
NHS Activity Tracker
Introduction
Over the last few weeks the number of positive COVID-19 infections in the community has increased. However, today's Test and Trace data covering 24 - 30 June 2021 shows that positive cases have jumped up significantly with an increase of 75% since last week. This means that positive cases are back to figures observed in early February 2021 around the peak of that wave.
Hospital activity is also increasing, and as of 7 July 2021, there has been a week on week increase of 70% in hospital admissions and 42% in the total number of COVID-19 patients in hospitals. Despite the increase in community prevalence, we are yet to see infections translate into the same level of hospital admissions as in the January/February 2021 wave. This is largely down to the success of the vaccine programme and the hope that the link between infection and severe illness has been broken.
However, as the numbers start to increase, the treatment of COVID-19 patients is once again more widespread. This is supported by more data released today showing that the overall weekly hospitalisation admission rate for COVID-19 increased from 1.97 per 100,000 last week to 2.65 per 100,000 in week 26. Outbreaks in care homes also doubled from 48 to 96 in the past week.
Alongside the latest increase in COVID-19 pressures, trusts are telling us that demand across the urgent and emergency care pathway, spanning ambulance services and emergency departments across the country, is at record levels for this time of year. Trust leaders continue to report that mental health services face their own challenges alongside those delivering physical care services. Both messages are strongly reflected in the activity and performance data for June and in this blog we explore how the rising COVID-19 rates may impact hospital pressures over the rest of the summer.
This month's performance figures
Each month NHS England and NHS Improvement publish statistics looking at activity and performance across a range of services including urgent and emergency care, routine care, cancer, and mental health. Below we set out the latest trend for each clinical area:
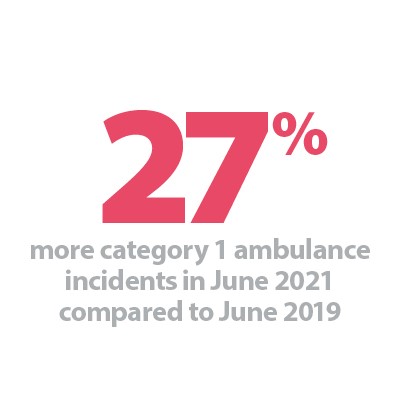
NHS 111 and ambulance: Activity continues to rise across the urgent and emergency care pathway meaning ambulance services are facing more pressure and unprecedent levels of demand for this time of year.
- Ambulance category one incidents, those requiring immediate intervention and resuscitation, increased by 8.1% since last month to 73,505 (5,523 more incidents). Compared to two years ago before the pandemic, they have increased by 27%.
- For the second consecutive month, the ambulance service has missed the average mean response time target of seven minutes for category one calls, exceeding it by 54 seconds. The average response time for category two calls also deteriorated further, missing the 18-minute target with an average time of 30 minutes and 42 seconds. This is the highest average response time seen since March 2020.
A&E and emergency care: Activity across emergency departments increases again this month, reaching the highest number of A&E attendances in 18 months and the highest for any June since records began.
- In June 2021, there were 2.15 million A&E attendances – the highest figure since December 2019 and the highest figure for any June on record.
- There were 535,173 emergency admissions in June 2021, a decrease of 1.6% since the previous month but up by 22.3% since June 2020.
- Performance against the four-hour waiting time target continues to deteriorate as it drops to 81.3%, missing the 95% standard.
- The number of patients waiting longer than 4 hours has increased this month by 16.2% to 66,619 (9,312 more). The number of patients waiting more than 12 hours has increased significantly by 85.7% to 1,289.
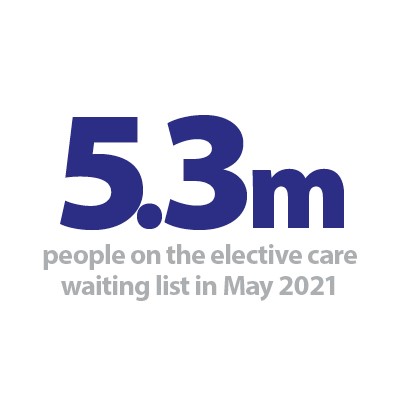
Elective care: Planned care activity increased again in May 2021, but referrals still outstrip supply as the waiting list continues to grow, reaching 5.3 million. Trusts continue to reduce the number of long waits, with patients waiting 52 weeks or more decreasing for the second consecutive month.
- In May 2021, the size of the elective care waiting list increased by 3.6% to 5.3 million (182,932 more). This is the highest level seen in the current records over the last decade.
- The number of patients waiting more than 18 weeks decreased for the first time in months, falling by 4.6% since April. With fewer people waiting over 18 weeks, performance against the 18-week standard improves slightly, increasing to 67.4% in May 2021.
- The number of people waiting over 52 weeks has decreased for the second month running. The number of long waits fell by 12.6% to 336,733.
- The data shows that in May 2021, a total of 76,583 patients were waiting at least 18 months (78 weeks) for elective treatment. Of these, 7,403 patients were waiting at least two years (104 weeks) for elective treatment.
- In May 2021, 151 trusts had at least one patient waiting at least 52 weeks (same as last month); 140 trusts had at least one patient waiting 78 weeks (up from 134 last month); and 103 trusts had at least one patient waiting at least 104 weeks (up from 96 last month).
Diagnostics: Diagnostic activity increased in May 2021 but remains below pre-pandemic levels.
