Commentary
Context
Trusts and their staff continue to face a challenging context in which they must manage local surges in positive cases and resume previous non-COVID treatment, as set out in the phase three recovery plan from NHS England and NHS Improvement.
The NHS is open and available for all those who need care and treatment. However with infection rates rising swiftly in some parts of the country, every individual must play their part in regular hand washing, and adhering to social distancing rules and local restrictions.
Following the first wave of the pandemic, trusts across England have been working hard to deliver services safely. As our case studies demonstrate, frontline staff have been rolling out innovations in all corners of service delivery in response to the challenges presented by COVID-19.
In this second edition of our, Restoring Services: NHS activity tracker, we offer our commentary on the monthly, publicly available performance data and share detailed case studies of innovations developed by trusts and their staff.
This month’s performance figures
Each month NHS England publishes statistics looking at performance across a range of services including urgent and emergency care, routine care, cancer, and mental health. The data this month shows a complex and nuanced picture across services.
When reviewing the national data it is important to remember that at the moment the trends across the country are not uniform. Confirmed COVID cases are increasing nationally, but trust leaders are reporting different experiences of local surges in different parts of the country based on the numbers requiring hospital admission. Furthermore, as cases rise and more local lockdown restrictions are introduced, we may expect the way the public interacts with the NHS to change as we did in the first peak of the pandemic.
Below we highlight some of the latest trends and figures in both areas.
NHS activity
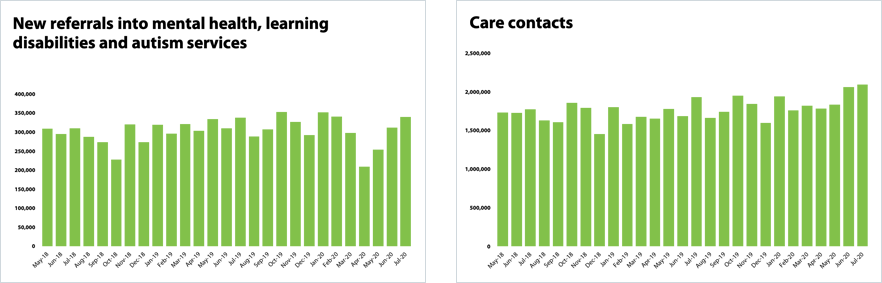
- Demand and activity for mental health services is at an all time high. The number of care contacts provided by mental health trusts is the highest since records began at 2,096,013 in July 2020. In the same month, referrals to mental health services increased by 9% to 339,522 since the previous month.
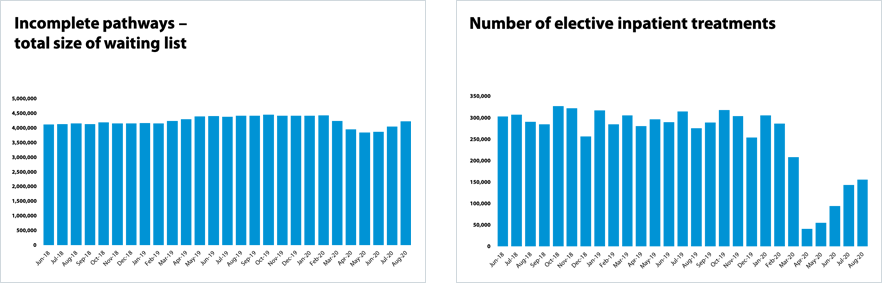
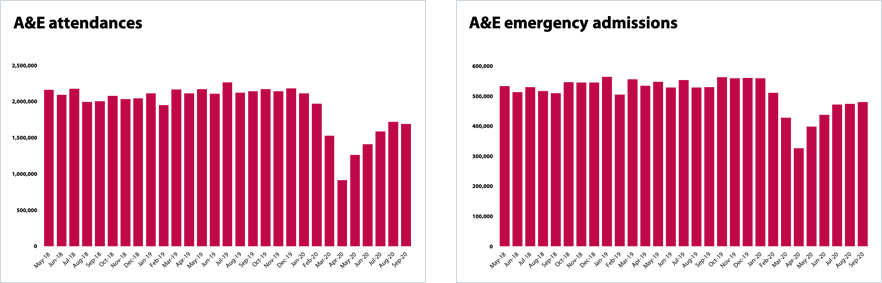
- A&E departments saw a reduction in footfall in this period but a rise in emergency admissions. A&E attendances fell slightly by 1.6% from last month to 1.69million - 21% lower than in September 2019. But attendances are still up 85% on the levels observed in April 2020. Emergency admissions increased from last month by 1.2% to 479,800 – and are only 9% lower than September 2019. Emergency admissions have increased by 47% since April 2020The number of elective care operations increased by 9% from July to August and has increased by 279% since April. There has been month on month improvement with more elective activity taking place since the low of 41,121 operations in April.
