
Commentary
Context
Trusts and frontline staff are working flat out to restore those services which were necessarily interrupted to cope with the first peak of the pandemic. Our Restoring services: NHS activity tracker highlights detailed examples of the innovations trusts and their staff developing to improve capacity, and respond to unmet demand despite the constraints created by COVID-19, and the need to prepare for additional winter pressures.
Trust leaders are only too aware of the disruption and distress for many patients caused by the need to focus on COVID-19 at the height of the pandemic. However recent claims that all non-COVID care came to a grinding halt are simply not true. At the peak of the pandemic, for everyone COVID-19 patient in hospital there were two non-COVID patients being treated for other conditions. Trusts continued to carry out over 41,000 emergency operations in April and find ways to safely continue cancer care in the context of COVID-19. And most mental health and ambulance, and many community services, continued to function at their pre-COVID levels of activity, or higher.
Factors which continue to have a bearing on capacity levels include:
- a drop in the numbers of people seeking help during the height of the pandemic and a significant reduction in the number of GP appointments resulting in fewer referrals to secondary care
- reduced capacity across the NHS due to necessary infection control measures (such as regular deep cleaning), social distancing and additional PPE requirements
- changes in clinical practice in response to COVID-19
- changes in patient behaviour in response to COVID-19 which mean that for a range of reasons people can be less confident about seeking help or treatment.
This month’s performance figures
Each month NHS England publishes statistics looking at performance across a range of services including urgent and emergency care, routine care, cancer, and mental health. The data show how much activity has been undertaken and how long patients have been waiting, against a range of waiting time access standards.
Below we highlight some of the latest trends and figures in both areas.
NHS activity
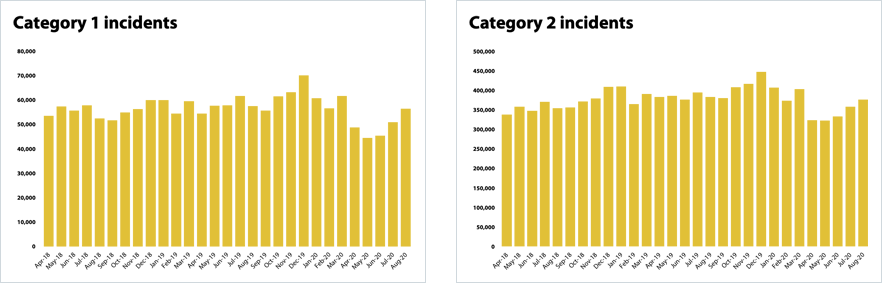
- Ambulance activity is steadily increasing. The number of category one incidents receiving a face-to-face response from an ambulance service or resolved on the telephone has increased by 11% to 56,498 from July to August, equating to 5,590 more incidents receiving a response. This means ambulance ‘category one’ activity is returning to levels similar to those recorded in February prior to the pandemic.
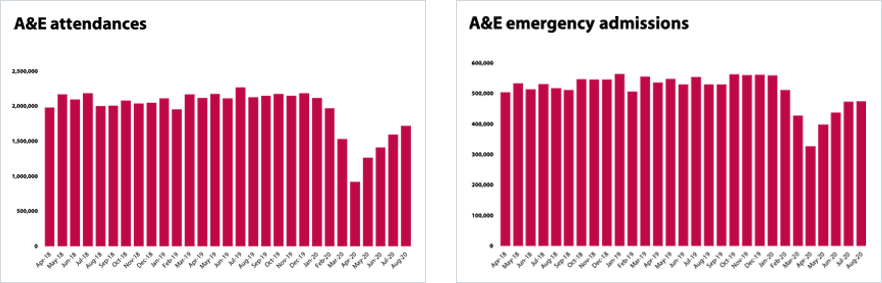
- The urgent and emergency care pathway is also seeing increases in activity. In April 2020 the number of people who attended A&E fell to under a million – an all-time low in recent decades. However, since May there have been increases month on month. In August 88% more people attended A&E than they did in April, with attendances reaching 1.7 million.
