
The latest winter sitreps published today by NHS England and NHS Improvement cover the end of 2020 and the first few days of 2021. The growing pressure brought about by COVID-19 is clear to see. As the number of people infected with the virus skyrocketed in December, this has inevitably led to greater demand for NHS services, and in the data there are several concerning developments taking shape.
Winter sitreps key headlines (28 December – 3 January):
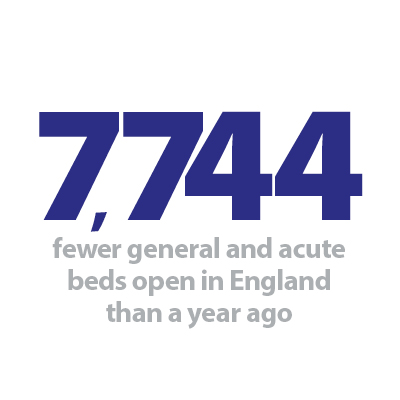
- The national bed occupancy rate is 86.7%, up from 82.9% in the Christmas week. The overall occupancy rate remains lower than the same time last year (94.2%), but this will feel much busier given the current workforce constraints and infection control requirements
- regionally, London has the highest occupancy (90.4%), with the East of England and South East also above the national rate
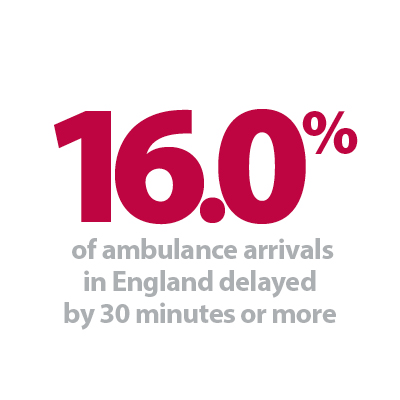
- the number of patients arriving by ambulance increased this week (5.6% more than last week), and while the total number of arrivals remains considerably lower than last year, the proportion with delayed handovers saw a worrying jump this week. 16.0% were delayed by 30 mins or more (up from 10.7%), and 5.8% were delayed by 60 mins or more (up from 3.0%). These are now close to last year’s levels when the total number of arrivals was much higher
- on the positive side, we continue to see far fewer patients staying in hospital longer than 7, 14 or 21 days compared to last year (18.6%, 23.4% and 27.3% lower respectively)
- likewise, the impact of diarrhoea and vomiting and norovirus as well as the effects of seasonal flu continue to be far less than we’d expect at this time of year.
Since the start of December, the number of new COVID-19 cases has risen dramatically. In the seven days to 6 January, there were 360,537 new cases in England, over 300% higher than the same period a month ago. As a result, we are now seeing record numbers of patients being admitted to hospital, with the latest total of 27,727 COVID-19 patients on 6 January occupying approximately a third of the entire general and acute bed base of the NHS. For comparison, the largest number in hospital on a single day during the first peak of the pandemic was 18,974 in April 2020, which means there are now 46% more COVID-19 patients than at the height of the first phase.
London and the South East have been the first regions to feel the effects of the new variant of the virus which is spreading rapidly. Currently, more than nine in ten beds in London trusts are occupied, and with over 7,000 of the capital’s 12,668 beds taken by COVID-19 patients, there really is very little room for manoeuvre. Already we are hearing that some trusts are being forced to scale back non-COVID services, and with cases continuing to rise, it appears to be a matter of time before this becomes more widespread.
Ambulance services are in the spotlight as larger numbers of critically ill patients are requiring emergency care. The total number of ambulance arrivals increased to the highest level of the winter so far, and unfortunately this week the proportion of handovers that were delayed was also higher than anything seen since last winter. Of particular concern, over 5,000 patients were delayed by 60 minutes or more, as certain parts of the system are disproportionately affected by the current crisis.
Efforts to retain patient flow are as crucial as ever in all care settings, and it is positive that there are far fewer long-stay patients than previous years. Trusts will also be glad the impact of norovirus and seasonal flu remains low, but we know cold weather can quickly change this. Staff are working exceptionally hard to maintain services in these unprecedented times, and their incredible dedication to ensure the quality of care for patients must be recognised.
In our member contribution this week we hear from Dr Ayesha Rahim, consultant perinatal psychiatrist and chief clinical information officer for Lancashire and South Cumbria NHS Foundation Trust, who outlines the technology they are using to reduce pressure on secondary healthcare and enable access to mental health services at the first point of care.
Implementation of Advice and guidance in Lancashire and South Cumbria
Dr Ayesha Rahim, consultant perinatal psychiatrist and chief clinical information officer for Lancashire and South Cumbria NHS Foundation Trust tells us about the implementation of a clinical decision support software introduced to mental heath services for the first time. The prevalence of common mental health disorders in the UK population continues to rise year on year, as evidenced by national data. This puts increasing pressure on the finite resources within both primary care, and secondary care mental health services. Community mental health team (CMHT) referrals increased by 19% between 2010 and 2014 (Mental health network, 2016).
In Lancashire and South Cumbria NHS Foundation Trust, the CMHT referral rate in 2019 was shown to be 42% higher than the national average, according to national reporting data (NHS Digital, 2019). Anecdotally, some patients were having to wait up to nine months to see a consultant psychiatrist due to these pressures. Therefore managing this demand effectively and efficiently was important to provide a better experience for patients in terms of waiting times to see a psychiatrist, and also to support GPs in our catchment area who were inevitably having to manage these patients in the interim.