- The number of 111 calls continues to increase for the third consecutive month - 1,792,507 calls were offered. This is an increase of 7.3% since the previous month (122,091 more calls offered) but still 39.5% lower than in March 2020 when we saw NHS 111 under immense pressure due to the COVID guidance at the time. However, activity remains 36% higher than at the same time last year.
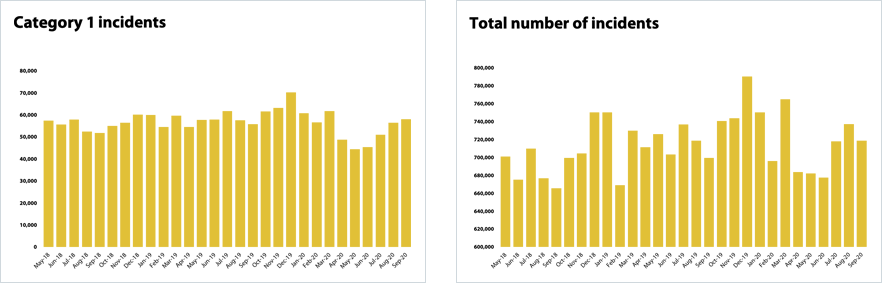
- Ambulance Category 1 incidents continue to increase and are higher than this time last year with 57,967 incidents in September. Category 1 activity has increased by 4% compared to the same month last year and all incidents have increased by 2.7%.
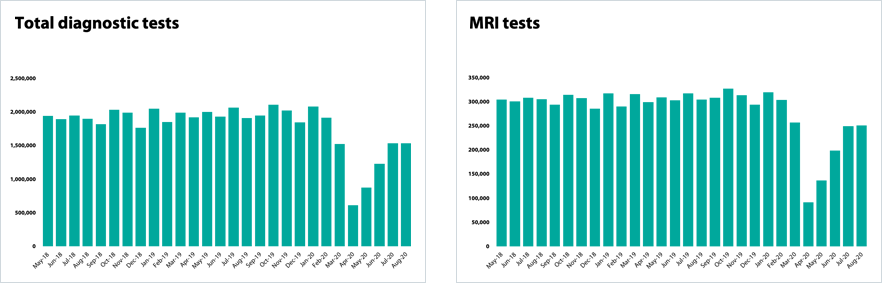
- Diagnostic activity is very similar to last month and remains some way below the level a year ago. 1.5 million diagnostic tests were carried out, an increase of 0.1% on the previous month. Some improvements were made in colonoscopies which see a 14% increase in activity in August.
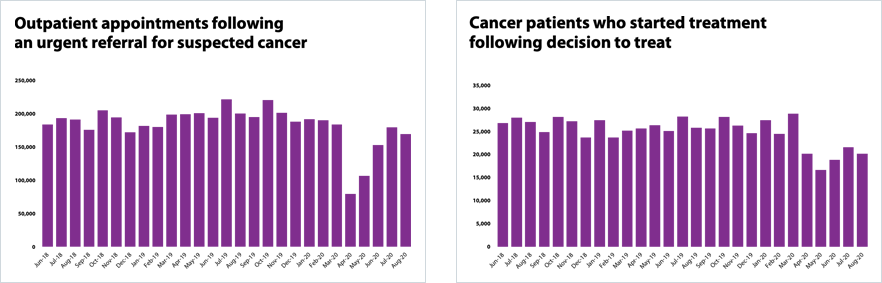
- Cancer activity has dropped from last month and is still some way below pre-pandemic levels. There were 5.5% fewer appointments for a suspected cancer in August than in July. This is 15% lower than at the same time last year.
NHS waiting times
- Performance against the 95% A&E standard slipped from last month, falling to 87.3% in September down from 89.3% the previous month. In addition, 333 patients waited longer than 12 hours from the decision to admit to admission – a small rise of 2% on the previous month.
- The number of people waiting over 52 weeks has now exceeded 111,000 – an increase of a third (33%) since last month and of 905% since April. The size of the elective care waiting list increased by 173,408 to 4.22 million in August. Although the waiting list grew by 4.3% since July 2020 it is still smaller in size that it was pre-COVID-19 (4.43million in February).