- The number of people attending A&E in August is still a fifth lower than in August 2019. This reduction is likely to be drive at least in part by the public choosing NHS 111 and other primary care services when A&E wasn’t required, and potentially choosing not to seek help in a hospital setting as a result of COVID-19. It is worth noting that NHS England and NHS Improvement are now piloting enhanced NHS 111 services ahead of winter to encourage the use of more community based pathways for those patients who may need advice or treatment but do not need to attend an A&E setting.
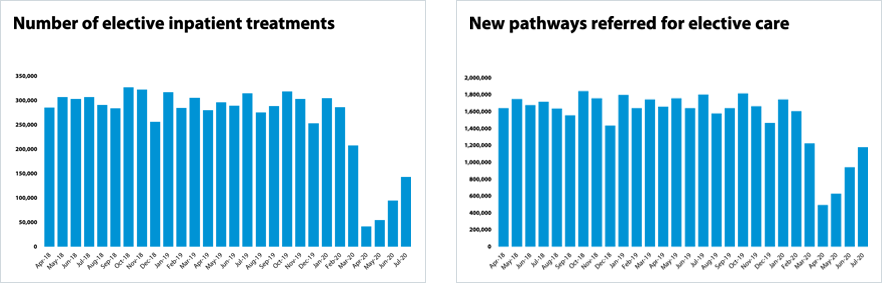
- In April routine operations were officially paused for two weeks under a direction from NHS England and NHS Improvement although trusts were asked to continue urgent operations. Activity has started to increase each month. Trusts are working together across systems and using private sector capacity to increase activity in this area. In July 2020 there were 51% more operations than in June this year - and 247% more than in April 2020.
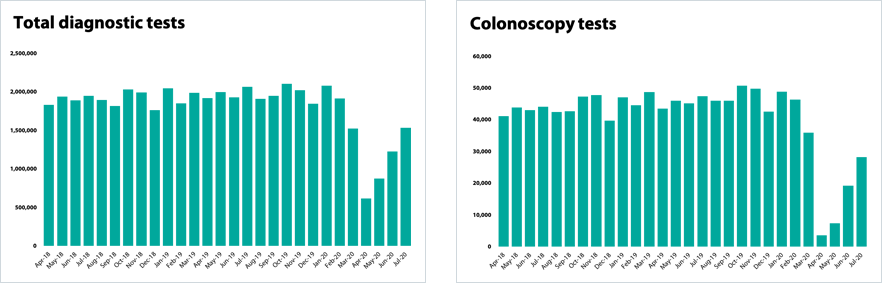
- Activity is also being restored across diagnostics, and there were 25% more diagnostic tests undertaken in July than in June. However, there is variation by test type. For example, colonoscopy tests fell to just over 3,000 in April but by July trusts had increased this number to over 28,000. This is still short of the 48,000 completed in February but shows that progress is being made.
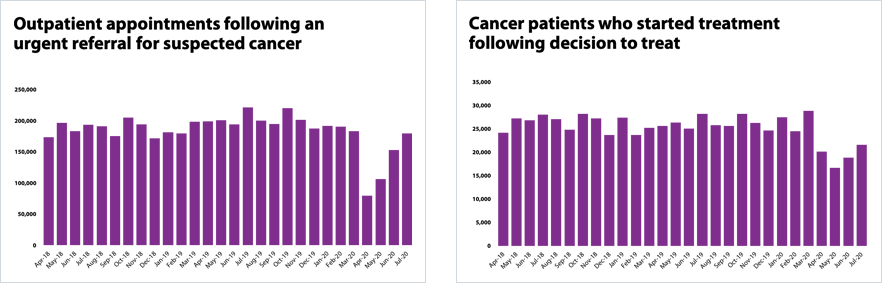
- Cancer care has been impacted by COVID-19, particularly because those undergoing treatment often have compromised immune systems. Trusts have been working closely with patients and finding innovative ways to continue treatment. As a result of a significant fall in GP consultations throughout the peak of the first wave, there was a reduction in urgent two-week urgent referrals for a suspect cancer. However, positively, each month the number of outpatient appointments following an urgent referral is increasing. In July, 17% more people attended an appointment than in June. In fact, nearly 100,000 more people have attended an outpatient appointment following a referral in July than in April.
