Introduction
With the winter months approaching, COVID-19 pressures continue to escalate. Across England, there are over 5,200 patients in hospital with COVID-19 and the number of new cases has reached over 36,000 this week in England.
Many trust leaders have expressed their concerns over further increases in community infections and how this may impact on capacity and ability to provide non-COVID care. COVID-19 also accounted for 21% of all staff absences as of 6 October meaning it is still having a significant impact on the workforce.
The statistics published today highlight an incredibly busy month, with substantial pressures across clinical areas, particularly across the urgent and emergency care pathway, and mental health services.
This month's performance figures
Each month NHS England and NHS Improvement publish statistics looking at activity and performance across a range of services including urgent and emergency care, routine care, cancer, and mental health. Below we set out the latest trend for each clinical area:
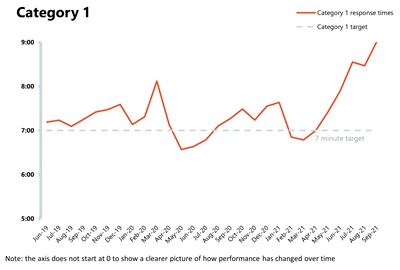
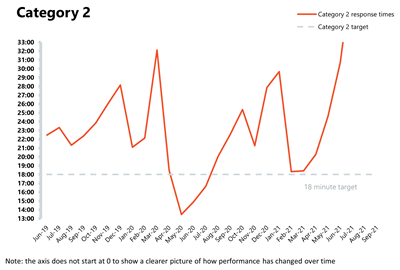
NHS 111 and ambulance: Ambulance category 1 incidents continue to increase, registering the highest figure on record in September. This highlights that demand and pressures remain elevated across the urgent and emergency care pathway.
- Ambulance category 1 incidents, those requiring immediate intervention and resuscitation, increased by 2.7% to 76,123 since the previous month (2,027 more incidents). Compared to two years ago, incidents have increased by 36.5%, underlining just how high the demand pressures continue to feel to frontline ambulance staff.
- The ambulance service has missed the average response time target of seven minutes for category 1 calls for the fifth consecutive month, registering the worst performance on record. Equally, the average response time for category 2 deteriorated, missing the 18 minutes target, and registering its worst performance on record as well.
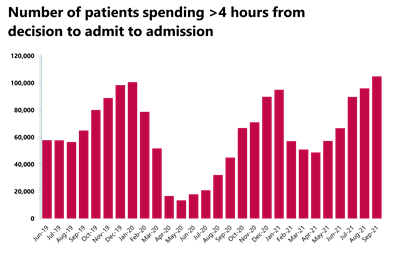
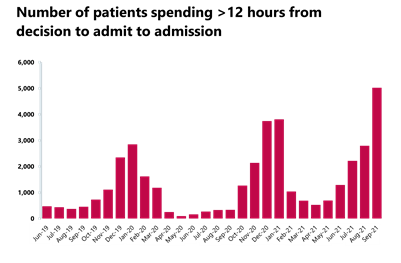
A&E and emergency care: the pressure across the emergency care pathway extends to emergency departments which is evident in the September data. Waiting times for patients have deteriorated and performance against the A&E 95% standard is at record lows. A particular concern for trust leaders is the number of patients waiting 12 hours to be admitted after the decision to admit.
- In September 2021, there were 2.12 million A&E attendances, an increase of 4.4% from the previous month, but very similar (-0.6%) to levels observed two years ago before the pandemic.
- There were 506,916 emergency admissions in September 2021 – a very small increase of 0.6% from the previous month but lower (-4.3%) than two years ago in September 2019.
- Performance against the 95% target for all A&E types drops by 1.82 percentage points from last month to 75.2%, making it the worst performance on record.
- The number of patients waiting longer than 4 hours has increased this month by 9% to 104,875 (8,862 more people), a figure 61% greater than two years ago. Equally, the number of patients waiting more than 12 hours also increased by 79.8% on last month to 5,025 (2,231 more). This is by far the highest number on record with the second highest being 3,809 in January 2021 at the height of that wave of the pandemic.
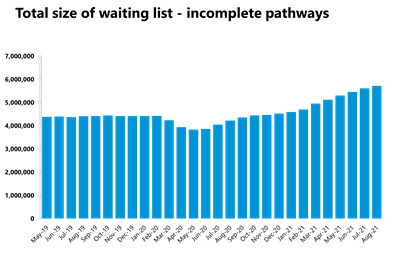
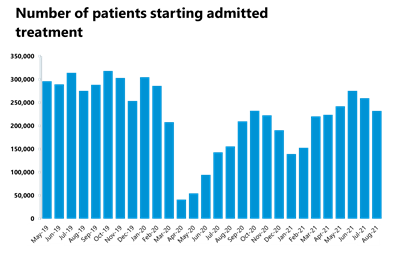
Elective care: referrals continue to outstrip activity as the waiting list keeps growing to the highest level observed in the last decade, reaching 5.71 million in August 2021. That said, trusts continue to reduce the number of long waits, with the number of patients waiting over 52 weeks decreasing for the fifth consecutive month.
