

Our analysis
Introduction
This week England took a further step along the road to end COVID-19 lockdown restrictions, with the opening of non-essential shops, hairdressers, and places to eat. Other changes include being allowed to meet outside in groups of six. The easing of restrictions was taken after the government agreed that its tests, including COVID-19 pressure in hospitals, were met and trends were continuing in the right direction.
The most recent data does show a picture of reducing COVID-19 pressure in hospitals. The total number of people in hospital with COVID-19 is reducing each day. As of 14 April, there were 1,972 people in hospitals across England with COVID-19 - 94% fewer people than at the peak of 34,000 in January.
Similarly, the number of people in intensive care is continuing to decline, with the latest data showing 315 people in mechanical ventilation beds across England. Deaths from COVID-19 have also fallen, with the rolling daily average over the past week equalling 28 deaths per day. We have been tracking the COVID-19 trends in our daily dashboard.
The most recent data does show a picture of reducing COVID-19 pressure in hospitals. The total number of people in hospital with COVID-19 is reducing each day.
One key contributing factor to the reduction in community transmission and the subsequent decrease of pressure in hospitals, is the ongoing successful rollout of the vaccination programme. This week the government met its target to offer all priority groups 1 to 9 a vaccine, meaning people under 50 are being offered the vaccine earlier than planned. To date, nearly 34 million vaccine doses have been administered, comprising 27.1 million first doses and 6.7 million second doses.
Against this backdrop, today’s NHS activity figures highlight a major concern for trust leaders across ambulance, acute, community and mental health services – the mounting backlog of care spanning physical and mental health services. This month, our NHS activity tracker demonstrates the significant gains trusts have been making by increasing their activity levels over February and March, an impressive feat when taking the COVID-19 pressures into account.
Today’s NHS activity figures highlight a major concern for trust leaders across ambulance, acute, community and mental health services – the mounting backlog of care spanning physical and mental health services.
This month’s performance figures
Each month NHS England and NHS Improvement publish statistics looking at activity and performance across a range of services including urgent and emergency care, routine care, cancer, and mental health. Below we set out the latest trend for each clinical area:
NHS 111 and ambulance:
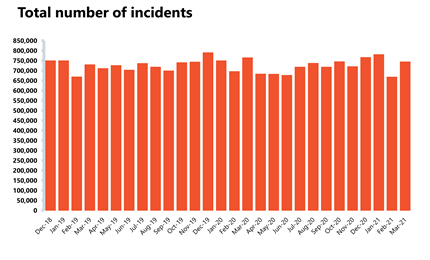
In March 2021, there was an increase in demand for NHS 111 and ambulance services following a dip in the previous month.
- The number of NHS 111 calls offered in March 2021 increased by 25.9% compared to the previous month – meaning 345,225 more calls. This is significantly lower than the first peak of the pandemic, down by 43.3% or 1,283,871 fewer calls than March 2020. Compared to the latest peak in January 2021, the number of calls offered has increased by 5.4% (86,264 more calls).
- Ambulance category 1 incidents also increased by 15.3% to 56,783 in March 2021 (7,552 more incidents). The increase in activity may be due to the easing of the national lockdown restrictions. In comparison to the same time last year, during the first peak of the pandemic, incidents are down by 8%.
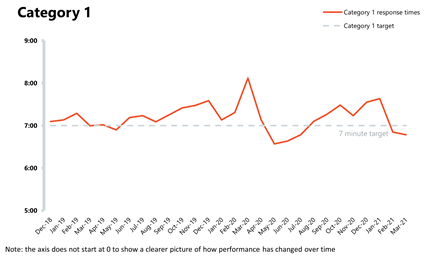
- In terms of performance against the ambulance standards, the mean average response time across England in March 2021 for category 1 calls was 6 minutes 47 seconds, meaning that the target was met again last month. The average response time for category 2 calls has increased slightly this month to 18 minutes and 24 seconds meaning that the target was slightly missed again. However, this is a significant improvement compared to March 2020 (32mins 6 secs) and January 2021 (29 mins 40 secs).
A&E and emergency care:
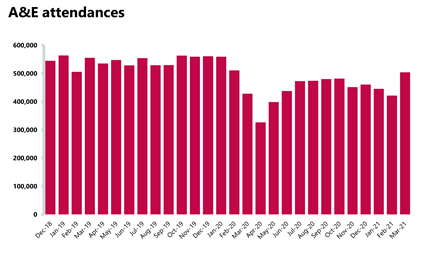
Emergency care activity appears to be picking up again.