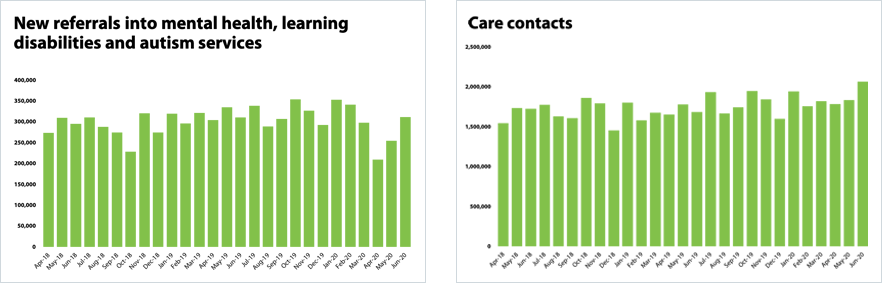
- In relation to mental health, referrals have been increasing month on month since April. In June 2020, referrals increased by 4.7% to 311,393 since March 2020. In June 2020, there were 111,752 referrals received to Improving Access to Psychological Therapies. This is an increase of 42.3% (33,208) since last month. Anecdotally trusts report significant increases in demand for early intervention services, often linked to the wider impacts of COVID-19 such as economic hardship.
- Although referrals are down, mental health contacts (the number of interactions with services) is the highest on record at 2,062,570 and have increased by 12.4% in the past month. This is 17.3% more contacts than in February which shows that following the pandemic mental health services are providing more interactions than ever before.
NHS waiting times
- The most concerning figures from this week’s national figures are those for elective care which includes routine operations. Trusts tell us this is the biggest challenge they are facing and are undoubtably very concerned that their patients are having to wait longer for care. Trusts have also told us that they are working collectively to prioritise those most in need.
- The number of people who have been on the waiting list less than 18 weeks has fallen to 46.8% and the number of people waiting over 52 weeks has gone up from just over 3,000 in March to over 83,000 in July.
- In emergency departments there is a long-established target that 95% of people should be seen within four hours. The NHS has failed to meet this target for the past five years. Due to the reduction in the number in A&E attendances, trusts had seen some improvement against the standard which rose to 93.5% in May. However, as activity begins to increase each month, performance against the target has declined. In August 89.3% people who attended A&E were seen within four hours.
- In relation to ambulance services the reduction in people accessing services resulted in the sector meeting both its Category 1 and Category 2 targets for several months. However, the latest data for August shows that as activity once again increases, the average response times have slipped with the sector missing the seven minute and 18 minute targets.
- As diagnostics tests have started to increase patients waiting for six weeks or longer for one of the 15 key diagnostic tests fell to 39.6% this month, down from 47.8% last month. This is much longer than the target of 1% but the trend is at heading in the right direction.
- Trusts have worked hard to maintain performance against the cancer standards. The latest data showed that 90.4% of patients with an urgent GP referral for suspected cancer were seen within two weeks, missing the 93% standard. As those that start cancer treatment continues to rise, nationally 95.1% of those starting treatment following a decision to treat, did so within 31 days narrowly missing the 96% standard.
Our view
The pandemic has had far-reaching implications for all NHS services, spanning mental and physical health care in all settings.
The data published in September reflects the hard work by trusts to restore services in what remains a very challenging period for everyone across the NHS. Trust leaders are particularly concerned about the number of patients having to wait longer for diagnostic tests or to receive the treatment they need. It is right that we acknowledge that people are waiting longer, and we know that trusts and systems are working together to tackle this unfortunate consequence of the pandemic. However, looking at waiting times alone would miss a key part of the post-pandemic recovery story.
