
Week nine of the winter sitreps published today by NHS England and NHS Improvement continues to show how difficult this period is for trusts. While there have been welcome reductions in a number of the COVID-19 metrics nationally, the pressure on trusts remains extreme as large numbers of the sickest patients still require treatment in critical care. Huge efforts are being made by trusts throughout the system, with impressive reductions seen in ambulance handover delays this week, but the impact on the NHS workforce is increasingly in focus as we start to look ahead to the spring.
This week’s key headlines (covering 24 – 31 January):
- the number of COVID-19 patients in hospital continues to fall (as of yesterday this figure stands at 26,374), but this remains 39% higher than the peak of the first wave in April 2020. Regionally, the South East is seeing the fastest reduction (20% fewer in hospital than last week). The number in mechanical ventilation beds is falling at a slower rate, as the downstream effect of the large rise in cases in the first weeks of 2021 continues to be felt
- the number of adult critical care beds open continues to increase, although there has only been a small rise from last week. An average of 6,153 of these beds were open, 96 more than last week (+1.6%). The current figure is 39% higher than the start of the winter, with an additional 1,738 more beds open, and there are now 2,492 more than the same time last year, an increase of 68%
- national general and acute bed occupancy is down slightly this week (86.9%, down from 87.6%), while the total number of beds open is very similar to last week
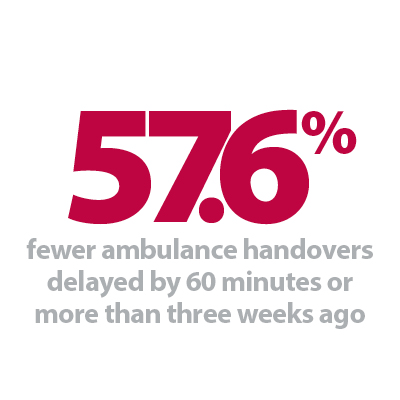
- the number of ambulance arrivals were very similar to last week and remain lower than last year (-8.2%). Handover delays continue to lessen, now well below the high levels seen in early January. 2.6% of arrivals were delayed by 60 minutes or more, down from 3.7% last week and much lower than the 6.4% in week 6
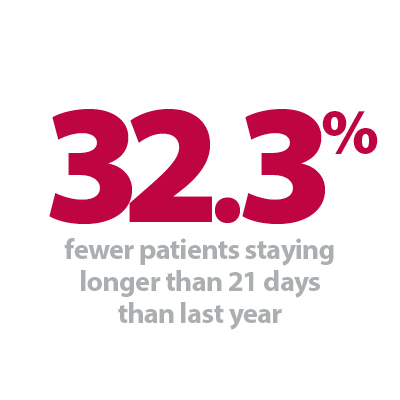
- the number of long stay patients remains well below the level expected at this time of year, with the proportion of COVID-19 patients a contributing factor, while beds closed due to diarrhoea and vomiting, norovirus and the prevalence of flu are all having far less impact than in previous years.
While the number of COVID-19 cases and patients being admitted to hospital are now falling nationally at some speed, we are understandably seeing slower rates of reduction in the total number still requiring hospital treatment, as well as the number of the sickest patients requiring mechanical ventilation. Trusts will be acutely aware of how precarious the current situation is, and will want politicians to factor in the evidence from across these different peaks when considering easing lockdown restrictions.
This week we saw an average of 6,153 adult critical care beds open each day, a new record high and 96 more than last week (1.6% higher). 5,302 of these were occupied, also slightly more than last week (24 more, 0.5% higher). Because the number open increased by more than the increase in the number occupied, the occupancy rate fell slightly (86.2%, down from 87.1% last week), but this is a reflection of the efforts of trusts to open more beds and create adequate surge capacity, rather than a reduction in the number of patients requiring this level of care.
Looking at the regional breakdown, London, the East of England and South East have rapidly increased the number of adult critical care beds open since the start of December (by 64.2%, 62.6% and 52.3% respectively). The North West and North East and Yorkshire have also seen increases over this period (by 17.5% and 13.7%). While not as dramatic as in some other regions, this is largely a result of trusts in these areas already having opened additional capacity to accommodate the increase in demand they experienced in November.
Ambulance services have faced a unique set of circumstances this winter, and their ability to transport large numbers of critically ill patients to hospital has never been more important. At the start of January, the proportion of patients delayed at the point of handover was at a record high, as several parts of the system were stretched near breaking point. Thankfully, far more handovers are taking place swiftly now, with the latest figures showing 2.6% are delayed by 60 minutes or more, the smallest proportion since the start of the winter.
Trusts know that the challenges they are currently grappling with will not be relieved overnight. It is very positive that COVID-19 cases are falling, but the descent from the latest peak in demand for NHS services will naturally take place more slowly. All types of trust, including those delivering community and mental health services, will be dealing with the impacts of COVID-19 for the foreseeable future, and the recovery of staff will be essential for the continued provision of high-quality services.
This week's contribution comes from Dr Esther Cohen-Tovee who is the director of AHPs and psychological services at Cumbria, Northumberland, Tyne and Wear NHS Foundation Trust. She describes the COVID emotional wellbeing team (CEWT) set up during the first lockdown, and how it continues to be a vital resource for staff as the importance of wellbeing is increasingly in the spotlight.
COVID emotional wellbeing team
During the first lockdown, Cumbria, Northumberland, Tyne and Wear NHS Foundation Trust (CNTW) set up a COVID emotional wellbeing team, otherwise known as CEWT.
