (118,723 more) to 5.83 million since August 2021. This is the highest level seen in the current records over the last decade.
- The number of patients waiting more than 18 weeks increased by 5.6%, meaning that performance against the 18 weeks standard worsened, falling by 1.1 percentage points to 66.5%
- The number of people waiting over 52 weeks has increased in September 2021 as well, after a few months of decreasing figures. The number of long waits grew by 8,428 to 300,566, representing an increase of 2.9% from August 2021, and an increase of 115% from last year.
- Inpatient elective care activity has increased in September 2021 from the previous month, with the number of admitted inpatient pathways increasing by 8.9%, meaning that a total of 252,699 inpatient treatments were carried out.
- Non admitted pathways also increased, with the NHS delivering 1,038,803 elective non-admitted pathways – an increase of 14.8% on the previous month.
- There were 1.62 million new RTT pathways in September, representing an increase from 1.47 million in the previous month.
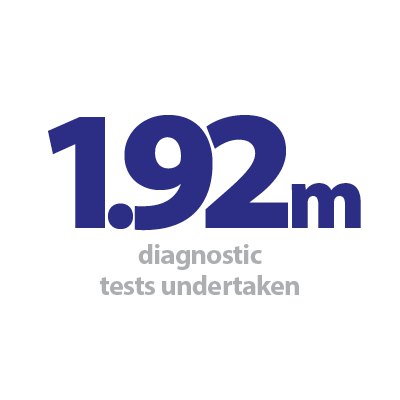
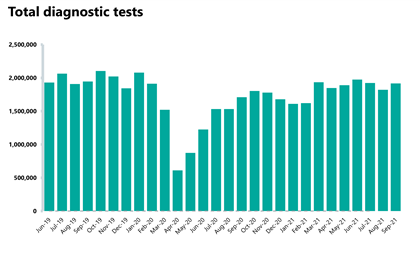
Diagnostics: diagnostic activity increased in September 2021 and remains slightly below pre-pandemic levels. However, the waiting list has increased and is at an all-time high.
- The number of tests carried out in September 2021 has increased by 5.3% to 1.92 million (95,828 more) compared to August 2021. Compared to two years ago before the pandemic, total activity has decreased slightly by 1.4%, with 27,371 fewer tests carried out.
- Compared to last year, the number of MRI, CT and colonoscopy tests all increased by 14.5%, 9.6% and 21%, respectively. When looking at diagnostic activity from September 2019, before the pandemic, the number of MRI tests is down by 1.7% (5,338 fewer); however, the number of CT and colonoscopy tests have both increased by 10% and 4.6%, respectively.
- The diagnostic waiting list has increased by approximately 4% to 1.41 million (53,705 more) since the previous month, with 26.1% of people waiting six weeks or more for a test in September. This figure is slightly down from 27.1% last month and is again missing the 1% target.
Cancer: performance against the waiting time standards continued to deteriorate and the NHS is missing all key national targets; however, activity is higher than pre-pandemic levels.
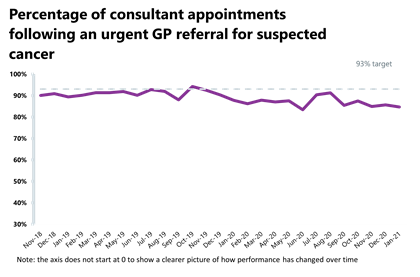
- A total of 231,421 people were seen within two weeks from an urgent referral for a suspected cancer pathway; this is an increase of 9.7% (20,490 more consultant appointments) compared to the previous month. This figure is 15.8% greater than the same time last year and 18.6% higher than two years ago, before the pandemic. 84.1% of urgent GP referrals were seen within two weeks, a slight decrease in performance from the previous month (84.7%) and missing the 93% standard.