The same frontline staff who worked so tirelessly to respond to the challenges of the first peak, are the very same staff who are now doing all they can to restore services. To focus solely on longer waiting times, and not the positive gains they are making in increasing activity levels does them a disservice.
Trusts often have to use new and innovative approaches to keep patients and staff safe because of the constraints created by COVID-19 with regard to infection prevention and control. Below we set out a number of examples of ways trusts are restoring service and thinking ‘outside the box’ to provide patients with the care they need, including in mental health services and in a drive through phlebotomy and lung function services.
Recovery from the experience of a pandemic was always likely to be incremental but many trust leaders report that they are exceeding their own expectations of the speed at which services can be safely restored. Trusts have proved that they are well on their way to restoring services alongside responding to the now increasing number of COVID cases and planning for winter.
NHS activity overview
Ambulance services
Urgent and emergency care
Diagnostic testing
Elective care
Cancer services
Mental health services
Case studies
Addenbrooke's Hospital, Cambridge University Hospitals NHS Foundation Trust
Ewen Cameron, Director of Improvement and Transformation
Over the past few months getting vital services back up and running while continuing to care for COVID-19 patients has been the main focus for us as a trust.
Delays to treatment can lead not only to further physical problems down the line for patients but almost inevitably cause anxiety and mental health issues too. It’s for this very reason that maintaining cancer services has remained one of our top priorities.
With the efforts of our dedicated staff and some innovative approaches, we have kept our cancer diagnosis and treatment services running. We have maintained chemotherapy capacity throughout the pandemic by extending treatment hours and opening at weekends. We typically receive 280 cancer referrals per month, but at the start of the pandemic, in order to maintain social distancing, the number of chemotherapy spaces were cut by almost half from 40 to 23. However, with enormous efforts from our cancer teams, we were able to extend our service hours and ensure patients got the care that they needed.
We also took on recommendations from a breast cancer study which showed that some patients could be treated safely over a week rather than three weeks. We were also one of the first hospitals to restart Public Health England’s bowel cancer screening programme. The programme, offered to all those aged 60, provides the opportunity to be tested for bowel cancer by sending in a stool sample. Colonoscopies are typically performed within two weeks of receiving a positive test, but due to the pandemic, some patients have had the unfortunate wait of up to three months to see if they are at risk.
One such patient was Dennis Barry, 71. Dennis was identified as needing a colonoscopy just before lockdown in March and was one of our first patients to receive a colonoscopy when services were switched back on in June. He said: “When you hear the word 'cancer', you always think the worst. I'm not saying it's on your mind 24/7 - you forget about it halfway through the day and then in the evening you sit down maybe have a sandwich or watching the TV and all of a sudden it'll just come back to you 'oh dear, what if I do have cancer?”
Dennis’ colonoscopy revealed he had pre-cancerous polyps and abnormal tissue growths, which were removed a week later. With the scare over, he is now back doing what he loves most, sea fishing.
It’s cases like these which make us more determined to find novel ways of restoring capacity.
Working with our partners across the local health care system and the Cambridge Biomedical Campus has enabled us to find ways of treating people closer to home and has also allowed us to speed up cancer treatment times with the use of cutting edge technology such as AI and machine learning.
Our outpatients department has also seen some dramatic changes. For instance, we went from having only 750 remote video or telephone appointments a week to 5,000 a week.
We also moved some of our services off-site in order to reduce the risk of infection and reduce the number of patients coming on site. For example, drive-through blood tests are now available at a nearby Park and Ride in Cambridge.
Overall, we have made incredible changes and have been hugely impressed by all of our staff, from receptionists manning the front desk to consultants and nurses at the heart of medical care. Our staff have literally rolled up their sleeves, shielded themselves with the right PPE and focused on what needs to be done.
It’s important to recognise the support we’ve had from patients too. They’ve had to cope with considerable changes, from restricted visiting, to virtual appointments, to wearing facemasks on site. We recognise that despite our best efforts, and some super-human achievements, some patients are still having to wait longer for their treatment than we want with potentially serious impacts on their quality of life.
