NHS Activity Tracker
Introduction
Over the last two weeks the level of community infections from COVID-19 have fallen. However, hospital activity remains significant with over 5,000 patients currently in hospital with COVID-19, and 764 on mechanical ventilators.
Any level of COVID-19 hospital activity has an impact on services, but we also know that trusts are doing all they can to see, treat and prioritise as many patients as possible in a challenging environment.
This month’s figures reflect the stellar efforts to increase activity to often exceed pre-pandemic levels. However, they also show that no matter how fast the NHS runs, the scale of the demand challenge means it may feel like it isn’t gaining ground.
This month's performance figures
Each month NHS England and NHS Improvement publish statistics looking at activity and performance across a range of services including urgent and emergency care, routine care, cancer, and mental health. Below we set out the latest trend for each clinical area:
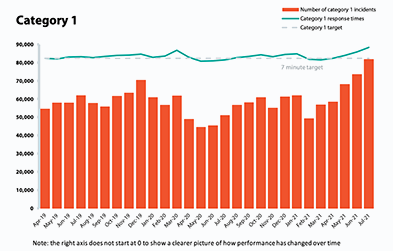
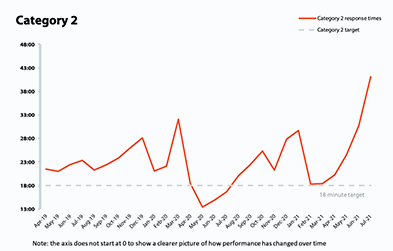
NHS 111 and ambulance: Demand and pressure continues to rise across the urgent and emergency care pathway meaning the ambulance service is facing challenges it usually experiences during the peak of winter. For patients, this means waiting longer for ambulances as waiting times rise significantly.
- Ambulance category 1 incidents, those requiring immediate intervention and resuscitation, increased by 11.1% since last month to 81,685 (8,180 more incidents). Compared to two years ago before the pandemic, they have increased by 32% showing the additional demand pressures.
- For the second consecutive month, the ambulance service has missed the average mean response time target of seven minutes for category 1 calls, with a national average response time of 8 minutes and 33 seconds. The average response time for category 2 calls also deteriorated further, missing the 18-minute target with an average time of 41 minutes. This is the highest average response time since the new targets were introduced.
A&E and emergency care: The pressure on the ambulance service translates to more activity across emergency departments again this month. Although trusts are now seeing numbers akin to two years ago before the pandemic, they report that presentations are far more complex. As a result, waiting times have stretched, resembling those usually experienced in winter.
- In July 2021, there were 2.16 million A&E attendances – just shy of levels in July 2019.
- There were 532,677 emergency admissions in July 2021, a small decrease of 0.5% since the previous month and slightly lower than two years ago. However, admissions are 12.7% greater than July 2020.
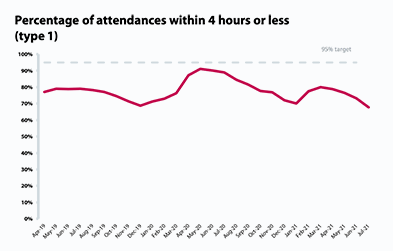
- Performance against the four-hour waiting time target continues to deteriorate as it drops to 77.7%, missing the 95% standard. Performance in type 1 A&E departments slips to 67.7% – the lowest recorded level against the 95% standard since records begun.
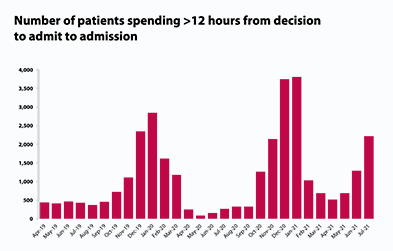
The number of patients waiting longer than 4 hours and 12 hours in A&E after a decision to admit increased significantly this month. Those waiting more than 4 hours increased by 34.7% compared to last month, and those waiting more than 12 hours increased by 71.8% reaching 2,215.