- Performance against 18 week elective care standard has slightly improved to 53.6% in August from the all-time low of 46.8% in July.
- The ambulance service missed both category 1 and 2 time standards. The service missed the category 1 target of 7 mins with a national time of 7 minutes and 16 seconds. This is a deterioration on last month and the worst performance in six months reflecting increasing demand.
- Mental health trusts have seen more people than last month within the six week standard for talking therapies. In July 2020, 87.5% of people started Improving Access to Psychological Therapies (IAPT) treatment within 6 weeks, an increase of 1 percentage point since the previous month.
- Waits for diagnostic tests are still long but not getting worse. 0% of patients were waiting six weeks or longer, a slight improvement from 39.6% last month but a long way off the operational standard of less than 1%.
- Performance against key cancer standards slipped with the sector missing some of the main waiting time standards. 8% of people were seen within two weeks following a suspected cancer referral, missing the 93% standard; 94.5% of people started cancer treated within 31 days following a decision to treat, missing the 96% standard.
Our view
The NHS activity and performance data published in October reflect the pressures trusts are under as they seek to restore services and activity levels. Activity levels including the number of A&E emergency admissions, diagnostic tests, operations and mental health referrals and care contacts have all increased again month on month.
Trusts are doing all they can to restore elective care as swiftly as they can, prioritising waiting lists based on clinical need, working collaboratively to help manage the backlog, and maximising use of the independent sector where possible. NHS England confirmed in its board meeting last week that the acute sector had met the phase 3 objective of conducting 80% of September 2019 overnight elective activity in September 2020. This was a stretching target and it is testament to the focus and dedication of frontline staff including surgeons, theatre staff and operational managers to step up activity to this level in such a short space of time.
However, the progress in some services is slower in part down to the nuanced and complex nature of local COVID-19 surges impacting services differently. For example, the national aggregate figure shows that fewer people are attending emergency departments. We also note that the pace of cancer activity recovery has begun to slow compared to previous months.
Demand heading into winter
With testing and infection survey data showing a marked increase in COVID-19 cases, trusts are concerned about the potential challenges the next few months may present and the impact this will have on frontline staff.
The data published in October covers September and August. However, anecdotally trusts are also already signalling that they are beginning to see demand for most services grow with pressure building across the urgent and emergency care pathway in the first few weeks of October. Trust leaders tell us this reflects local COVID-19 surges but that, in some parts of the country, the majority of presentations are people unwell with common non-COVID seasonal illnesses.
Alongside system partners from all sectors, trusts will continue to manage the increases in demand in a very different environment this year. With social distancing measures in place, more time required for donning and doffing additional personal protective equipment and increased infection prevention control measures, frontline staff will feel every squeeze on their time more than ever this winter.
Key examples of sustained demand pressures include:
- Ambulance trusts tell us they have significantly increased the number of incidents in which they offer their hear and treat and see and treat services - all in an effort to intervene at the right time and help reduce the pressure on acute hospitals. Ambulance trusts that deliver NHS 111 services are also working with acute hospitals and other system partners in the piloting of NHS 111 First which aims at directing unnecessary physical presentations to A&E over winter to better manage demand.
- Community trusts tell us the level of palliative care they are providing has increased in recent months resulting in an increase in complexity of case mix. This is supported by the fact that deaths in private homes has remained well above the five-year average for the past few months, thought to be a result of more people choosing to die at home. Community service providers are also catering for a range of rehabilitation needs outside of hospital settings as they continue to support acute colleagues in ‘discharge to assess’ models.
- Trust leaders tell us demand for mental health services is at an all time high. This is supported by the evidence today which shows mental health trusts are providing a greater number of care contacts than ever before. Many trust leaders predict a continued surge in demand and acuity of people seeking support for mental health conditions often related to the socioeconomic impact of COVID-19 with conditions exacerbated by isolation and loneliness as well as increasing unemployment.
Collaborative working and innovative solutions
In a recent survey of trust leaders, 92% said that the experience of COVID-19 had accelerated better partnership working across systems, and this is reflected in collaborative efforts to restore services. These relationships will be vital in how the sector will manage the risk it is carrying over the next six months.
As our case studies highlight, the restoration of services is down to the energy and commitment of frontline staff to do all they can to make sure as many patients are receiving the care they need as soon as possible. Without diminishing the challenges ahead, we must recognise the progress the NHS is making in uncertain times as we head into winter 2020-21.