- In March 2021, there were 1.69 million A&E attendances – a significant increase of 32.3% since the previous month and 10.5% more than a year before, at the start of the pandemic in March 2020. A&E attendances remain significantly higher than the lowest levels seen in April 2020 (84.5% higher). Emergency admissions have also increased this month by 19.5% and are 17.8% higher than March 2020.
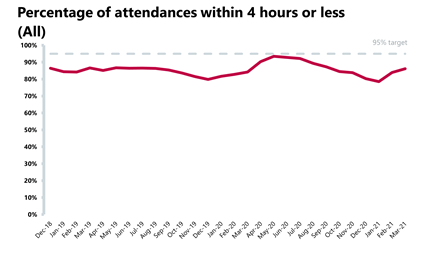
- In March, 86.1% of patients were seen within four hours across all types of A&E. This is a slight improvement than the previous month, but falls short of the 95% target.
- The number of people waiting longer than four and 12 hours has fallen again this month. The number of patients waiting longer than four hours has fallen by 10.8% to 50,972. The number waiting over 12 hours has fallen by 33.7% to 688.
In March, 86.1% of patients were seen within four hours across all types of A&E. This is a slight improvement than the previous month, but falls short of the 95% target.
Elective care:
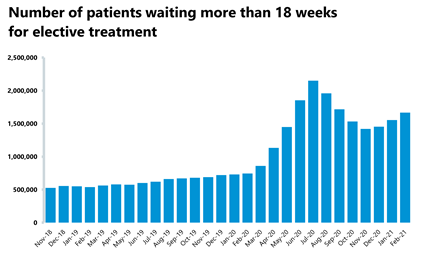
In February 2021 inpatient elective care activity increased on the previous months, but the number of people being added to the list outstripped activity. The waiting list is now the largest it has been in over a decade.
- The size of the elective care waiting list increased by 105,673 to 4.7 million - a 2.3% increase since January 2021. The waiting list is also 6.2% greater than a year ago just before the pandemic.
- The number waiting for more than 18 weeks rose from 1,554,305 in January to 1,667,900 in February, which has resulted in a deterioration in performance against the 18-week standard.
- Performance against the 18-week standard fell for the second month after the improvements over autumn. As things stand, 64.5% of people have been waiting less than 18 weeks. However, the reduction in activity due to COVID-19 in January did not fall by the same extent as in the first peak and performance against the standard is still higher than the all-time low of 46.8% in July and 53.6% in August.
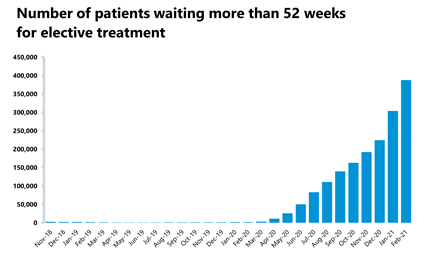
- However, the number of people waiting over 52 weeks has increased by 27.6% in one month, with numbers increasing from 304,044 in January to 387,885 people in February. When compared to the previous year, there are an additional 386,272 people waiting, an increase of 23947%.
Diagnostics:
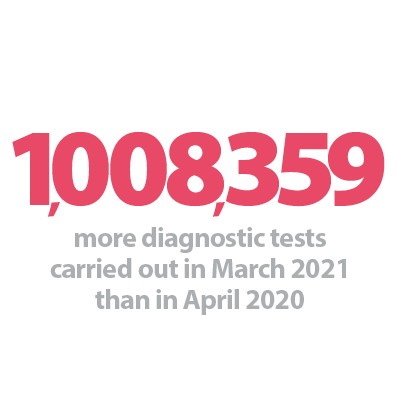
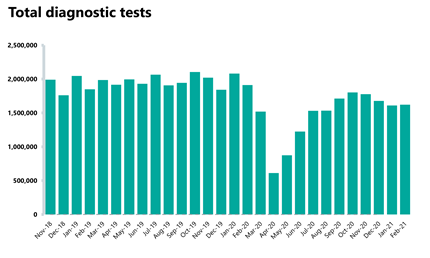
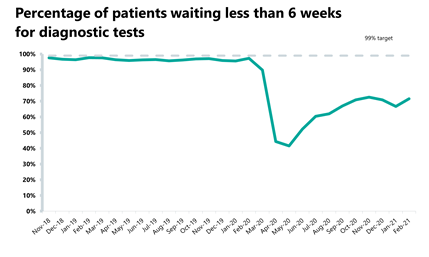
Diagnostic testing remains stable, but significant uplift will be needed to clear the backlog and improve performance across cancer and elective pathways.