- The number of tests carried out in May 2021 has increased by 2.3% to 1.88 million (42,053 more). However, this is 5.3% fewer tests since May 2019. Compared to a year ago, there are 116.2% more tests carried out (1.05 million more).
- The number of MRI, CT and colonoscopy tests have all increased this month, by 4.5%, 3.2% and 7.7% respectively. Compared to May 2020, all of these have increased considerably by 116.4%, 51.7% and 578.9%.
- The diagnostic waiting list has increased by 3.4% to 1.31 million since the previous month, with 22.3% of people waiting six weeks or more for a test in May – missing the 1% target again this month.
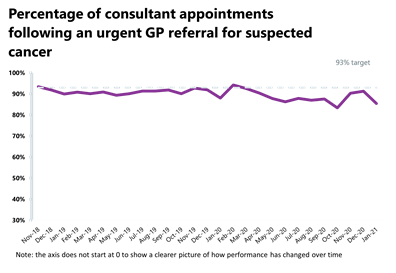
Cancer: Cancer activity is now at pre-pandemic levels; however, activity and performance have deteriorated slightly since last month and all targets have been missed.
- A total of 207,188 people were seen within two weeks of an urgent referral for a suspected cancer – this is down by 1.1% from the previous month which means that there were 2,264 fewer consultations. However, it is still 3.2% greater than two years ago which means activity is at pre-pandemic levels. 87.5% of urgent GP referrals were seen within two weeks, missing the 93% standard.
- The number of people on the 31-day pathway, which aims for one month between starting treatment following a decision to treat, also fell this month to 24,810. This is down by 0.6% since the previous month (153 fewer people). 95.1% of people started treatment within one month of the decision to treat, missing the 96% standard.
- The number of people waiting 62 days from urgent GP referral to starting treatment also decreased since the previous month to 12,999. This is 1.1% fewer than the previous month and a 7.1% decrease since this time last year. 73% of the people who started treatment did so within 62 days of their urgent GP referral, missing the 85% standard.
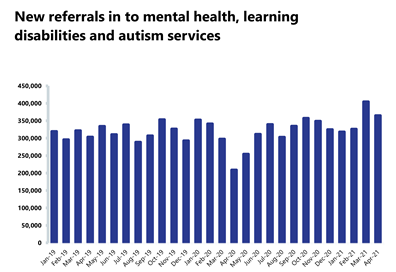
Mental health: Pressures on mental health services continue to rise, with the highest number of people in contact with mental health services since records began recorded in April 2021.
- In April 2021, there were 1.41 million people in contact with mental health services. This is 0.7% more than the previous week and 8.8% more people in contact compared to a year ago.
- The number of people being referred for mental health services fell by 9.9% to 364,691 since the previous month. Compared to last year, during the first wave of the pandemic, referrals have increased significantly by 74.6%.
- In April 2021, the number of out of area placements (OAPs) has remained at 700 (same as last month). Compared to the same point last year, there are now 245 more OAPs.
Our view
Today's figures reflect what trust leaders have been telling us over recent weeks. Alongside lockdown measures easing, they are witnessing demand for the majority of physical and mental health services increase. Referrals for elective and mental health care mean waiting lists continue to grow, despite the NHS doing all it can to increase activity.
The matter at the forefront of everyone's minds is how the current NHS pressures interplay with the impact of rising COVID-19 cases and the next easing of measures planned for 19 July 2021. We explore this issue in more detail here.
Impact of rising COVID-19 and NHS pressures
There is confidence among trust leaders that the vaccine has had a significant impact. The ongoing rise in community infection rates, even to the levels we saw in January, is not translating into the levels of hospitalisation and mortality we saw in that peak. However, the daily COVID-19 data already indicates that there will be more hospital admissions.
It is imperative that COVID-19 pressures on the NHS are not considered in isolation. The activity data published today shows the need to factor in demand and capacity of the NHS as a whole across physical and mental health services.
The activity the NHS can carry out is interwoven – pressures on one part of the system have an impact elsewhere. For example, each winter urgent and emergency care displaces a considerable amount of elective activity due to limited bed numbers.
Trusts are working hard to increase activity and are working flat out to recover care backlogs that they are now seeing across all their services. But there must be honesty about the huge pressure this is putting on staff, services and beds, particularly with COVID-19 activity rising once again.
The most recent sickness absence data published today for 30 June shows 68,512 staff absences in total, up by 27.7% compared to 31 May. On average in the past 7 days, COVID-19 absences accounted for 17.9% (11,509) of 64,289 total staff absences. As COVID-19 infections rise in the community, including the expected rise after 19 July, so will NHS staff absences as a result of infection or needing to isolate.
Therefore, even though trusts are likely to be able to cope with any expected rise in COVID-19 patients, NHS pressures must be seen from the broader perspective taking into account the cumulative impact of all the different factors at play. Staff shortages, the urgent pressure to clear the care backlog, the resources needed to treat people experiencing long COVID and the need to minimise growing health inequalities are all wrapped into the task at hand for trust leaders.
A&E