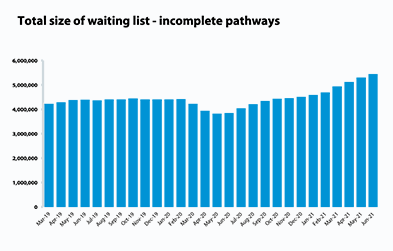
Elective care: For another month planned care activity increased. However, referrals still outstrip supply resulting in a small expansion of the waiting list to 5.45 million. Trusts continue to reduce the number of long waits, with patients waiting 52 weeks or more decreasing for the third consecutive month.
- The size of the waiting list is 41.3% greater than a year ago during the first wave of the pandemic and 24.1% greater than two years ago before the pandemic.
- In June 2021, the number of patients waiting more than 18 weeks decreased again this month, falling by 1.4% meaning 24,783 fewer people are now waiting over 18 weeks than in the previous month.
- As a result performance against the 18 weeks standard improved slightly, increasing from 67.4% in May to 68.8% in June – an increase of 1.4 percentage points.
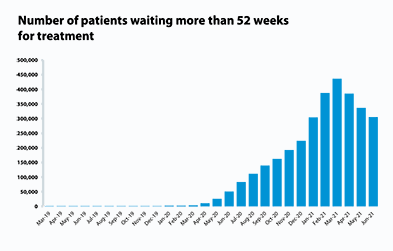
- The number of people waiting over 52 weeks has decreased for the third month running with the number of long waits falling by 31,930 to 304,803. This is a decrease of 9.5% compared to the previous months but an increase of 503% compared to a year ago.
- The number of admitted inpatient pathways increased by 13.7% compared to the previous month with an additional 33,207 admitted pathways than in May, now reaching a total of 275,271.
- Non admitted pathways also increased from May. In June 2021, the NHS delivered 1,06 million elective non-admitted pathways – an increase of 11.2% on the previous month.
- There were 1.67 million new RTT pathways in May, an increase from the previous month. This results in the overall size of the waiting list growing because new referrals outstrip activity.
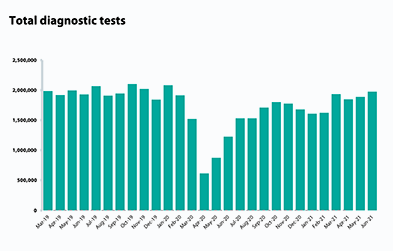
Diagnostics: Diagnostic activity has had a significant boost this month with activity levels exceeding pre-pandemic levels for the first time since before March 2020.
- The number of tests carried out in June 2021 has increased by 4.5% to 1.97 million (84,314 more). This is also 2.3% more than June 2019 showing activity is exceeding pre-pandemic levels.
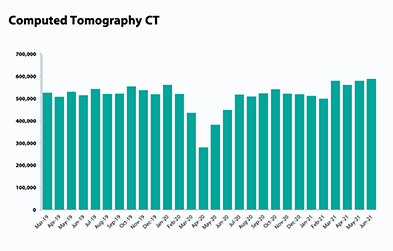
- The number of MRI, CT and colonoscopy tests have all increased this month (+3.1%, +1.5%, +1.1%). Compared to June 2019, the number of MRI, CT and colonoscopy tests carried out has increased (+0.7%, +14.3%, +11.4%).
- The diagnostic waiting list in June 2021 has increased by 4.9% to 1.38 million (64,757 more) on last month. This is up by 80.1% on last year (613,817 more) and down by 3.0% on June 2019 (43,060 fewer).
- 22.4% of people were waiting six weeks or more for a test in June 2021, missing the 1% target again this month.
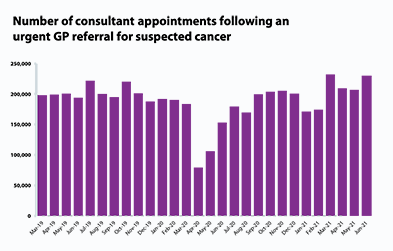
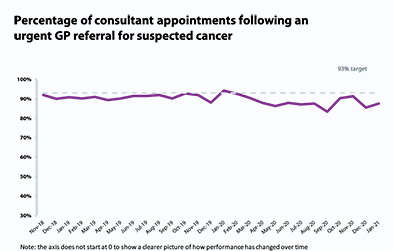
Cancer: There was also a significant pick up in cancer activity in June 2021 after a few months where activity had fallen. Numbers are once again exceeding pre-pandemic levels showing how hard trusts are working to treat those presenting with cancer. However, demand is high and therefore performance against the key cancer waiting time standards has deteriorated.