NHS activity tracker
Mental health services
Cancer services
Elective care
Diagnostic testing
Urgent and emergency care
Ambulance services
Case studies
Northamptonshire Healthcare NHS Foundation Trust
James Mullins, Assistant Director of Clinical Quality
Northamptonshire Healthcare NHS Foundation Trust has curated an innovative system which ensures the robust distribution of PPE to all clinical and non-clinical staff across a mental health and community NHS trust that spans a large geographical area. This has enabled us to protect staff, patients and visitors during the COVID-19 pandemic.
The model was developed to successfully manage the allocation, distribution and maintenance of PPE across the trust and is being used as a benchmark for other NHS trusts across the country to share best practice, and key learnings. The model was developed by James Mullins, assistant director of clinical quality, and Alex Quinn, contract manager.
The trust covers a 150-mile radius with staff working across more than 40 sites in Northamptonshire, Bedfordshire, Cambridgeshire and Staffordshire. It was vital to have an accessible and robust process in place to maintain over 30 types of PPE in all service areas and enable healthcare professionals to continue to provide outstanding and compassionate care with ease. So far, the system has successfully distributed more than 3.5 million pieces of PPE across four counties. This includes over 50,000 Type IIR masks dispatched per week.
Using quality improvement methodology, the team collectively explored the best way to create a system that ensured safety and efficiency for frontline teams. The system enables colleagues to monitor stock levels and allocate and distribute PPE across the trust. Based on the ‘push model’, it holds robust data that can quickly pull reports to efficiently manage PPE distribution and if required can enable recall of products. This data provides essential reports and live data analysis to the trust’s incident control centre on performance and to NHS Improvement.
Since the introduction of the new system, the trust has seen a reduction in ad-hoc orders by 80%, with weekend requests for stock averaging between 0-5 email requests to a central mailbox, where no urgent PPE has been required in recent months. Crucially, the team have enabled a trust wide cohort of PPE champions in each service who provide daily updates on usage and stock take which feeds into the push model and gives overall and accurate data.
Alex explains: “Safety is one of our core principles, and it is vital that we implemented a system which would enable us to effectively manage and maintain PPE across the trust. The ‘push model’ enables clinical staff to continue to provide outstanding care, while we work with our operational staff to distribute and monitor PPE, keeping our staff and patients safe. We are continually reviewing the system to ensure that it evolves to meet the needs of the trust.”
James has overseen PPE since the new system was implemented in March, he added: “The system is easy to navigate and provides staff with accurate and up to date information, allowing them to quickly access data or make a request for information. Clinical staff are delivering outstanding care during a challenging time, and it was important that we ensure that they had the right PPE to keep them and our patients safe. We are working with partners regionally and nationally to continually manage our PPE in line with any changes, and the system enables us to quickly and efficiently distribute PPE across the county.”
Julie Shepherd, chief nurse at Northamptonshire Healthcare Foundation Trust, said: “Our PPE service has been and continues to play a vital role in keeping both our staff and our patients safe during the COVID-19 pandemic. This model has been developed and delivered by a group of staff who have come from many areas of the trust using their skills and knowledge to deliver an important service. Everyone in the team has a role to play from those working in the services to the trust drivers who deliver the PPE out to our services and PPE champions in our services.”
Northumbria Healthcare NHS Foundation Trust
Marion Dixon, Executive Director of Nursing
The COVID-19 pandemic has encouraged Northumbria Healthcare to look at new ways of connecting with patients and make appointments more convenient across a large geographical area. The trust is responsible for the care of patients across a large part of Northern England from the border of Scotland right down to North Tyneside.
Due to coronavirus, there has been a surge in the patients accessing virtual appointments. This use of technology has helped ensure continuity of care and has provided a safe and convenient approach to appointments for many of our patients.
Prior to the pandemic, between 10% to 20% of outpatient appointments at the trust were done digitally, by video or telephone consultation, however by the end of July, this increased dramatically to 60% and equated to almost 55,000 appointments - a significant increase compared to the same time last year where only 7% of outpatient appointments were done via these methods (around 10,000 appointments).
Better use of digital technology has not only meant care has continued to be delivered for patients but has also saved patients travelling thousands of collective miles to appointments. In fact, the technology has more than halved the average number of miles travelled per patient in two years from 16.9 miles to 7.2 miles. This means that in total, our patients have been saved from travelling almost 900,000 miles with an associated environmental benefit.
Charlie, 64, is one of thousands of patients who has been assessed by video call or over the phone as non-urgent appointments and operations were postponed due to COVID-19. Charlie was diagnosed with Parkinson’s Disease in May on a video call with nurse consultant Annette Hand.
