
The latest winter sitreps published by NHS England and NHS Improvement today cover the second week of January, showing that the pressure on the NHS due to COVID-19 remains incredibly intense.
Thousands of additional critical care beds have been opened, and occupancy of these is rising as more of the most severe COVID-19 patients require urgent care. Some other measures such as ambulance handovers did show signs of improvement this week, but the overall situation is likely to remain extremely challenging for trusts through the rest of the winter.
Key headlines from the winter sitreps (11 – 17 January):
- Adult critical care bed occupancy is rising quickly, despite many more beds being opened. Nationally, 86.5% of these beds are occupied, with London particularly stretched at 92.7%. There are now 5,677 beds open, 29% more than the start of December and 54% higher than a year ago
- overall, general and acute bed occupancy fell slightly this week to 87.2% (down from 88.7% last week), with a very similar number of beds open. The proportion occupied remains lower than last year, even though fewer beds are open, but the additional demands of COVID-19 means this will still feel very busy
- ambulance arrivals were again much lower this week compared to what we would usually expect, as the national lockdown has an impact on activity (12,293 per day, 9.0% lower than a year ago). Handover delays improved considerably from last week, with 12.6% delayed by 30 minutes or more (down from 17.2% last week) and 3.9% delayed by 60 minutes or more (down from a record high of 6.4% last week)
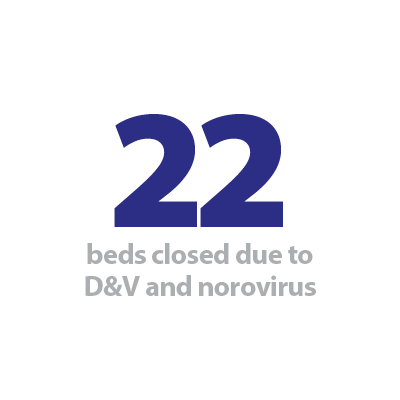
- the number of long stay patients, beds closed due to diarrhoea and vomiting and norovirus and the prevalence of flu, all remain much lower than last year.
The main story in January across the sector is the huge volume of COVID-19 patients being admitted to hospital, and while we might be starting to see signs that the large daily increases are beginning to level off, the number requiring care remains extremely high. Trusts are opening as many critical care beds as possible but demand has never been higher, and in London and the South East over 90% of these beds are now occupied. The national lockdown has led to fewer patients being transported to hospital by ambulance, and as the latest monthly figures released last week showed, the total number of attendances to A&E are lower than we would normally expect at this time of year. However, the disruptive effects of the different peaks of the pandemic have displaced significant levels of routine care. Finding new ways to clear the backlog of care is a key focus for NHS leaders, even during this current peak, which demonstrates just how important the NHS COVID-19 recovery trajectory is for everyone in the service.
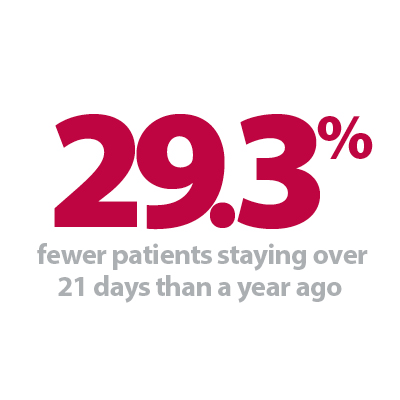
On a positive note, ambulance handovers improved this week, following several weeks of large numbers of patients being delayed at this point in the system. Nationally, a lower proportion were delayed by 30 minutes or more compared to the same time last year, and while some regions do continue to face particular challenges, it is encouraging that the overall figures were much lower this week. Similarly, the number of patients staying in hospital longer than seven, 14 or 21 days remains much lower than last year, as the ongoing efforts of trusts to retain patient flow and ensure capacity is available for COVID-19 patients take effect.
The coming weeks will not be easy as the pressures of COVID-19 and regular winter demand combine with the growing strain being experienced by the NHS workforce. Progress with the vaccine roll-out continues to offer hope for the future, but cold weather, as well as the spread of the new COVID-19 variant to northern regions looms large. Trusts will continue to be asked to make huge efforts to maintain standards of care for all who require it, and the nation owes a huge amount to their dedication in a winter like no other.
Our latest Winter Watch contribution comes from Craig Harman, ambulance and community response director at St John Ambulance, who highlights the positive impact that partner organisations can have when joining forces with the NHS. The organisation is working with the NHS to aid the national vaccination programme and provide vital staff resource at a time when NHS staff are working to maximum capacity, as well as dealing with high levels of staff absence through the pandemic.
The role of St John Ambulance in the UK's COVID-19 response
In its biggest peacetime mobilisation, St John Ambulance has been tasked with training more than 30,000 volunteers to help with the NHS England and NHS Improvement COVID-19 vaccination programme. At the same time, it has provided much of its usual winter pressures support to the NHS, with assistance in hospitals and more ambulance crews added to the mix since the pandemic began.
Craig Harman, the charity's ambulance and community response director, leading on its operational delivery of the vaccination programme, talks about the achievement.
In 2019 and early 2020, we provided our largest number of winter support hours to the NHS to date. Working in partnerships and among communities up and down the country, we helped on ambulances and with services including flu vaccinations, homeless outreach and first aid for the night-time economy.
But little did we know what was in store for us for the rest of 2020 and beyond. As for most organisations on the planet, but especially those in healthcare, the COVID-19 pandemic has thrown up challenges like no others. On the basis of our strong and longstanding relationship, the NHS called on us to assist and we were standing ready to step up.