- A total of 230,110 people were seen on the two weeks of an urgent referral for a suspected cancer pathway– an increase of 11.1% compared to the previous month equating to an additional 22,922 more consultations. This level of activity is 18.6% more than two years ago before the pandemic. 84.9% of those urgent GP referrals were seen within two weeks, missing the 93% standard.
- The number of people on the 31-day pathway, which aims for one month between starting treatment following a decision to treat, also improved this month to 27,293. This is an increase of 10% since the previous month and 8.8% greater than before the pandemic in June 2019. 94.6% of people started treatment within one month of the decision to treat, missing the 96% standard.
The number of people waiting 62 days from urgent GP referral to starting treatment also increased to 14,218. This is an increase of 9.4% compared to the previous month and an increase of 6.7% from June 2019. 73.3% of the people who started treatment did so within 62 days of their urgent GP referral, missing the 85% standard.
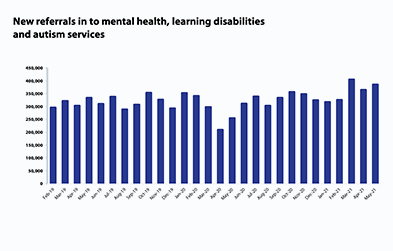
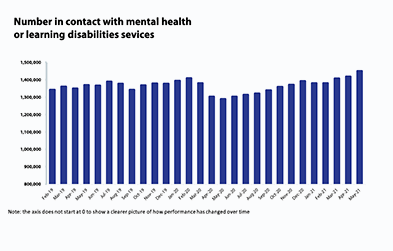
Mental health: A month on month trend, we are seeing the highest ever number of people in contact with mental health services since records began each month. New referrals are also considerably higher than before the pandemic, with demand showing no signs of easing.
- In May 2021, mental health referrals increased by 5.7% to 385,430 (20,739 more referrals). Compared to a year ago, during the first wave of the pandemic, referrals have increased significantly by 51.6% (131,243 more referrals). Compared to May 2019 referrals have increased by 15.3% (51,271 more referrals) showing the significant demand pressures currently being experienced by mental health trusts.
- The number of people in contact with mental health services has increased by 2.2% to 1.45 million (31,865 more people in contact) on last month. This is the highest number of people in contact since records began. Compared to a year ago, there are 12.4% more people in contact with mental health services (160,277 more people).
- In May 2021, 2.04 million care contacts attended (up slightly by 0.1% and 1,720 than the previous month). However, in comparison to a year ago, there are now 11.2% more care contacts attended (204,783 more care contacts).
In May 2021, the number of out of area placements (OAPs) increased to 745 (45 more OAPs than last month). Compared to a year ago, OAPs have increased by 49.0% (245 more OAPs).
Our view
The activity and performance data published today paints a clear and coherent picture across the bulk of services. The NHS is doing all it can to increase activity and is now taking more people to hospital by ambulance, carrying out more diagnostic tests, seeing more people with a suspected cancer, treating more people with cancer, receiving more mental health referrals and providing more mental health contacts than it was this time two years ago. Elective activity has also returned to 100% of pre-pandemic levels.
All of this work to exceed previous activity levels needs to be applauded given the context in which the NHS is delivering these gains.
NHS running very fast to stand still
As frontline staff work tirelessly to reduce the backlog of care across all physical and mental health services, it is clear from the figures published today that demand for services is outstripping these efforts.
Despite the increase in activity across the board there are a range of factors which are making current conditions for trusts very challenging. In fact, some trust CEOs are telling us that their organisation is facing the toughest pressures they have ever known.
Firstly, trust leaders have been reporting the extreme pressures across the urgent and emergency care pathway. Winter-like pressures put additional strain on bed capacity, reducing the availability for elective care treatment and therefore capping how fast trusts can go to reduce waiting times.