Although we are proud of being able to maintain many services throughout the COVID-19 crisis, we will always strive to get as much capacity back on track as quickly and as safely as possible.
East London NHS Foundation Trust
Paul Calaminus, Deputy Chief Executive
There has been a lot of focus recently on the importance of ’restarting’ the NHS to address the impacts of the COVID-19 pandemic. From my perspective in a mental health and community trust, the ’restart’ of services began several months ago. For example, acute mental health wards (providing 24-hour care to the most acutely unwell) returned to pre pandemic activity levels by July, having taken a dip at the height of the pandemic.
Indeed, the majority of all of our services never stopped running throughout the pandemic and new services were opened during April and May while the pandemic was at its peak. Among these were new 24-hour walk in services able to provide face to face assessment and support. Similarly, phone lines were bolstered during these months, and have continued to operate – now taking double the number of calls of a year ago. And these services are proving accessible, with about half of all attendees newly seeking help.
While services are now offering more digital services, face-to-face work has continued, and we have continued to maintain waiting times to pre-pandemic level (with reductions in some place) for our community mental health teams. In part, this has been delivered because we (like every community and mental health trust I know) have worked alongside our primary care colleagues to design new ways of working. In mental health this has led to us delivering more care closer to the community and linked to GP practices which has enabled us to get help to people more quickly.
In our Improving Access to Psychological Therapies services (a key source of support for many thousands of people each year) we have seen referral activity return to pre-pandemic levels, and we are on track to continue the planned expansion of these services during the remainder of the year. In these services, more is now provided online. The work of both our clinical teams and the service users they work with to design digital models of care together has been quite remarkable. Here too waiting times have decreased during the pandemic, even while activity levels have been returning to normal and are expected to continue to increase.
We have also been working hard on our Children and Adolescent Mental Health services. While there has been a drop in referral rates (quite similar to a drop we often see during the school holidays) we have increased our crisis services and seen an increase in self-referrals too. As with every Autumn, services are ready for the increase in referrals we are expecting as young people return to education.
Finally, I have to reflect on the help and leadership from our service users. This has extended to designing a befriending service that has now offered support to well over a thousand people over the last few months. Interventions such as these have really helped to support the work of clinical services over the course of the pandemic and provided invaluable support for people in the community.
The same is true in community health, where district nursing services have seen response times to referrals remain stable, taken on new and enhanced roles in support care homes, running integrated discharge hubs in partnership with acute hospital and social care colleagues, and opening COVID-19 positive facilities at short notice to provide safe step down care from hospital.
There is plenty of work to do to bring back all of the services in the NHS and this is a complex task. But I would just reflect, as above, that for much of the NHS, services have continued running through the pandemic period: new services have been established, and new ways of working developed enable us to approach this task with some confidence in our ability to work with service users to achieve recovery.
Epsom and St Helier University Hospitals NHS Trust
Daniel Elkeles, Chief Executive
At the height of the pandemic, we were hit very hard by COVID-19, and had over 300 patients with confirmed or suspected COVID in our hospitals. We redeployed 350 staff from their normal duties to support our emergency care teams to manage the influx of patients.
Like many other NHS providers, we scaled back our planned care to the most urgent patients. However, since July, after much careful consideration and a huge re-think on how to operate safely in an estate that largely pre-dates the NHS, we have steadily re-opened our planned care programmes.
The good will of staff to get our services back to a 'new normal' has continued from the height of the pandemic in the spring to now. We have been fortunate enough to have lots of staff who continue to volunteer extra hours during the day and at weekends. Part of the reason why staff are working extras hours is due to enhanced infection control practices lengthening procedure times.
We are well on the way to returning to business as usual. At the end of August, we achieved:
- 71% of our usual level of activity in planned care procedures (inpatient and day cases)
- 107% of our dedicated orthopaedic centre’s normal level of activity compared to last year
- 90% of our endoscopy activity and 86% of other diagnostic activity.
Now that all our new outpatient clinics have gone live, we aim to reach 80% of activity by the end of September.