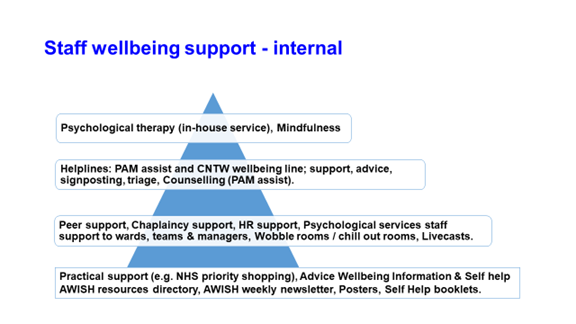
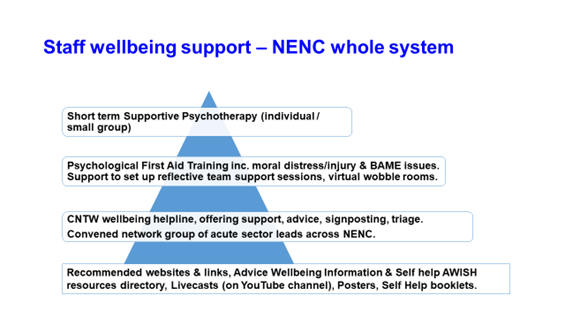
This enabled us to coordinate a wide range of wellbeing initiatives, based on issues that were emerging both internally within the organisation and nationally as we all got used to a new way of life. An external network of representatives from acute trust partners and the North East Ambulance Service (NEAS) was also created to explore staff wellbeing needs and what CNTW could offer, as a leading provider of mental health and disability services.
The work resulted in a number of wellbeing initiatives and offers, both internal and external. The external offer was extended to the whole health and care system in the North East and North Cumbria (NENC), and was later extended to include education, police, fire and prison services. This work received regional and national interest, including presenting it as part of webinars and hosting a virtual ministerial visit.
AWISH (advice, wellbeing, information and self-help) newsletter
The AWISH newsletter is sent to our staff every fortnight. It is sent via email and teams are encouraged to print copies for those who do not regularly access a computer. There have now been 25 editions, detailing where staff can go to for help as well as NHS offers and discounts, and staff news. It also includes a searchable resource directory which helps staff access links to wellbeing support.
Psychological wellness training
We have offered an adapted form of psychological first aid training, which includes issues specific to the pandemic such as moral distress and Black, Asian and minority ethnic staff issues. This training has been taken up by nearly 250 people so far, both inside and outside of the organisation.
Livecasts, wobble rooms and team time
CNTW organised and delivered 10 livecasts to staff on a range of topics, from sleep to burnout and BAME conversations. The livecasts are available to watch on the trust YouTube channel.
The trust's Schwartz Round team launched 'wobble rooms' to support staff wellbeing, offering them a way to articulate how they feel about the pressures they are dealing with. Staff discussed a range of topics including how to adjust to changes in our lives, anxiety and how to protect our families during times of crisis. These sessions took place virtually, some services also set up physical 'wobble rooms' where staff could take a break during their shift. Feedback has been extremely positive, with staff saying they felt well-supported as a result.
The Schwartz Round team have also provided a modified form of Schwarz Round called 'team time' to teams or groups of staff and they also support external organisations set up reflective team sessions.
Psychological helpline and staff support
A helpline for both CNTW and external staff was set up to provide additional support. People have been able to talk through many issues such as mental health, bereavement, family and work-related stress, guilt and returning to work. Call volumes have been steadily increasing, and the support and impact for individuals appears to be significant. The helpline has recently been integrated with the North East and North Cumbria staff wellbeing resilience hub.
Next steps
It is clear that staff wellbeing needs are increasing as the pandemic continues. Many staff are suffering fatigue, morale is low and they are at risk of burnout.
CNTW HR and workforce have put forward the health and wellbeing star as our health and wellbeing strategy, which is aligned to the NHS England and NHS Improvement People promise. This will ensure a holistic integration of emotional, psychological, physical and social wellbeing approaches, together with the dimensions of financial and career wellbeing.
NHS under sustained pressure as pandemic continues to take its toll – talk of relaxing restrictions premature
Responding to the latest winter figures, the chief executive of NHS Providers, Chris Hopson said:
"The latest COVID and winter figures show that while the NHS may have passed the peak of COVID-19 infections and hospital admissions, we are still in dangerous territory.
"To continue the mountaineering analogy, whilst we may have crested the peak, we remain at a dangerously high altitude, have only just started the descent and know that this descent is going to take months, not days or weeks.
"Although the number of patients in hospital with COVID-19 is falling from the peak last month, there are still 26,000 covid positive inpatients, 40% higher than the peak of the first wave in April 2020.
"The NHS currently has nearly 70% more critical care beds than it did last winter, with some trusts still having to open more ICU beds last week to accommodate the sickest COVID-19 patients.
"These extraordinary pressures will continue for a long time yet. And with another cold snap on the way, we must not forget that the NHS is also having to deal with the usual winter pressures that come with a drop in temperatures and bad weather conditions.
"Much of the media coverage focuses on hospitals. But all types of trust - community, mental health and ambulance trusts - are incredibly busy. They are working together across their local health and care systems to respond to the pressures by providing mutual aid and flexing capacity so patients are in the most appropriate setting.
"Passing the peak must not, and should not, be a trigger in itself for the relaxation of restrictions, as some siren voices are prematurely suggesting. The key questions are how rapidly we can come down the mountain and how far down we need to get before we can consider safely relaxing the restrictions. We saw last year how dangerous it is to relax restrictions prematurely.
"So staying at home and following the rules remains as important as ever. Rushing headlong into lifting the restrictions risks undermining all of the hard work and sacrifices we have made so far."