- The number of tests carried out in February 2021 has increased by 0.7% to 1.62 million (11,410 more tests than last month). Compared to the year before however, there are 15.2% fewer tests carried out (290,871 fewer). However, when compared to April 2020, there are 164.7% more tests carried out (just over a million more).
- MRI and CT scans both fell since the previous month (by 1.3% and 2.5% respectively). Compared to a year ago, there were significantly fewer tests carried out (14.0% and 4.1% fewer, respectively).
- There were 8.2% more colonoscopy tests carried out compared to the previous month (3,088 more). However, compared to the previous year there were 11.7% fewer tests carried out (5,416 fewer).
- The diagnostic waiting list has increased by 1.6% on last month to 1,151,235 - 18,437 more tests needed. It is up by 6.4% on last year (69,314 more). 28.5% of people were waiting six weeks or more for a test in February, down from 33.3% last month and missing the target considerably.
The size of the elective care waiting list increased by 105,673 to 4.7 million - a 2.3% increase since January 2021. The waiting list is also 6.2% greater than a year ago just before the pandemic.
Cancer:
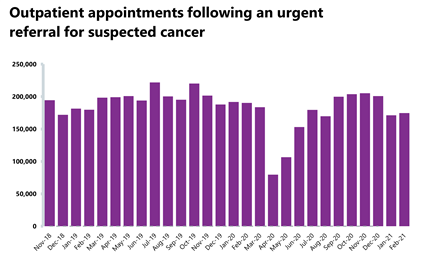
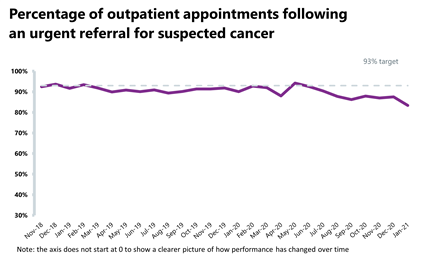
Similar to other services, cancer activity has increased in February, but performance continues to fall short of the waiting time standards. In terms of activity and performance across the three key cancer pathways:
- 174,624 people had a consultant appointment following an urgent GP referral (two-week pathway), which is 2% more than the previous month (3,393 more). This number is down by 8.3% compared to a year ago but over double (119% more) levels carried out during the first peak. Performance against the standard was 90.3%, an improvement from last month but still missing the 93% standard.
- 22,935 people started treatment following a decision to treat (31 day pathway), showing little change on the previous month with seven fewer people starting treatment. Compared to a year ago, this has decreased by 6.3%, but compared to the first peak in April 2020 this is 13.1% higher. Performance against the standard increased slightly to 94.7%, missing the 96% standard.
- 12,208 people started treatment following an urgent GP referral (62 day pathway), which is 1.8% fewer than the previous month. Compared to a year ago, this is 4.3% fewer, but compared to the first peak in April 2020 this is 13.1% higher. Performance against the standard fell from 71.2% to 69.8%, missing the 85% standard and recording an all-time low level.
Mental health:
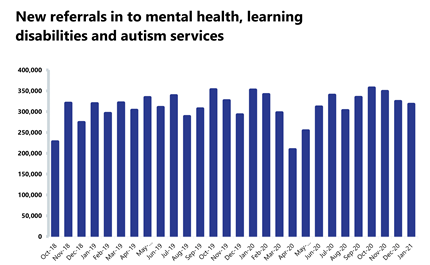
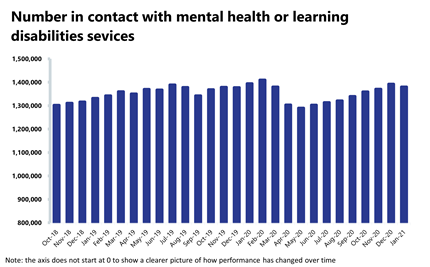
In January 2021, the number of people in contact with mental health services decreased slightly by 0.9% to 1.38 million. Compared to the previous year, there are 1.0% fewer people in contact with mental health services. However, this is 7.0% higher than the lowest levels seen in May 2020.
The number of people being referred for mental health services saw a slight fall of 2.1% to 317,900. Compared to the previous year, referrals have decreased by 9.7% but compared to the first peak in April 2020, referrals remain 52.2% higher.
In relation to inpatient services, in January 2021, the number of out of area placements rose to the highest level in 16 months to 760. This is 7.0% more than the previous month (50 more OAPs). Compared to a year ago this is 11.8% more (80 more OAPs).