Some of the many measures that we have taken to get services safely re-started include re-signing our hospitals to create one way flows, manning checkpoints at entrances to welcome patients safely and moving outpatient departments so they aren't located near to wards. We have also increased waiting room capacity, for example by using the League of Friends shop as an additional waiting area, and we have set up a booking system for blood tests which sees 450 people per day rather than having direct access. Other major changes include changing every one of our 2,800 clinics and now 40% of our outpatient appointments are 'virtual'. We have also installed one portable CT scanner and have received funds for another CT and MRI scanner to be installed by Christmas alongside extra endoscopy equipment.
The pandemic has allowed us to work better together with private and NHS providers to deliver the essential care that our patients need. We have made really good use of the private sector capacity made available to us by NHS national bodies with government funding and become the biggest user of the facilities in our local private hospital. Our community services have restarted all their planned care services as well. The collaboration between the four hospital trusts in South West London has continued to go from strength to strength - we are successfully sharing the longest waiting lists between us and working collectively to increase surgical and diagnostic capacity.
The catch up required is huge but we have already made great progress. To put it into perspective, before the pandemic we had less than 10 patients waiting more than 52 weeks for treatment and the number of patients waiting now is almost 300. If we have a benign winter with no significant COVID-19 surge then we will be back to business as usual this autumn, with the hope of being caught up with most services by Easter.
There is no doubt that recovering from the virus has taken an incredible amount of effort. I am so proud of our staff for everything that they have been doing for our local communities to restart services in a safe and careful way.
Luton and Dunstable University Hospital, Bedfordshire Hospitals
NHS Foundation Trust
Rachel Geary, Lead Clinical Respiratory Physiologist
In the age of COVID-19, we are all adapting to new ways of providing services in hospitals. This includes introducing new and innovative approaches to carrying out routine procedures. At Bedfordshire Hospitals NHS Foundation Trust, we have taken an interesting new approach to performing lung-function tests on our patients.
Prior to the pandemic, patients would have come into the clinic to have their lung-function test where there would have been up to 40 test slots a day at each hospital. However, because lung-function testing is an aerosol generating procedure, the room where it is performed needs a minimum of six air changes per hour to maintain important infection prevention and control rules. This means only four test slots a day are available - reducing usual capacity down to 10%.
To tackle this and at the same time address the huge backlog of patients that regularly need tests, our respiratory physiologist team have come up with a novel solution - making the patient’s own car the ‘test laboratory’.
As a result, a new drive-through lung-function testing system was created in the disabled car park. The team are now back up to 100% capacity again and the facility is currently open seven hours a day, five days a week.
The respiratory physiologists wear enhanced PPE and the test is performed with the patient safely inside their car. The physiologist passes the handle through the window, which the patient winds up so that it is open only slightly. The main body of the device is then operated from the roadside.
This has proved to be an extremely efficient system for testing patients. This high-quality service is safe and cost-effective while alleviating patient anxiety and reducing pressure on diagnostic services within the hospital building. Patient feedback so far has been extremely positive – particularly those patients who have been shielding, as they feel so much safer.

Royal Papworth Hospital NHS Foundation Trust
Stephen Posey, Chief Executive
In April, at the peak of the pandemic, Royal Papworth Hospital became the busiest critical care department in the East of England. We received some of the region’s most seriously ill patients. As a result, we expanded our extracorporeal membrane oxygenation (ECMO) service to four times its usual capacity. Thanks to the expertise and commitment of our staff, we achieved excellent outcomes for our COVID-19 patients and more than 75% were discharged either to their home or to their local hospital.
As a specialist heart and lung hospital, we maintained our urgent and emergency services, such as our lung cancer service and the heart attack pathway throughout the pandemic. However, as directed by NHS England and NHS Improvement, we had to postpone most of our elective activity in response to the peak of the COVID-19 crisis.