- In August 2021, the size of the elective care waiting list increased by 108,974 to 5.71 million, representing an increase of 1.9% since July 2021. This is the highest level observed in the current records over the last decade.
- The number of patients waiting over 18 weeks increased again this month by 4%. With 71,091 more people now waiting than the previous month, the performance against the 18 weeks standard has fallen by 0.6 percentage points to 67.6%.
- The number of people waiting 52 weeks or more has decreased for the fifth consecutive month by 0.3% from July 2021. That said, this figure is still 163% higher than the same time last year.
- Inpatient care activity has decreased in August 2021: the number of admitted inpatient pathways decreased by 10.6% compared to the previous month, meaning that a total of 232,140 inpatient treatments were conducted.
- For non-admitted pathways, the figures also decreased by 9.5%, with the NHS delivering 904,810 elective non-admitted pathways.
- There were 1.469 million new RTT pathways in July, a decrease from the previous month. This results in the overall size of the waiting list growing because new referrals are still outstripping activity.
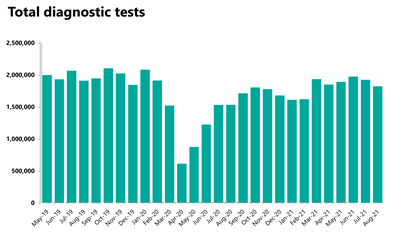
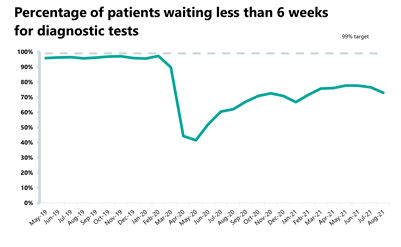
Diagnostics: diagnostic activity decreased in August 2021 and remains below pre-pandemic levels. However, the waiting list has decreased since last month.
- The number of tests carried out in August 2021 has decreased by 5.3% to 1.82 million (102,166 fewer) compared to July 2021. Compared to two years ago before the pandemic, 4.5% fewer tests were carried out (86,439 fewer).
- Compared to last year, the number of MRI, CT and colonoscopy tests all increased by 19.5%, 11.9% and 37.7%, respectively. When looking at diagnostic activity from August 2019, before the pandemic, the number of MRI tests is down by 1.5% (4,662 fewer), the number of CT tests increased by 9.4% (48,884 more), and the number of colonoscopy tests decreased by 3.6% (1,638 fewer).
- The diagnostic waiting list has decreased by approximately 2% to 1.36 million (22,276 fewer) since the previous month, with 27.1% of people waiting six weeks or more for a test in August. This figure is slightly up from 23.5% last month but still missing the 1% target again this month.
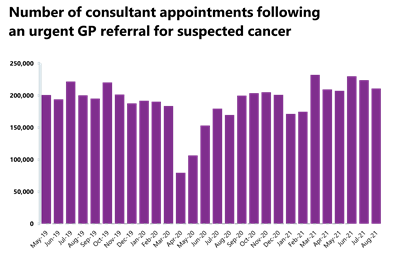
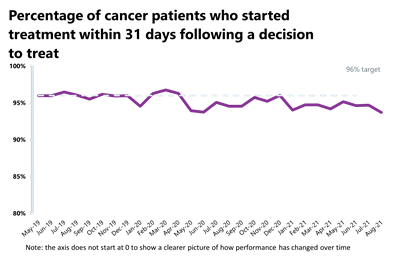
Cancer: even though activity is roughly at pre-pandemic levels, performance against the waiting time standards has slipped slightly meaning the NHS is missing all key national targets.
- A total of 210,931 people were seen on the two weeks from an urgent referral for a suspected cancer pathway – this is a decrease of 5.9% (13,155 fewer consultant appointments) compared to the previous month. This number is 24.3% greater than the same time last year during the pandemic and higher (5.3% greater) than two years ago before the pandemic. 84.7% of urgent GP referrals were seen within two weeks, a decrease in performance from the previous month and missing the 93% standard.