“I felt so much more comfortable being able to see Annette and her happy, smiling face than I would have done over the phone. I felt so much more relaxed being able to remain in my own home and not have to travel, whereas travelling from where I live could have taken hours. With the lockdown I was worried that I would have to wait months to be seen but I had my video call only a week or so after I was referred by my GP. I was surprised by how quickly it happened. I couldn’t recommend virtual appointments more and I hope that even after coronavirus people use it as I think it’s the way forward.”
During lockdown, Northumbria Parkinson’s service made full use of ‘Attend Anywhere’ – and waiting times have reduced from three to four months pre-pandemic to two weeks now, diagnosing a number of patients like Charlie.
We receive around 60 new referrals a month and rely on being able to see patients to assess them properly. The last thing we wanted to do was to have them wait longer for a diagnosis.
Parkinson’s remains very much a clinical diagnosis and we rely on not only what the patients tell us but also on how they look, move and present on examination. ‘Attend Anywhere’ has enabled clinicians to still see patients face-to-face and provide a diagnosis.
The technology also enables patients to have a relative or friend log in to the video consultation if they want them to, just as they would attend an appointment with them in person, ensuring they are not alone.
‘Attend Anywhere’ is being used across the trust for hospital and community services throughout Northumberland and North Tyneside. 98% of patients who used it to access talking therapies in North Tyneside for help with conditions such as anxiety, depression, stress and phobias said they would use it again with the technology. This technology is in turn also reducing non-attendance rates.
Nottingham University Hospitals NHS Trust (NUH)
Tracy Taylor, Chief Executive
I am so proud of team NUH, they continue to astound me with their use of innovation, teamworking and dedication to restore services as quickly and as safely as possible for our patients. Staff have taken creative approaches to tackling the pandemic head on in so many different areas of service provision. There are many examples I want to share to demonstrate how we are doing this at NUH.
Since the height of the pandemic, we have increased the number of outpatient appointments using our Dr Doctor video consultation tool. This has reduced the number of face-to-face appointments, allowing us to follow social distancing guidelines and has enabled our clinicians to work remotely, while giving patients access to the treatment and advice they need without coming into hospital. In addition to video consultations we’ve armed our consultants with e-outcoming, e-vetting and e-clinical noting functionality so that despite consulting remotely they are supported in the process with the right tools to do their job effectively.
Prior to the pandemic, radiology reporting from home was not commonplace. However, since the pandemic, we have provided our radiologists with the necessary IT kit and system access to report from home. Turnaround times have reduced and when reporting a high volume such as plain film, radiologists can move quickly through the work list without disruptions. This allows us to restore more services for patients and enables us to reduce our waiting lists.
In A&E, we developed our systems so the acute medicine team can telephone triage patients from home or anywhere within the hospital and it automatically e-mails the referral to the acute medicine reception e-mail inbox so the receptionist/nurse in charge is notified of an upcoming patient arrival ensuring that patients get to the right place, first time round.
For patients that are ready to be discharged, we have agreed a medically safe fit for discharge target across system partners, where we are moving from an average in 19/20 of around 175 patients to a target of less than 75 absolute supported patients (37 for >24hr). We have also established a Greater Nottinghamshire discharge HUB to enable collective flow/discharge management across the system, ensuring we have enough beds for our elective services to increase activity.
To continue to restore our elective activity, we have worked with the independent sector. Different solutions were needed, alongside the appropriate information governance sharing agreements. The deployment of laptops and the creation of sharing agreements and honorary contracts has allowed 700 elective NHS operations to be carried out using capacity in the independent sector.
Our commitment to research and innovation has helped to ensure that life-changing patient care can return safely. A team of clinical researchers, working with ear, nose and throat (ENT) surgeons and medical manufacturers have created an innovative plastic drape which is designed to create a protective barrier or ‘tent’ between the theatre team and the patient’s head and upper torso. This is now in use in our ENT operating theatres at the Queens Medical Centre for cochlear implant surgery, allowing our surgical teams to take a lead nationally in efforts to re-start these important procedures safely.
We are determined at NUH to come out of this ‘safer, smarter and better’ than before COVID-19 and team NUH continues to be a force for good, in times of uncertainty.