Even as early as April, we were thinking about service recovery and how to involve our staff in doing so. Understandably, our staff were exhausted from responding to the pandemic so we sought a balance between restoring services quickly and safely as possible for patients while still ensuring staff had time to rest and recharge. We are incredibly proud of our staff who have responded spectacularly to the challenge of restoring services. We are also fortunate to have the infrastructure in the form of a modern, purpose-built hospital with single patient rooms and enhanced ventilation, which has undoubtedly supported our recovery.
We listened carefully to the concerns staff had about restoring services. We were honest and transparent about the fact that reduced diagnostic, bed and theatre capacity from staff shielding and social distancing requirements, as well as lost productivity caused by the additional safety measure of wearing PPE would impact on how we recovered services.
We felt it was important to quantify the impact of these constraints and show staff what was possible under these unexpected, new constraints. To do this, we developed a dynamic hospital model using previous years’ data to show what was ‘normal’ in terms of staffing hours, theatre time and other factors. We then adjusted the model to take into account COVID-19-related constraints. The model made clear how certain factors such staff shielding, PPE, and the additional demands of creating an ongoing service for COVID-19 patients would impact on how we recovered services. Our clinical leads developed a realistic strategy that would help us deliver the greatest clinical benefit with the resources available to us.
Involving our clinical teams in this work helped us to develop a strategy that everyone bought into. It also gave us the impetus to prioritise several actions, including more detailed risk assessments to identify staff who could safely work in the hospital, some changes to donning and doffing PPE in theatres to improve flow, and a clear plan for our ongoing COVID-19 service.
On 31 July 2020, NHS England chief executive Sir Simon Stevens set out national targets for service recovery, and we are already exceeding these targets in diagnostic imaging and elective inpatient admissions:
- our cardiology service has restored day case and admitted activity to match some of our most productive months last year and our transplant service is actually carrying out 30% more heart and lung transplants than in February 2020, helped in part by an increase in donations following the recent change in law
- the number of thoracic and cardiac operations we perform is also exceeding NHS England’s national targets
- our outpatient service is set to meet this month’s targets for first and follow-up appointments, even though we have seen a reduction in cardiology referrals after providing better guidance to primary care about when referrals are necessary
- some services have been slower to recover, for example respiratory medicine and sleep services, partly due to patients being understandably nervous about coming into hospital, but we are making good progress in these areas too.
We are immensely proud of our staff and how hard they have worked to achieve these results. Even at the peak of the pandemic, when we were caring for unprecedented numbers of seriously ill COVID-19 patients, our ‘usual’ patients were never far from their thoughts. Despite the challenges, we will keep working with passion and commitment to give all of our patients the treatment they need.
Press statements
Restoring services: The NHS is rising to the challenge once again
Growing evidence is emerging of the extraordinary commitment and innovation of NHS frontline staff to restore services for non COVID-19 patients.
NHS Providers will highlight examples of this outstanding work, covering a wide range of activities and procedures, in a new series of briefings over the coming months.
Restoring services: NHS activity tracker will set out in detail how trusts and staff are working to raise levels of routine care despite the continuing threat from COVID-19, and the need to prepare for additional winter pressures.
Trust leaders are only too aware of the disruption and distress for many patients caused by the need to focus on COVID-19 at the height of the pandemic. However, recent claims that all non-COVID care coming to a grinding halt are simply not true. At the peak of the pandemic, for every one COVID-19 patient in hospital there were two non-COVID patients being treated for other conditions. And most mental health and ambulance, and many community services, continued to function at their pre-COVID levels of activity, or higher.
Trusts and frontline staff are now working flat out to restore those services which were necessarily interrupted to cope with COVID-19. They are doing so in the context of a range of COVID-19 related constraints that, for some trusts, have meant the loss of between 10% and 30% of their normal capacity. These constraints include:
- loss of waiting room and/or bed capacity due to social distancing in acute, mental health and community settings
- loss of surgical and patient facing time in all settings due to the need to wear and change, with appropriate frequency, cumbersome personal protective equipment
- loss of access to diagnostic testing equipment and other physical equipment due to the need for deeper and more frequent cleaning between patient treatments
- loss of bed space and access levels to diagnostic equipment due to the division of estates into COVID and non-COVID areas
- limitations on ambulance trust capacity due to the need for deep cleaning vehicles.