- In August 2021, 25,900 people completed the 31-day pathway which aims for one month between starting treatment and the decision to treat. This was 1,272 fewer people than the previous month – a decrease of 4.7%. Activity is 27.9% lower than one year ago, but 0.1% lower than two years ago before the pandemic. 93.7% of people started treatment within one month of the decision to treat, meaning a slight decrease in performance compared to the previous month, again falling short of the 96% standard.
- Those completing the 62-day wait from urgent GP referral to starting first cancer treatment pathway also deteriorated compared to the previous month. 13,927 people completed the pathway, a decrease of 3.2% from the previous month, yet this figure has increased by 24.4% from one year ago and increased by 2% from two years ago before the pandemic. Performance this month is at 70.7% of the people who started treatment doing so within 62 days of their urgent GP referral, representing a decrease from the previous month and missing the 85% standard.
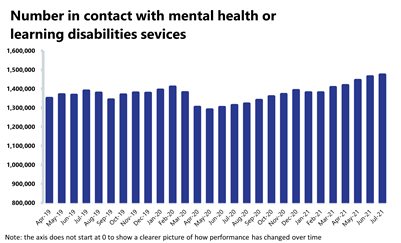
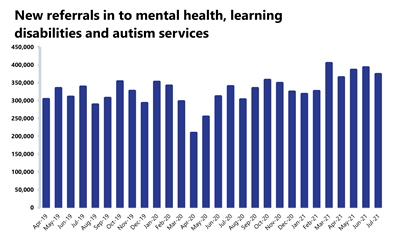
Mental health: the number of people in contact with mental health services continues to increase each month, with contacts at their highest level. Referrals have fallen slightly this month, but remain 10.4% higher than pre-pandemic levels.
- In July 2021, mental health referrals fell by 4.9% to 373,504 (19,199 fewer referrals). Compared to a year ago, referrals have increased by 10% (33,982 more referrals than July 2020). In comparison to two years ago, referrals have increased by 10.4% (35,171 more referrals than July 2019).
- The number of people in contact with mental health services has increased by 0.6% to 1,47 million since the previous month (8,937 more people in contact). This is the highest number of people in contact since records began. Compared to a year ago, there are 12.2% more people in contact with mental health services (160,028 more people in contact). In comparison to two years ago, there are 6.1% more people in contact (84,082 more people).
- In July 2021, there were 2.06 million care contacts attended (down by 2.2% and 46,558 fewer than the previous month). Compared to a year ago, there are 1.6% fewer care contacts (33,524 fewer). However, compared to two years ago, there are 6.8% more care contacts (131,177 more).
- In July 2021, the number of out of area placements increased to 730 (35 more OAPs than last month). Compared to a year ago, OAPs have increased by 23.7% (140 more OAPs). Compared to two years ago, OAPs have fallen by 6.4% (50 fewer OAPs).
Our view
This month's data show, once again, how tirelessly NHS staff are working across physical and mental health services, juggling COVID-19 pressures with non-COVID care. Trusts are facing a significant challenge as we head into the winter months, with pressure constantly increasing throughout many clinical areas.
The urgent and emergency care pathway continues to be remarkably busy, with demand increasing by 37% compared to the pre-pandemic period for category 1 ambulance calls. If emergency care demands further increase throughout winter, this could impact trusts’ ability to deliver the sector’s elective care recovery ambitions.
Additionally, trusts are experiencing larger waiting lists for planned care and the highest number of people in contact with mental health services since records began. However, in the face of these challenges, NHS staff are pushing hard and increasing activity, balancing the treatment of COVID-19 patients and urgent and emergency patients, alongside dealing with the backlogs of care across physical and mental health services.
These data highlight how trusts have continued reducing long waits, with the number of patients waiting over 52 weeks decreasing for the fifth consecutive month, and the waiting list for diagnostic tests falling for the first time this calendar year. Cancer services are also running at similar levels of those -pre-pandemic. These are positive achievements and testament to the hard work of frontline staff.
Trust leaders are still extremely concerned about further rises in demand as winter approaches, alongside the expected seasonal flu, norovirus and anticipated increases in respiratory syncytial virus infections (particularly among children), all of which were considerably absent in 2020. These unpredictable demand pressures, alongside possible COVID-19 increases, heighten the risk across systems which trusts will have to manage this winter.
The government's funding announcement last month provided a critical and much needed boost but trusts will need more support and resources in the longer term, including a fully funded workforce plan and a capital settlement designed to improve access to treatment, bear down on the backlog of care and transform services.
Somerset NHS Foundation Trust
Peter Lewis, chief executive of Somerset NHS Foundation Trust
Somerset NHS Foundation Trust has worked with Rutherford Diagnostics Limited to open a new state-of-the-art diagnostics centre which will serve NHS patients from across Somerset.