Sherwood Forest Hospitals NHS Foundation Trust
Simon Barton, Chief Operating Officer
At Sherwood Forest Hospitals NHS Foundation Trust, we began thinking about restarting elective care in April.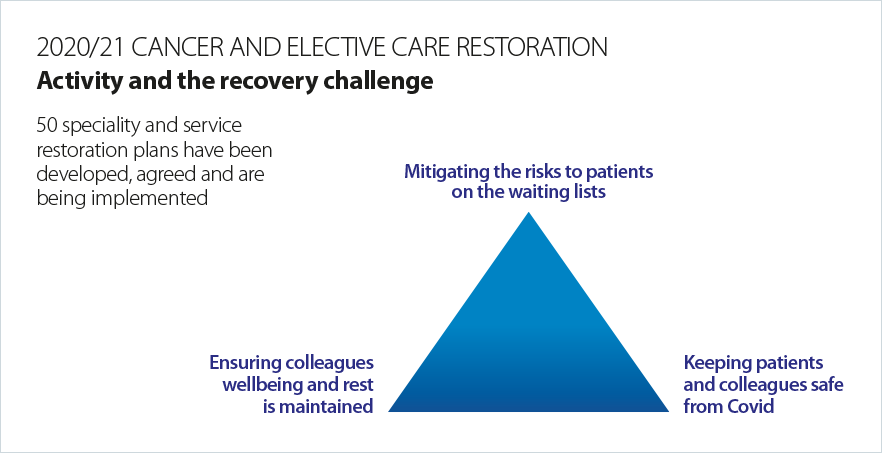
We worked closely with our tertiary partner, Nottingham University Hospitals NHS Trust and primary care colleagues to continue to provide as much cancer care as possible. The clinical decision making was swift and decisive, ensuring patients were reviewed, alternative treatment decisions were made to reduce risk for patients and Sherwood colleagues, and we continued to operate if it was safe to do so. We have always been dedicated to providing cancer patients with the best possible care and colleagues worked even harder during this period to treat high risk patients wherever possible. We were fortunate the local independent sector had critical care capacity and we worked with them to provide cancer care for high-risk patients.
Despite the actions taken above, the number of patients waiting for cancer care and the length of their waits grew during the first wave. In the early stage of restoration, we prioritised cancer patients and pathways and it was a key priority to get diagnostic capacity back up and running. It was the focus on diagnostics that helped us to rapidly reduce the backlog of patients waiting over 62 days. It was important we could quickly give the 93% of patients who did not have cancer peace of mind, while providing a treatment date to those who had their operations or treatment delayed because the COVID risk outweighed their clinical risk.
As well as restoring services, we had to help patients understand the risks of them not coming to hospital might be greater than the risk of them attending. We did this by working with local media, writing to all patients and by hosting virtual Q&A sessions for patients to raise their concerns.
The critical factor for restoring elective care was ensuring we had adequate PPE. Making sure colleagues and patients were as safe as they could be was our main priority. We have an outstanding procurement team at Sherwood who provided a usage forecast three times a week. This helped us always have sufficient access to timely and appropriate PPE. We followed national infection prevention control (IPC) guidance as a minimum standard and, in some areas, this reduced the number of patients that could be treated. To respond to this, we worked on changing our operating model, where we continued to use the independent sector. We redesigned the theatre timetable and we created a green operating site at Newark Hospital for the reintroduction of orthopaedic elective surgery.
As with PPE, our local IPC experts have been incredible. Their testing has been essential for recovery and our microbiology team have developed platforms and work 24/7 to ensure there is adequate testing and results are received in a timely way.
In outpatients we worked with clinical colleagues to enable them to offer patients face to-face appointments, telephone consultations or virtual appointments.
One of the most difficult elements has been asking colleagues who gave so much during the first wave to do it again this time round as we head into winter. Some colleagues were redeployed to areas such as critical care and did not take any annual leave during the first wave. Many colleagues have needed a lot of support and we have regularly debriefed to understand their experiences. We have focused relentlessly on meaningful actions to support the welfare and wellbeing of colleagues.
The people who work in the NHS make it what it is. I may be biased, but I think the colleagues at Sherwood are some of the most caring I have ever encountered. Their hard work and compassion held the organisation together through the pandemic and it has supported the on-going recovery of services for elective and cancer patients.
University Hospitals Plymouth NHS Trust
Linda Boorer, Lead Transplant Nurse Consultant
The South West transplant centre is a regional centre offering a service for kidney patients across Plymouth, Cornwall and the South of Exeter. We provide both a deceased and living donor programme and currently follow up approximately 400 patients who have been transplanted. National statistics show we have one of the lowest waiting times in the country with most patients waiting around 18 months before receiving a kidney transplant.
COVID -19 presented the centre with many challenges. Intensive care beds normally used to care for our donors were potentially needed for vulnerable patients requiring specialist treatment as a result of COVID-19. In addition, newly transplanted patients who are given high levels of immunosuppressive medication were extremely vulnerable if exposed to the virus.