By offering frontline commentary and compelling case studies, this new series will show the spirit of resilience and resourcefulness that served the NHS so well at the height of the pandemic is alive and well as trusts rapidly recover service volumes.
Examples from the first briefing include:
- restoring cancer screening and treatment services at Addenbrookes Hospital in Cambridge by compressing treatment times when it was safe to do so, extending opening hours and staff working weekends
- a new drive-through lung function testing system at Luton and Dunstable Hospital Foundation Trust
- increasing virtual outpatient appointments, expanding waiting room capacity and using private sector capacity for planned care in Epsom and St Helier University Hospitals
- finding new ways to maintain mental health services during the pandemic and working with service users to co-create a service in East London
- exceeding pre-COVID heart and lung transplant service activity and restoring cardiology services at Royal Papworth Hospital NHS Foundation Trust.
The NHS Providers chief executive, Chris Hopson, said:
"Much of the public commentary over the last few months has focused on how far NHS activity has fallen. Very little of it has focused on how hard NHS frontline staff are working to recover services and how rapidly they are succeeding.
"Every trust leader recognises that COVID-19 has forced the delay of some treatments to patients and that this has significant impact for patients and their families. No-one underestimates the huge challenge this poses for the NHS.
"But we also owe it to frontline NHS staff to recognise their hard work, their ingenuity and their persistence in overcoming a set of wicked constraints – lost beds, lost patient and surgical time, lost diagnostic test slots – because of the unavoidable need to protect patients from COVID-19.
"As our new briefing shows, frontline staff are working just as hard, and being just as innovative, as they were in the first COVID-19 peak earlier this year. Chief executives tell us that they are recovering activity levels significantly faster than they were expecting to, just two or three months ago.
"Trust leaders worry that the current unrelenting focus on what the NHS is unable to do, as opposed to how rapidly it is recovering services, is also discouraging patients from coming forward to seek help when they need it.
"The NHS is there for all patients, whatever their need. Trusts are going as fast as they can to treat the same number of patients as they were before the pandemic hit, despite the constraints they face. Our new project will shine a light on some of the incredible things trusts are doing up and down the country to make this happen."
Performance figures show just how hard trusts are working to restore services
NHS Providers deputy chief executive Saffron Cordery said:
"Today’s figures show just how hard trusts and frontline staff are working to restore services for non COVID 19 patients.
"They are doing this in the context of various constraints, such as a reduction in available diagnostic testing equipment and ambulance capacity due to the need for deeper and more frequent cleaning between patient treatments, and additional time needed to wear and change personal protective equipment.
"While many people have had to wait longer than usual for treatments due to the need to focus on COVID-19, the figures highlight the commitment and hard work being undertaken by frontline staff to boost activity with the aim of returning to pre COVID levels of service as quickly as possible.
"Although the figures show there are over four million people on a waiting list for elective care and those waiting over 18 weeks has significantly increased, the number of operations carried out has increased by more than 50% since June and is up by almost 250% since April. Additionally, in July 25% more diagnostic tests were carried out than in June.
"The number of people who attended an outpatient appointment following an urgent referral by their GP for suspected cancer is also up 17% on last month, and the number of people with cancer who started treatment following receipt of an urgent GP referral for suspected cancer is also up 19%.
"There has also been a significant increase in the number of people attending A&E since April, with emergency rooms treating 88% more people.
"The recovery from the peak of the pandemic was always going to require step by step increases in activity and the NHS is well on the way to restoring services. We are in a much better place than many would have predicted a few months ago.
"We should not focus solely on what COVID-19 has stopped the NHS doing. We must also recognise how rapidly acute, mental health, community and ambulance trusts are recovering services working across the entire health and care system to keep people safe.
"These figures highlight that the NHS is open for everyone and people must come forward to seek treatment if they need it."