In the absence of national waiting list data for mental health, anecdotally, mental health trust leaders are flagging significant levels of pent up demand for mental health services. Areas of critical concern include children and young people’s services and demand for eating disorder services.
In the absence of national waiting list data for mental health, anecdotally, mental health trust leaders are flagging significant levels of pent up demand for mental health services. Areas of critical concern include children and young people’s services and demand for eating disorder services.
Our view
The figures published today across physical and mental health services illustrate just how hard frontline staff and trust leaders are working to recover the care backlogs caused by the ongoing pandemic. Across many clinical areas activity has increased on the previous month, albeit levels falling short of the usual activity seen pre-pandemic.
However, the data published today covers the period of the latest and largest wave of COVID-19. At the peak of the latest wave in January there were 34,336 COVID-19 patients in hospitals across England; 81% more than in the first peak. It is testament to the hard work of staff, therefore, that the NHS continued to carry out diagnostic tests, operations and cancer treatments in much greater numbers than it managed to sustain in the first wave.
Today’s referral and waiting list data also shows the scale and complexity of the future challenge facing trusts across England. The size of the care backlogs across the NHS – in elective and cancer care, in mental health and community services – represents a massive multi-year challenge for the NHS.
Trusts are going, and will go, as fast as they can to recover these backlogs. But they will need multi-year financial support from the government. Additional resources are needed to expand capacity and increase the workforce across services to clear backlogs, to support COVID-19 recovery and to restore waiting time performance to the standards set out in the NHS constitution over time.
For elective care in particular, trusts need financial support to address the pinch point that diagnostic testing currently presents by transforming the pathway and setting up community diagnostic hubs. The investment needed will build on the work that trusts, alongside their partners in primary care, are already doing to better manage waiting lists across local systems, ensuring those with the highest clinical need are prioritised.
Despite the focus on clearing the care backlog, we must also be mindful that we may see another rise in COVID-19 pressures as restrictions ease. Exiting lockdown, staff recovery, tackling further waves of COVID-19 and the cyclical vaccination programme will all need to be considered alongside the urgent need to address the care deficit.
NHS activity tracker
A&E
Cancer
RTT
Diagnostic tests
Ambulance
Mental health
This month’s case study comes from Greater Manchester Mental Health NHS Foundation Trust, who discuss their specialist perinatal community mental health teams, how they have adapted their service during the pandemic, and the support it provides for women during and after pregnancy.
Case study: Greater Manchester Mental Health NHS Foundation Trust
The perinatal community mental health team
Greater Manchester Mental Health NHS Foundation Trust (GMMH) provides the specialist perinatal community mental health teams (CMHT) across Greater Manchester. The teams support women who experience moderate to severe mental health problems during and after pregnancy.
Perinatal mental health problems have a serious impact on women, their baby and the wider family. Mental health problems affect at least one in five women during and or after pregnancy: 3-5% of women will experience a serious psychiatric disorder and it is the single greatest indirect cause for maternal deaths in the UK.
The specialist perinatal community mental health team across Greater Manchester provide assessment, care and treatment to women and their families. This includes the prevention, detection and management of maternal mental health problems that complicate pregnancy and the postpartum year. They work closely across Greater Manchester with all maternity services, adult mental health services, parent-infant mental health services, early years services, primary care, IAPT services and independent and voluntary sector organisations. The CMHT ensure that all health professionals have access to specialist advice and guidance on supporting all women with mental health needs throughout the perinatal period.
Perinatal mental health problems have a serious impact on women, their baby and the wider family. Mental health problems affect at least one in five women during and or after pregnancy.
GMMH also run the mother and baby unit (MBU) which covers the entire North West and accepts women from all over England and Wales. The Andersen ward, which is based at Laureate House on the Wythenshawe Hospital site, provides a high-level of quality, specialist, mental health care to both women who are pregnant and mothers following childbirth. The unit promotes the mother and baby relationship within a secure and supportive environment while incorporating evidence-based practice drawn from the fields of both perinatal and general mental healthcare.
The team on the MBU provides comprehensive advice, medical and psychological assessment, and treatment for women with severe mental health problems. It also offers support and supervision which is tailored to the individual’s needs to promote and ensure the infant’s safety.
The MBU is run by professionals who have longstanding experience in perinatal psychiatry and includes a consultant psychiatrist, inpatient mental health nurses, nursery nurses, an occupational therapist, and a clinical psychologist and has access to physiotherapists and parent-infant psychologists.