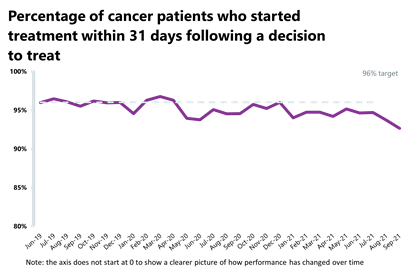
- In September 2021, 27,342 people completed the 31-day pathway, which aims to start treatment within one month from the decision to treat. This was 1,542 more people than the previous month – an increase of 6%. Activity has increased from both one year ago (11.9% higher) and two years ago, before the pandemic (6.8% higher). 92.64% of people started treatment within one month of the decision to treat, a decrease in performance compared to the previous month (93.7%) and missing the 96% standard.
- The number of people who completed the 62-day wait from urgent GP referral to starting their first cancer treatment pathway increased compared to the last month. 14,866 people completed this pathway, an increase of 6.7% (939 more people) from the previous month. This has also increased compared to one year ago (10.8% higher) and two years ago, before the pandemic (9.5% higher). Performance this month for the 62-day wait is at 68%, a decrease from the previous month (70.7%) and also missing the 85% standard.
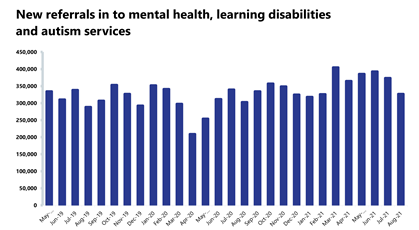
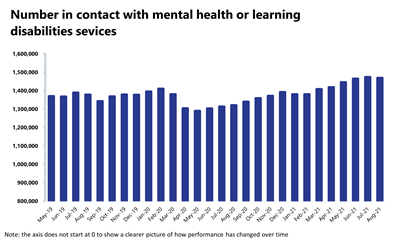
Mental health: the number of people in contact with mental health services has fallen this month, but levels still remain high.
- In August 2021, mental health referrals fell by 12.5% to 326,896 (46,608 fewer referrals). Compared to a year ago, referrals have increased by 8% (24,137 more referrals than August 2020). In comparison to two years ago, referrals have increased by 13.4% (38,533 more referrals than August 2019).
- The number of people in contact with mental health services has fallen slightly by 0.3% to 1,469,187 since the previous month (4,004 fewer people in contact). However, levels remain high, registering the second highest number of people in contact since records began. Compared to a year ago, there are 11.2% more people in contact with mental health services (148,446 more people in contact). In comparison to two years ago, there are 6.6% more people in contact (91,228 more people).
- There were 1.84 million care contacts attended (down by 10.6% and 217,711 fewer than the previous month). In comparison to the same time last year, care contacts have increased by 2.6% (46,843 more). Compared to two years ago, there are 10.9% more care contacts (181,145 more).
- In August 2021, the number of out of area placements decreased to 690 (40 fewer OAPs than last month). Compared to a year ago, OAPs have gone up by 15. Compared to two years ago, there were 65 fewer OAPs.
Our view
This month's data highlight one more time how NHS staff are working diligently across physical and mental health services, doing their utmost to balance COVID-19 pressures with increased demand for non-COVID care. As we head into the winter months, trusts are facing a challenging time ahead with increasing pressures across the service.
Similarly to last month, the urgent and emergency care pathway remained extremely busy, registering record numbers for category 1 incidents and increased A&E attendances and emergency admissions. Trust leaders have expressed their concerns about capacity to meet demand and, if these emergency care demands increase further throughout winter, the high risk of elective care being compromised. Winter will also bring the expected seasonal flu, norovirus and anticipated increases in respiratory syncytial virus infections (particularly among children), which represent unpredictable demand pressures alongside potential rises in COVID-19 cases.
This month's data also showed activity increases in diagnostic testing and elective care. Equally, cancer activity remains higher than pre-pandemic levels and more people were being seen for treatment this month. These remarkable achievements are a true testament to the work of NHS frontline staff. However, the number of patients waiting for their treatment to start keeps growing to worrying levels.