In April, following extensive discussions with other centres, our own referring centres and NHS Blood and Transplant we made the decision to temporarily close our programme in the best interest of our patients. Two months later we gradually re-opened the programme, activating patients back onto the transplant waiting list in phases with national guidance. Under the direction of Dr Imran Saif, lead director for transplantation, the medical, surgical, immunology and nursing staff have worked incredibly hard to ensure the programme was reopened while taking every measure to ensure the safety of our patients.
The transplant waiting list had been growing and since reopening we have successfully transplanted 20 patients across our region. This is an incredible achievement for all those involved in the programme and life changing for those patients returning home with a new transplant who can now avoid the prospect of returning to, or starting, dialysis.
This has been a combined effort from many different services across the hospital, the renal unit (Mayflower ward) and support from the trust management has ensured a safe environment for patients returning to the ward following surgery. Other services such as microbiology have been working hard in the background to swab patients and staff both routinely and in emergency situations to minimise the risk of infection from the virus. The support of the theatre and radiology departments has ensured the timely assessment and transplantation of patients.
We would like to thank our on-call team and our immunology team in working together successfully to maintain the on-call rota during this period. This meant they had to still take potential screening offers so that patients from other centres could be seen while also maintaining our own patient list. The transplant team have also pro-actively managed both the suspension and re-activation of recipients in a short space of time and provided reassurance and information to anxious patients and their families.
Patient, Trudy said: “I was sitting in the sunshine sipping a glass of white wine when I got the call. It was Wednesday, 29th July at 5.30pm. Owing to COVID-19, the transplant list had been suspended. I had been reinstated on the newly opened list just two days beforehand. A rush of excitement and tears of joy ensued. I had been waiting for this call for almost three years due to antibody issues. Arriving at the Mayflower Ward, firstly I was tested for COVID-19. I am so grateful to the team who operated on me and everyone who continues to take care of me post-op. The high levels of attentive and care surely is the best and is administered in the most testing of times.
In the early days I had several clinical interventions daily, where COVID guidelines were strictly adhered to throughout. In these dark days, to date I am one of 10 patients at Mayflower who unexpectedly has been given this exceptional life enhancing opportunity.”

The Walton Centre NHS Foundation Trust
The Walton Centre PMP Team
The pain management team at The Walton Centre have been working hard to find alternative ways of continuing to provide effective pain management support and treatment for people with long-term pain in a safe and clinically-effective way since the start of the pandemic.
The team provides clinical input and support for people with chronic pain who have complex needs where many of our patients have significant restrictions and challenges within their daily life. It has been a considerable challenge to continue providing a high-standard of healthcare for our patients whilst also keeping patients and staff safe under the government guidance.
Pain management programmes are group-based rehabilitation programmes that aim to help reduce pain-related disability and distress and improve the quality of life of those suffering with long-term pain conditions. The group aspect of the programme has always been a key component of the multidisciplinary rehabilitation treatment, supporting patients to rebuild their confidence, self-esteem, psychological wellbeing and physical ability.
Since the onset of the COVID pandemic, the pain management programme team has since incorporated video conferencing and virtual appointment technology. This enabled the team to quickly and efficiently provide one-to-one care through video appointments whilst also planning a detailed interactive online group pain management course. The pain management course follows the core principles of the face-to-face group programmes, focusing on physiotherapy, occupational therapy and psychological strategies to help reduce pain related disability and distress.
The format and structure of the programme has been re-designed to make it manageable as a computer-based online course, for use during the COVID pandemic. Sessions are fully interactive with clinicians leading small group discussions alongside active workshops or exercise classes. One-to-one support is also available throughout the course. The course runs half a day, three times a week for six weeks and supports patients in learning effective self-management skills for their chronic pain condition minimising the physical and psychological impact of their long-term pain condition.
In addition to the general pain management programme, the pain management service has been providing specialist programmes for young adults, women with pelvic pain and people with facial pain conditions for several years. We are already planning further adaptations in order for us to provide these specialist courses in the very near future.
The team and the trust are exceptionally proud of the quality of the course and are pleased to be able to continue providing high-quality healthcare support and rehabilitation during the pandemic and associated restrictions to hospital-based care.
Press statements
Restoring services: Trusts are innovating to increase activity
Trusts and their staff continue to work hard to restore activity levels in all services within a challenging context of seasonal pressures, local surges in COVID-19 and a pressing need to address a care backlog in some services, particularly elective care.