The involvement of partners, family members and friends is encouraged and the unit offers support and education for all who visit. The team also provides carer support and has established links with the GM Dad Matters organisation.
The unit promotes the mother and baby relationship within a secure and supportive environment while incorporating evidence-based practice drawn from the fields of both perinatal and general mental healthcare.
How we adapted following COVID-19
Our specialist perinatal CMHT adapted quickly to the COVID-19 pandemic by keeping face-to-face contact for all first appointments. Patients were also given the option to decline face-to-face appointments if they felt uncomfortable. After the initial appointment, patients were given the choice of either face-to-face, video or telephone appointments. The type of appointment was also dependent on the level of patient risk.
Video clinics were also introduced for women who were usually seen in community centres that had since closed due to the pandemic.
In the Andersen ward, we introduced video conferencing in to ward rounds and professional meetings. We also ensured safe contact with patients and their family by introducing a family bubble. This allowed one member of the family of a patient to visit them in a room which was cleaned to COVID-19 infection prevention control standards. This enabled partners and family members to maintain contact with their family member who was an inpatient and develop their relationship with the baby or infant.
Our specialist perinatal CMHT adapted quickly to the COVID-19 pandemic by keeping face-to-face contact for all first appointments. Patients were also given the option to decline face-to-face appointments if they felt uncomfortable.
Letters were also sent to commissioners and GPs about the importance of perinatal mental health and babies in the lockdown period. Staff within each cluster in the CMHT moved to working in two separate bubbles to prevent infection and maintain a COVID-free environment.
Morning wellbeing checks were also introduced. All staff attended these checks and they enabled staff to maintain a collaborative approach to their work while sharing best practice and their objectives. These morning meetings also enabled staff to discuss patients who are identified as high risk and how best to treat such patients. This approach was called zoning. Regular group and individual staff wellbeing checks were also carried out throughout the day and over lunch breaks via Microsoft Teams.
Staff were also able to catch up over Teams to discuss work as they would have passing by in the corridor.
Staff within each cluster in the CMHT moved to working in two separate bubbles to prevent infection and maintain a COVID-free environment.
The impact for patients
These efforts since the pandemic started mean that we have supported 1,541 mothers and their families. 1,473 were supported by the specialist perinatal CMHT whilst 68 were supported by the mother and baby unit.
This is a remarkable team effort. The team have recently received outstanding feedback in the Perinatal Quality Network peer review which reviewed the service from January 2020 to January 2021. The team were praised by the network for being "cohesive and passionate", with "strong clinical leadership". Patient feedback included "professional, compassionate, very experienced and intuitive to individual needs", and one patient stated the service has "absolutely zero faults" and was "so grateful for this service, I couldn’t have asked for more".
The feedback from the network and patients shines a light on how important it is to support those who are suffering from perinatal mental health issues. Such positive feedback are brilliant examples of the hard work of staff to successfully restore and maintain mental health services in a challenging 12 months.
Press statement
Trusts are working hard to recover backlogs but there is a difficult road ahead
Responding to the latest monthly combined performance data from NHS England and NHS Improvement, NHS Providers chief executive Chris Hopson said: "The figures published today illustrate how hard trusts are working to recover care backlogs as well as the size of the future challenge they face, despite a decline in COVID-19 patients.
"The trend across A&E standards, ambulance activity, cancer performance, and the number of diagnostic tests carried out shows that activity across the NHS is rapidly improving since the COVID-19 peak in January.
"We know that the NHS has a track record of moving at pace and adapting to overcome challenges, as we are seeing with the vaccination programme, and saw when the NHS reconfigured itself at the start of the pandemic. Every trust is doing everything it can to deliver, especially for the most clinically urgent patients. We saw that in how trusts recovered care last summer, after the first COVID-19 wave, and we are seeing it again now.
"But the size of the care backlogs across the NHS – in elective and cancer care, in mental health and community services – represent a massive multi year challenge for the NHS. Trust leaders are obviously concerned, for example, that the waiting list has increased to 4.7 million and there are almost 400,000 people waiting over 52 weeks for surgery. They’re also worried about the lack of inpatient beds for children with serious mental health need and the explosion of demand we’re seeing for many services such as eating disorders.
"Trusts are going, and will go, as fast as they can to recover these backlogs. But they will need multi year financial support from the government to expand capacity, increase the workforce, address pinch points like access to diagnostics and invest in new ways of delivering care to treat more patients more quickly.
"There is a difficult road ahead but trust leaders are clear that, with the right support from government, they can meet this challenge in the same way they have met so many others over the last 15 months."