As always, NHS staff continue to work tirelessly but the ongoing COVID-19 pressures, staff shortages and the care backlog remain significant challenges, ahead of what will no doubt be a very difficult winter.
Wirral University Teaching Hospital NHS Foundation Trust
Dr Nikki Stevenson, medical director and deputy chief executive at Wirral University Teaching Hospital
Dr Nikki Stevenson discusses how Wirral University Teaching Hospital NHS Foundation Trust has a new trial in their A&E department at Arrowe Park Hospital, potentially enabling people to receive care faster and closer to home, if they do not need emergency care.
We launched a pilot on 25 October which sees a change to the way patients who attend our A&E at Arrowe Park Hospital are cared for, potentially enabling them to be treated faster and closer to home.
Any patient attending A&E who needs emergency treatment will still receive it, however, under the new pilot, anyone attending whose care is not an emergency could be directed to an alternative service in the community more appropriate for their care, and where it is safe to do so. They could be directed to an appropriate service such as an urgent care centre, walk-in centre, minor injury unit, a local GP or a local pharmacy. The pilot builds on the national NHS 111 First campaign which was launched in December 2020 and aims to ensure patients are seen in the right healthcare setting at the right time.
As is the case nationally, our A&E in Wirral has seen an increase in patients arriving compared to before the COVID-19 pandemic. In the first eight months of 2019, there were 59,599 people attending A&E. This compares to the same period of 2021, where there were 62,385 attendances. This is an additional 2,786 attendances, which is a 5% increase. Many of those attendances were not emergencies. If this trend continues over this year, there could be 4,000 additional attendances compared to 2019.
One of the major benefits of the pilot is expected to be a significantly improved patient experience. The experiences of our patients are a top priority, and we are undertaking this pilot to ensure we are providing the highest possible standard of care to those coming to our hospitals for emergency treatment.
Crucially it is also expected to reduce long unnecessary waits in A&E. The range and breadth of high-quality health care services available to people across Wirral is considerable and while we understand people are often anxious to be seen quickly when they do attend A&E, it is often the case that they could be seen more appropriately, and considerably more quickly, elsewhere. This initiative will also enable emergency care teams to focus on patients who attend with an emergency.
Another significant benefit of the scheme is how it will ensure social distancing is maintained in the A&E waiting area, keeping urgent patients and staff safer from the spread of COVID-19 and other infections.
We also want to reassure our local community that if they have an emergency, we are open and are here to care for them. In an emergency, people should always still call 999 or come to emergency departments. Where people need to access NHS services, but their need is not an emergency we would urge people to contact 111 online in the first instance and allow the experienced call-handlers to direct them to the best service for their care.
A&E
Cancer
RTT
Diagnostic tests
Ambulance indicators
Mental health
Press release
NHS steps up but pressures intensify with winter on the way
Responding to the latest monthly combined performance data from NHS England and NHS Improvement, the deputy chief executive of NHS Providers, Saffron Cordery said:
"These figures underline in stark detail why trust leaders are increasingly concerned about winter approaching, with pressures set to intensify.
"This is being felt right across the health and care system including hospitals, community, mental health services and primary care.
"Ambulances services are operating at the edge of their limits, with record numbers of 999 calls answered in October for the most seriously ill patients. Emergency departments are coming under considerable strain with a record 1.42 million people being treated in October.
"The human impact of these pressures is a huge cause of concern for trust leaders. While it is positive that diagnostic tests and cancer referrals are both up compared to this time last year, the significant rise in the number of patients waiting over two years for their treatment to start, with waiting lists for planned surgery now hitting 5.8 million, is very worrying.
"NHS staff continue to go above and beyond, but chronic staff shortages, the ongoing threat of COVID-19, and the significant care backlog are ramping up the pressures on the health and care system.
"Trust leaders are also concerned about the crisis in social care, which the government must focus on to ensure vulnerable people are kept well and able to return home safely with support after treatment.
"The NHS is running hot already, ahead of what is expected to be an extremely difficult winter."