Cancer

RTT


Diagnostic tests


Ambulance indicators


Mental health

Case Study: University Hospitals Dorset NHS Foundation Trust
In June 2021, the theatres team of University Hospitals Dorset (UHD) won a Dorset Hero Award for best healthcare team. This highly-contested award, organised by our local newspapers the Bournemouth Echo and Dorset Echo, was given in praise of all that the team did during the last year, battling the COVID-pandemic, supporting our patients and each other, and all against the backdrop of being part of a merger in October 2021 of two major local trusts.
The theatres teams of Royal Bournemouth Hospital and Poole Hospital, now both part of UHD, worked tirelessly during this time to maintain urgent services, maintain cancer services and support colleagues in critical care.
In advance of our merger in October last year, our theatre teams were already working very closely together on plans following Dorset's clinical services review, run by the clinical commissioning group. These relationships that were well established before the merger were vital for dealing with all the events that occurred in 2020 and at the start of 2021. Future plans include making Poole the major planned care site and Royal Bournemouth the major emergency care site.
As with other hospitals nationally, at the start of the first lockdown in March 2020 we ceased elective work and switched to providing only emergency and trauma care in preparation to cope with any surge in COVID patients. This involved a steep learning curve as our theatre staff learnt to work in different ways, with new personal protective equipment guidelines. Our brilliant team also physically reorganised theatres to keep urgent cancer, trauma and emergency surgery running and to create more critical care space.
Thanks to the way staff responded and met all challenges with courage and enthusiasm, we were able to maintain life-saving surgery.
Thanks to the way staff responded and met all challenges with courage and enthusiasm, we were able to maintain life-saving surgery. Colleagues from Royal Bournemouth also further supported trauma in Poole by running additional theatres for urgent surgery. Rotas were also updated to allow us to double up our theatre teams enabling COVID-safe practice.

For our cancer services, we started working with the independent sector within one day. We already had a very close relationship with the sector and used local private hospitals in Poole and Bournemouth for cancer services and for some elective procedures where possible. We were supported in this work by NHS England and worked closely with the Dorset Integrated Care System to ensure we were all able to take the most from this opportunity. We also used the newly established Wessex Cancer Hub to help prioritise patients and move them to the most appropriate location for their care. We were fortunate to have great clinical buy in for this care, and the fact that our consultants were prepared to travel meant that our priority two patients were not compromised and received time-critical surgery.
During the first wave, 50 of our theatre team were redeployed to work in our critical care units. They had to learn new skills to support their colleagues and work as a very close team, as anyone who has been involved with proning a patient can attest. Their support was much appreciated.
Our staff also supported each other throughout these changes. Psychological support was in place, initially via occupational health and then via a bespoke drop-in clinic in theatre. We worked hard to ensure we had the support mechanisms to help staff members manage upheaval, change and the personal impact of the pandemic. Our theatre colleagues have shown flexibility, creativity and resilience during the last 18 months and we are very proud that all they achieved was recognised with the Dorset Hero Award.
Press Statement
Health staff addressing huge array of challenges
Responding to the latest monthly combined performance data from NHS England and NHS Improvement, the chief executive of NHS Providers, Chris Hopson said:
"Today's figures highlight the pressures the health service is under, as staff address a daunting array of challenges.
"In June trusts experienced record demand for urgent and emergency care. Trust leaders tell us they are seeing increasing numbers of patients with more complex conditions following the disruption caused by the pandemic, and they expect this to continue through the summer, ahead of what is expected to be a very difficult winter.
"Ambulance services are at full stretch, with over three quarters of a million call outs in the past month.
"Demand for community and mental health services is also worryingly high, particularly for children and young people's services.
"Trusts are working full pelt to meet this demand but there are shortages of beds and staff, and further capacity constraints because of continuing strict infection control measures.
"At the same time staff and volunteers are also rolling out the successful vaccination programme.
"There is a real concern that while COVID-19 hospitalisations are nowhere near as high as in previous waves, current pressures on the NHS mean that even a small rise in admissions will impact the ability to bear down on the care backlog.
"The government must continue to take this into account between now and next Monday when making the decision about whether to unlock restrictions."