Secondly, leaders from all trust types are telling us that the complexity of presentations has increased significantly. Seeing more acutely unwell patients, or people with more complex health needs takes more time and reduces capacity.
Thirdly, there are still 5,000 COVID-19 patients in hospitals across the country. Although the numbers do not resemble those seen in the January wave, the impact on planning, capacity and staffing is still felt and has reduced overall capacity. Not least because of the continued need for infection control measures. This means that trusts have less available space and must take more time to clean equipment which again reduces the speed at which they can go.
Lastly, staffing remains an ongoing challenge with higher than usual absences, in part due to sickness absence resulting from COVID-19. We are also hearing from some trust leaders that they are extremely concerned about the wellbeing of their staff with an increased level of sickness being recorded due to stress and burnout. Throughout July and August, trusts have also seen staff take their much needed summer leave which also has a knock on effect as to how fast trusts can go.
Therefore, considering these constraining factors, it is impressive how much activity the NHS is currently delivering for patients. However, trust leaders are only too aware that the progress is too slow, and that the pandemic has left an overwhelming backlog of care. For some patients, waiting times are growing and fall short of the standards leaders and frontline staff strive so hard to deliver.
Trust leaders are doing all they can prioritising those patients who need to be seen most urgently across all physical and mental health services. But they need to be resourced properly so they can meet the myriad challenges ahead.
As trust leaders put in place plans to tackle the backlogs over the second half of the financial year and beyond, it is so important the NHS gets the immediate funding it needs for H2 and in the upcoming comprehensive spending review.
A&E
Cancer
RTT
Diagnostic tests
Ambulance indicators
Mental health
CASE STUDY
Berkshire Healthcare NHS Foundation Trust
Dr Alice Farrington, Principal Clinical Psychologist
and Mairi Evans, CYPF & BEDS Clinical Director
Like many NHS services, Berkshire Healthcare had to transform overnight to utilise digital technology to maintain accessible, safe and effective care during the COVID-19 pandemic. Now that restrictions are being lifted, many services are considering which innovations to maintain or develop further.
Berkshire Healthcare’s Child and Adolescent Mental Health Services (CAMHS) made rapid service wide digital transformations, where clinically safe to do so assessments and treatment appointments were conducted online. This required us to master software to share genograms (family trees), diagrammatic formulations, and to continue to engage children in online therapeutic work. We quickly learned to problem solve and learned that we could still build effective relationships and deliver compassionate care digitally.
In addition to individual and family therapies, we used our new digital expertise to deliver online workshops for parents, where we were able to encourage active participation through using the chat function for questions and comments. These workshops were well received by parents, who rated them very highly, and found them easier to attend. Without the constraints of room size or parking capacity, we were able to invite more parents at a time to online workshops. In response to emerging needs and the impact of the pandemic we also developed new workshops including a workshop on ‘back to school anxiety’. Each workshop was recorded to make it accessible on demand.
Staff training events were also provided online and were well attended. Topics covered included clinical presentations such as ARFID (avoidant restrictive food intake disorder), autism, anxiety, and training about the types of adaptations needed to offer safe, effective and evidence-based assessment, treatment and supervision online.
Our Autism Assessment Team (AAT) changed the delivery of assessments due to concerns that the usual way of diagnosing via Autism Diagnostic Observation Schedule 2nd Edition (ADOS-2), would not be reliable with face masks and social distancing. As part of the comprehensive multi-disciplinary assessment, the AAT has now been using a combination of an adapted online assessment and/or inviting families in using the Brief Observation of Symptoms of Autism (BOSA) assessment, adapted from the ADOS-2 and the Brief Observation of Social Communication Change (BOSCC). These have allowed the team to offer an appropriate assessment option for a wide range of children according to age and language/learning levels and at every assessment stage during a challenging time. This has been appreciated by families who are keen to avoid additional waiting times for assessment.
In addition to individual and family therapies, we used our new digital expertise to deliver online workshops for parents, where we were able to encourage active participation through using the chat function for questions and comments.
The Autism Assessment Team (AAT) had already developed a video to give children and young people information about what an assessment will be like. With the help of service users, other CAMHS teams are now also developing short video clips for young people about emotional difficulties, ideas of what might help them, and what to expect at an assessment appointment.