Advice and guidance was implemented as part of the national Global Digital Exemplar programme. The project was focused on addressing the issues around waiting times for patients, and support for GPs in managing more complex mental health presentations.
Two community mental health teams (Single point of access team and the Memory assessment service) implemented the electronic messaging system to allow GPs to contact consultant psychiatrists directly for clinical advice, in lieu of putting in formal referrals to the respective teams. This led to a change in GP management in 66% of cases, shifting the balance from secondary care out-patient clinics, to GP delivered care with specialist advice.
This system is based on the Advice and guidance functionality within the national e-referrals service (eRS) platform. A local acute trust (University Hospitals of Morecambe Bay) had developed their own version, providing enhanced functionality over and above the national eRS version. This has now been adopted by Lancashire and South Cumbria NHS Foundation Trust.
The system is embedded in EMIS for all GP practices, so GPs who want to raise a query click through from their electronic patient record, in patient context. A dialogue box opens which they can then write the clinical query in, and they can also attach a file to the message if required. If GPs would prefer to be contacted by phone they can use the date/time picker to indicate their availability, which is then also sent alongside the query. Specific patient details are automatically pre-populated. The clinical query can be directed to a central email inbox, and the identified recipients (in this case the consultant psychiatrists in the team) take “ownership” of an individual query and respond to the query as appropriate.
There is no limit to the number of messages that can be sent by either party in the conversation, however the query can only be marked as "closed" by the GP. On closure, the system displays a mandatory questionnaire for GPs with four questions and an optional free text box for comments, this enables the GPs to provide information for the patient journey pre and post Advice and guidance, feedback on the ease of use of the system and the free text box allows GPs to make suggestions on how the system could be improved. Once closed, the conversation automatically feeds into the EMIS clinical record.
Data from the two pilot teams
Lancaster and Morecambe – Specialist triage, assessment and referral team (START)
Go live date: 15 October 2019
- How would GPs have managed the case if Advice and guidance hadn’t had been there?
- 12 month post-deployment data
- Percentage of management decisions changed as a result of Advice and guidance [via existing GP survey]
- 12 month post-deployment data = 62%
- Total number of queries
- 12 month post-deployment data = 143 conversations
- Ease of use of system for GPs [via existing GP survey]
- 12 month post-deployment data = 100% easy to use
- Usefulness of advice received by GPs [via existing GP survey]
- 12 month post-deployment data = 60% really useful, 32% useful, 8% not very useful
Lancaster and Morecambe – Older adults
Go live date: 10 August 2020
- How would GPs have managed the case if Advice and guidance hadn’t had been there? [via existing GP survey]
- Four month post-deployment data
- Percentage of management decisions changed as a result of Advice and guidance
- 4 month post-deployment data = 83%
- Total number of queries
- 4/12 post-deployment data = six conversations
- Ease of use of system for GPs [via existing GP survey]
- 4/12 post-deployment data = 100% easy to use
- Usefulness of advice received by GPs [via existing GP survey]
- 4/12 post-deployment data = 75% really useful, 25% useful
Following the deployment of Advice and guidance to the pilot teams, it has been important to look at widening the rollout of the system to other Lancashire and South Cumbria NHS Foundation Trust services, allowing more teams to benefit from the system and assess the impact on patient care.
The programme lead is linking in with the integrated care system project manager and following a road map, detailing the roll out of the Advice and guidance system to GP practices across Lancashire and South Cumbria. Future services are already being identified to benefit from Advice and guidance and the project will continue throughout 2021.
COVID-19 pressures are being felt across the system
Responding to the latest winter reporting data from NHS England and NHS Improvement the chief executive of NHS Providers, Chris Hopson, said:
"Today’s figures reflect the relentless pressure trusts are under as they deal with the demand posed by COVID-19 and winter pressures.
"Record numbers of COVID-19 cases are now being recorded every day.
"While the total number of beds open this week has increased, occupancy is rising at a faster rate, and there are real concerns about ensuring there’s enough capacity – in terms of beds and staff – to safeguard the quality of care for patients.
"Major pressure on hospital and community bed occupancy is having significant knock-on effects throughout the system.
"Ambulance arrivals increased by nearly 6% this week and handover delays for patients arriving by ambulance increased steeply, with 16% of patients delayed by 30 minutes or more and nearly 6% delayed by over an hour.
"Every handover delay equates to a crew that can’t respond quickly to other emergency calls where they are desperately needed.
"Trust leaders are telling us these pressures are being felt across the system, with mental health, community as well as in primary and social care settings similarly feeling the brunt of winter and COVID-19 pressures.
"In a positive development, it is good that bed closures due to norovirus remain significantly lower than usual thanks to social distancing measures.
"Throughout this, we must remember the devastating toll this pandemic is having on the NHS and care workforce. We owe a particular debt of gratitude to our hardworking NHS staff, who continue to work tirelessly in incredibly tough circumstances.
"In the coming weeks the acceleration of the COVID-19 vaccination programme will thankfully mean quick access to the jab for NHS and care workers.
"This will be crucial to reducing staff absence from COVID-19, and enabling sufficient staff to work to offer the best possible care for all patients, COVID and non-COVID."