
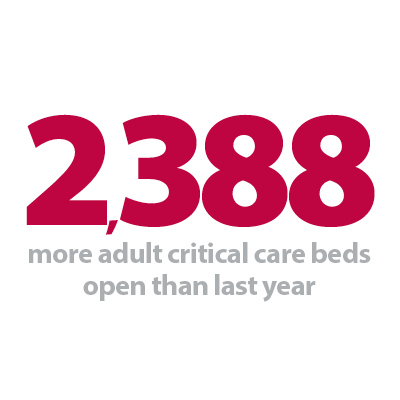
Today's winter sitreps data, published by NHS England and NHS Improvement, once again highlights the intense pressure the NHS is continuing to face. It was also this week that the UK tragically recorded over 100,000 registered COVID-19 deaths. This is a dreadful milestone to have reached and will be front and centre in the minds of all NHS staff as they go to work each day. Today’s data shows activity right across the country remains extremely high with large numbers of COVID-19 patients still requiring treatment. We are, however, starting to see the numbers in hospital starting to fall. This is a positive step in the right direction, but we know from previous trends it might be several weeks until we begin to see this translate into lower mortality figures. One notable theme from week 8 is the continued expansion of adult critical care capacity. This week, there were an average of 6,057 beds open, 380 more than last week. The current figure is 1,642 more than the start of the winter and 65% greater than the same time last year – equating to 2,388 more intensive care beds. Trusts are working incredibly hard to continually expand the capacity of intensive care units, with more critical care beds made available this week. This reflects how trusts are continuing to flex their resources to treat the sickest patients requiring ventilation, with these beds occupied at record levels – 87.1% nationally.
Other key headlines from this week’s data include:
• the number of COVID-19 patients in hospital is falling. There are currently 30,846 positive patients in acute hospitals across the country, but this is 3,000 fewer than a week ago (9% lower). Regionally, numbers are falling fastest in London and the South East
• nationally, bed occupancy of general and acute beds has increased slightly to 87.6%, up from 87.2%) last week. The total number of open general and acute beds is very similar to last week, again showing that the pressures are on the emergency and critical care pathway
• more patients arrived at hospital via ambulance this week but numbers still remain 5.2% lower than the same week last year
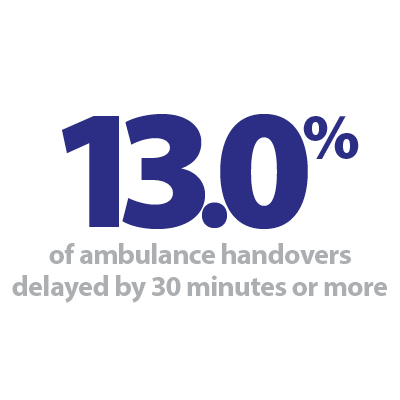
• ambulance handover delays are similar to last week – but remain lower than the numbers we were seeing a few weeks ago: o 13% of handovers were delayed by 30 minutes or more, up from 12.6% last week but much lower than the 17.2% in week 6. o 3.7% were delayed by 60+ mins, down from 3.9% last week and also much lower than the 6.4% in week 6
• fortunately, the number of patients staying in hospital more than 14 and 21 days remains much lower than last year
• similarly, the NHS isn’t having to close a significant number of beds due to diarrhoea and vomiting (D&V) or norovirus as it has in previous years. In week 8 there were an average of 17 beds closed per day - at the same time last year there were an average of 773.
Currently, COVID-19 patients account for 41% of all patients in hospital in England and although the numbers of new admissions and the total numbers of COVID-19 patients is falling, we can expect this intense pressure on the NHS to last for at least a further few weeks.
The direct impact of COVID-19 on NHS activity, right across community services, hospitals and the ambulance sector will only begin to ease over the next weeks if the public comply fully with the national lockdown rules. It is also imperative that NHS data and advice from trust leaders are central to any decision to ease the current lockdown restrictions over the coming weeks.
In the long term, once there is a significant reduction in the community and hospital prevalence of COVID-19, there are significant backlogs of care that will remain and trust leaders are already working with central bodies to plan for how these will be addressed.
We also know from NHS data that demand for mental health services has never been higher. It is clear that the NHS will need to be at the forefront of tackling the long term impact of COVID-19 on the mental health and wellbeing of the public and NHS staff.
Looking beyond the next few weeks of intense pressure, NHS staff will need respite and to be able to take their annual leave – much of which they have had to delay to continue treating patients in these extraordinary circumstances. They are the driving force behind the NHS and are working in such difficult circumstances every single shift. Their needs will need to be balanced against any recovery trajectory.
Lastly, the vaccine offers hope for the future. In week 8 the NHS has continued the successful roll out of the largest vaccination programme in its history. Across the UK 7.1 million first vaccine doses have been administered, 6.22 million in England. Although a lumpy supply chain is currently the main constraining factor, on the 23 January, the NHS vaccinated nearly half a million people in one day. In recent days we have seen news that many more vaccine centres are being opened, suggesting that once steady vaccine supply is in place, the NHS will have the capacity it needs to pick up the pace even further.
This week's Winter watch contribution comes from Heidi Smoult and Debbie Ivanova who are deputy chief inspectors at the CQC. They explain why some inspections are being carried out during such a busy time in the NHS, how inspections can help trusts manage risk from infection, improve service flow and how system working is helping to relieve bed occupancy pressure on the NHS.
Winter Watch: Immense Pressure
In our third #NHSWinterWatch episode we talk to Care Quality Commission colleagues, Heidi Smoult, deputy chief inspector for hospitals, and Debbie Ivanova, deputy chief inspector for adult social care, about the concerns surrounding ongoing NHS winter inspections, issues in infection prevention and control, and all about their clinician support tool Patient FIRST, designed by clinicians for clinicians.
Pandemic has had an enormous effect across all NHS services this winter
Responding to the latest winter reporting data from NHS England and NHS Improvement, NHS Providers chief executive Chris Hopson said:
"The data released today once again highlights the intense pressure the NHS is continuing to face. We can expect this to last for at least a further month. Large numbers of COVID-19 patients are still requiring treatment, despite a welcome reduction in the numbers in hospitals, particularly in London and the South East.
"It is extremely impressive to see how trusts are continuing to expand the capacity of intensive care units, with more critical care beds made available this week. This reflects how staff are continuing to flex their capacity to treat the sickest patients requiring ventilation, with these beds occupied at record levels – 87.1% nationally.
"More people were taken to hospital by ambulance this week. Reducing handover delays remains a priority for trusts, with 13% delayed by over 30 minutes, with each of these meaning a crew cannot respond rapidly to another emergency call in the community.
"While the full impact of the pandemic won’t be fully understood for some time, it is clear it has had an enormous effect across all NHS services this winter, despite the best efforts of staff working in ambulance, community, hospital and mental health sectors.
"Looking forwards, NHS staff will need support and respite. They are the driving force behind the NHS, and are currently rolling out the largest vaccination programme in history, while still caring for COVID and emergency non COVID patients amidst annual winter pressures. Their wellbeing continues to be the top priority of trust leaders."