Prior to the pandemic we were already providing support via SHaRON (Support Hope and Recovery/ Resources Online Network), this network has continued as a useful means to access safe and accessible support online. SHaRON offers confidential online space for self-help, peer support and access to resources and is moderated by a team of clinicians and volunteers. SHaRON includes support networks for: parents of children who have anxiety, depression, OCD, autism, are experiencing a first episode of psychosis; parents of children waiting for an autism assessment; people with eating disorders and new mums with mental health difficulties and their partners. SHARON also provides an online network for professionals working with children across Berkshire. SHaRON has been a wonderful resource to connect service users or parents/carer to each other as well as to the services supporting them. It increases access to evidence-based resources, empowering people to support themselves. It can give rapid access to peer support as well as specialist advice from a range of clinicians which families find very supportive. It is also a very efficient way for clinicians to provide information and support to many families at once. SHaRON also provides a wonderful opportunity for service users and families to share hope, successes and solutions that have worked for them. SHaRON has been of particular benefit during the pandemic with an increased use of online forums and has supported families during lockdown and with the anxiety about restrictions easing. Many users reported that they found this service ‘a lifeline’ during the pandemic.
We are now in the position to decide which of the digital transformations we would like to continue to offer. We are planning a ‘blended’ service going forward taking into account service user preference, where 38% of service users preferred face-to-face appointments, 34% preferred online appointments, 20% preferred a choice between online and face to face appointments. The main advantages of online appointments reported by families was saving travel time, more convenient and they did not need to worry about the risk of contracting COVID-19. However, 22% stated that they prefer talking face to face.
We feel service user choice and flexibility is very important. For example, young people who feel anxious about face-to-face appointments can be offered an online meeting first to build trust and facilitate engagement. Therapist assisted exposure at home can now take place online as well as via home visits, saving clinician time. However, we will always continue to offer face-to-face appointments for young people who prefer this, as well as when clinical presentation and/or risk indicates that a face-to-face appointment would be preferable.
There is plenty to do to meet the growing needs of children and young people and this is a complex task. But the pandemic propelled us to innovate and learn valuable lessons to improve service delivery and offer more flexible access.
Press Statement
NHS running very fast to stand still, as size of overall backlog increases
Responding to the latest monthly combined performance data from NHS England and NHS Improvement, the chief executive of NHS Providers, Chris Hopson said:
“Today’s figures confirm the scale of challenge facing the NHS. Trusts continue to rapidly increase levels of activity but the overall care backlog is still growing as patients for whom treatment was delayed during the COVID-19 now rightly come forward for care.
“Today’s figures show how hard NHS staff are working and how well trusts are performing. 84,000 more diagnostic tests took place in June than the previous month – the highest number over the last year.
“Trusts have, once again, reduced the number of people waiting for planned care for more than 52 weeks, this time by 32,000.
“They’ve also increased the number of people who have been checked for cancer in June to 230,000, the second highest figure on record.
“These are huge achievements, particularly given the other pressures the NHS has been facing – the large numbers of staff self-isolating and, in July, starting to take summer leave; huge pressures on the emergency care pathway; 5,000 COVID-19 patients in hospitals for a good part of July; and the ongoing vital COVID-19 vaccination campaign.
“They show that, when the NHS is fully supported, it delivers in spades.
“But there are significant concerns as well.
“Pressures across urgent and emergency care are very high. Despite the best efforts of frontline staff, 2,215 patients waited over 12 hours to be seen in July. The demands on ambulance services are particularly concerning with the most serious 999 calls requiring an ambulance reaching 82,000 in July – a 32% increase compared to two years ago, before the pandemic. Many trust leaders are saying that they are now experiencing levels of urgent care pressure traditionally seen in the depths of winter.
“Trust leaders are doing all they can to get through care backlogs as quickly as they can, prioritising those patients who need to be seen most urgently. But they need to be resourced properly so they can meet the myriad challenges ahead.
“That’s why it’s so important the NHS gets the immediate funding it needs for the second half of the financial year and in the upcoming comprehensive spending review”.