The centre will give patients increased access to diagnostic tests which inform their treatment and enable them to have their diagnostic tests in a stand-alone modern facility away from a busy hospital.
The Rutherford Diagnostic Centre Somerset in Taunton is the first community diagnostics centre of its kind in England – run by Rutherford Diagnostics Limited, a subsidiary of Rutherford Health PLC, as a result of a partnership with Somerset NHS Foundation Trust.
Rutherford Diagnostics Limited will provide diagnostic services from the Rutherford Diagnostic Centre Somerset which offers magnetic resonance imaging (MRI), computed tomography (CT), ultrasound and x-ray on equipment provided by Rutherford's technology partner, Philips.
This is a fantastic facility for patients in Somerset and the surrounding areas. We entered into our partnership with Rutherford Diagnostics Limited in June 2020 because, despite our investment in MRI and CT scanners, and our continued use of mobile scanners, we were concerned that our trust would not keep pace with demand for diagnostic tests in the future. We had to look for a different solution and were delighted to enter into our partnership with Rutherford Diagnostics.
As a result our patients have access to diagnostic tests at this modern stand-alone facility away from a busy hospital. This is part of the new recommended way forward for the NHS and has become more important as a result of the global pandemic. It also brings real benefits for our radiology, radiographic and booking colleagues who will be working alongside Rutherford's staff in the centre, enabling them to work in more diverse environments and expand their experience.
The centre also helps us to prioritise the capacity that we have available at Musgrove Park Hospital for emergency patients or those who are already in the hospital. This is not only good for our patients, but also the way we care for people across the whole Somerset healthcare system by enabling them to have imaging scans away from the acute hospital.
The centre, run by Rutherford Diagnostics, is the first of up to five centres that Rutherford intends to develop under an agreement between Rutherford Health plc and Equitix, a leading investor, developer and long-term fund manager of core infrastructure and energy-efficient assets in the UK and Europe. Philips will provide the innovative technology at the five sites.
The additional capacity at the Rutherford Diagnostic Centre Somerset enables Somerset NHS Foundation Trust to increase its CT capacity by a quarter immediately and its MRI capacity by a quarter within three months and scan a larger proportion of patients who require complex scanning. NHS organisations in Somerset are planning to provide 99% of patients with diagnostic imaging within the six week national standard by March 2022 subject to waiting lists remaining steady and the NHS will monitor its progress closely.
Davinia Fox from Wellington was the first patient to be seen at the new Rutherford Diagnostic Centre. She said: "I'm thrilled to be the first person seen at the new diagnostic centre. The centre is so accessible and I found it so much easier to get here and not to have to worry about the parking at Musgrove Park Hospital, which was a real weight off my mind. The new building is so spacious and I found the staff really friendly – I had much less of a wait for my scan and I couldn't fault the care I received. I'm so grateful for everything they have done for me."

A&E
Cancer
RTT
Diagnostic tests
Ambulance indicators
Mental health
Trusts in extremely challenging position as winter approaches
Responding to the latest monthly combined performance data from NHS England and NHS Improvement, the deputy chief executive of NHS Providers, Saffron Cordery said:
"Today's figures demonstrate the extremely challenging position trusts are in as we head into winter.
"Ambulances are under incredible strain, with demand amongst the most seriously ill patients rising by a staggering 37% compared to before the COVID-19 pandemic.
"This pressure is being felt across urgent and emergency care. There are worrying delays for patients, with over 5,000 people waiting over 12 hours to be admitted into hospital. Referrals for mental health services are far higher than they were before the pandemic and demand for community services continues to be a major concern.
"However, it is important to recognise the professionalism and commitment of NHS staff, who have given so much through the pandemic and are working hard for patients in these exceptionally difficult circumstances.
"Waiting lists for planned surgery have reached a new high of 5.7 million but there are hopeful signs this rise is starting to plateau, and there is some evidence of progress in bearing down on the longest waits, alongside the focus on the most urgent cases.
"But trusts need more support and resources as we head into what is expected to be the most difficult winter on record for the NHS. We must not forget that we are facing a 'twindemic' this year, with both COVID-19 and flu in circulation for the first time.
"This month's comprehensive spending review presents an opportunity to put health and care on a sustainable footing. We need a fully costed and funded workforce plan to recruit and retain more staff, and a multiyear capital settlement, including funding to invest in digital transformation.
"National bodies also need to be realistic about the challenges ahead when targets are set for recovering the backlog of care, with the majority of trusts saying it will take two to five years."