We know it is distressing and frustrating for those patients who are waiting longer for care while trusts seek to prioritise their services based on clinical need and reduce waiting lists for some treatments.
However, trusts tell us that many of their services are now operating at, or over, the capacity levels they would expect for the time of year, particularly in community and many mental health services.
In these challenging conditions, we must continue to recognise the extraordinary commitment by NHS frontline staff in restoring services. NHS Providers is shining a light on what trusts are accomplishing in a series of briefings over the coming months. The second edition of our series, Restoring services: NHS activity tracker, focuses on innovations as staff go above and beyond to find new ways of working across acute, ambulance, mental health and community services. Examples include:
- developing an innovative system to ensure the distribution of PPE across 40 mental health and community sites and a 150 mile radius in Northamptonshire
- using technology to ensure safe and convenient appointments continued for patients in Northumbria
- using technology to maximise capacity, enabling both patients and staff to operate triage, diagnostics and share results remotely; and restoring elective care in partnership with the independent sector in Nottingham
- ensuring critical pain management services continued in the Walton Centre
- prioritising cancer pathways and restoring elective care at Sherwood Forest
- reopening transplant services and undertaking 20 liver transplants in Plymouth.
These case studies show that the NHS is not providing a COVID-only service, and is not dragging its feet in restoring service volumes to their pre-COVID levels. Since April NHS trusts have been focusing on increasing the number of operations, procedures and diagnostic testing. Each month the NHS has significantly increased the number of operations and diagnostic tests carried out, as well as restoring outpatient appointments wherever possible.
NHS Providers director of policy and strategy, Miriam Deakin said:
"Trusts tell us they are restoring services as quickly as possible, and that many services are already operating at, or above, usual capacity levels. We know there is a particular challenge to address the elective care backlog, and trusts are addressing that as quickly as they can.
"Ordinarily in winter we see reduced elective activity so that trusts can focus on an increase in demand for urgent and emergency care often generated by seasonal pressures such as respiratory illnesses. However this year staff are under even more strain as they focus on managing a second wave of COVID, planning for a potential ‘no deal’ Brexit and reducing the elective waiting list, all alongside the annual spike in seasonal pressures.
"We owe it to NHS staff to recognise their achievements and just how hard they are working. As our new briefing shows, frontline staff are being just as innovative as they were in the first COVID-19 peak earlier this year.
"The NHS is open for business and it is essential that people seek help and care when they need it."
Most difficult days may still be to come as we head towards winter
Responding to the latest monthly combined performance data from NHS England and Improvement, the deputy chief executive of NHS Providers, Saffron Cordery said:
"Today’s figures reflect the pressures trusts are under to restore activity levels across all services and show a mixed picture of what has been happening on the ground in NHS trusts. We need to delve deeper to understand why there is variation locally in activity levels and why there has been a drop in footfall in A&E.
"It’s vital that despite the surge in COVID-19 cases we are now seeing in some regions, people need to know the NHS is absolutely open, and there for them if and when they need it.
"It’s deeply disturbing to see so many people are having to wait more than a year for routine treatment. Trust leaders are only too well aware how distressing these delays can be, as they work to prioritise services based on clinical need.
"The fact that the NHS is doing 80% of planned operations which required an overnight stay compared to last year is a really significant achievement considering constraints such as enhanced infection control measures, wearing and changing cumbersome PPE, and the lack of routine testing meaning increased staff absences. Trusts have met this key milestone set out for them in the NHS England and NHS Improvement recovery trajectory.
"It is clear that the cancer activity figures remain a concern, although we note that in August over 20,000 people started cancer treatment in the last month.
"We must recognise just how hard NHS staff are working to restore pre-COVID levels of activity, and the innovative approaches they are adopting. There are more operations taking place and the NHS delivered over 1.5 million diagnostic tests in August.
"We have been hearing from mental health trust leaders for some time about the surge in demand for services, as seen in today’s data. The numbers of patients calling the crisis lines has risen, and there are more referrals into mental health services and more individual contacts than ever before. Community and ambulance services continue to run and many colleagues report levels of activity, not captured in these figures, at and above capacity rates at the same point last year.
"But trust leaders tell us they are extremely concerned as demand pressures across systems are beginning to rise as we approach mid-October. The NHS faces turbulent times as it heads towards winter – seasonal pressures, the impact of a potential ‘no deal’ Brexit, a second surge of COVID-19 and a huge backlog in care. No one is in any doubt about the scale of the challenges in the coming months. The most difficult days may still be to come."