Our first challenge was to rapidly upskill our volunteer first aiders to help safely during COVID-19. With our expertise in training thousands in general and workplace first aid every year, we quickly adapted and provided this clinical training. This meant we could continue our ambulance and communities support, as well as assist into hospital emergency departments for the first time.
Within two weeks, we had developed our first ever volunteer course combining e-learning with face-to-face training and placed our first volunteers in Lewisham and Greenwich NHS Trust hospitals. To date, more than 5,000 volunteers have successfully completed this training and our assistance in scores of hospitals nationwide, including in COVID-19 wards, continues to be highly valued by frontline staff and management.

In addition, we have worked with a number of airlines to upskill furloughed and redundant cabin crew, already trained in first aid. We’re proud to say a number of these, inspired by their experience of volunteering with us, have now chosen to follow careers in the NHS and the health sector.
Then, as we approached winter, we began to prepare for our biggest ever challenge – to assist with the NHS' task of vaccinating the nation. But with more than 200,000 hours of patient-facing COVID-19 care already under our belts at that stage, the job of training 30,500 volunteers to give vaccinations and provide care at vaccination centres wasn’t as daunting as it might seem.
Essentially, as the nation’s health reserve, this is what we do. While this particular health emergency required us to move on a greater scale and at a faster pace than before, we were perfectly placed to answer the call. We are of course known for providing first aid cover at public events, which vary in crowd size from hundreds to many thousands. But they all have one thing in common – organisations approach us with their needs and we plan, adapt and respond.

So, working with NHS England and NHS Improvement, we developed our training packages for three clinical roles – volunteer vaccinator, vaccination care volunteer and vaccination patient advocate – within three weeks. We were delighted to deploy our first vaccination volunteer teams on 11 January, into the first seven large scale NHS vaccination centres to start administering injections and caring for people. We continue to train thousands more people each week and, with people from partner organisations like the Royal Voluntary Service swelling our ranks, we’re on target to have 10,000 trained by the end of this month.
At the same time, St John has continued to take some of the winter pressure off the NHS. Although the night-time economy reduced dramatically due to the pandemic restrictions, we began working for the first time with Pharmacy4U to provide post flu vaccination support and mobile units. We have continued with our ambulance and hospital support, our falls service (attending emergency calls for those who have fallen in their home) and our homeless outreach services have never been in such demand. In fact, since November, St John has provided nearly 50,000 hours of winter support.
First and foremost, St John owes these achievements to the dedication and expertise of our wonderful volunteers who give their time to serve humanity week in, week out. Another reason for the charity’s success, highlighted in particular during the pandemic, is its history of working in partnership and its focus on local connections.

Our work with charities and businesses to onboard thousands of vaccination programme volunteers is a good example. And, while these new volunteers will join virtual St John units, those units are being managed by our existing network of district managers – real people on the ground. Working with technology, these local leaders will play key roles in ensuring the smooth deployment of vaccination volunteers to centres as more open around the country. We have empowered local leadership teams to act locally, based on local needs, with support from the national team when they need it. I believe maintaining human connection will be vital in keeping our people motivated in the testing times ahead.
No room for complacency as NHS trusts face sustained pressure
Responding to the latest winter reporting data from NHS England and NHS Improvement, the director of policy and strategy at NHS Providers, Miriam Deakin said:
"COVID-19 continues to have an unprecedented impact on the NHS, and today’s figures highlight the sustained pressure trusts are facing.
"The number of adults occupying a critical care bed has increased once again, with 54% more intensive care beds open to treat patients than last year. Given the number of people being admitted into hospitals with COVID-19, trusts are doing all they can to ensure there is enough capacity – in terms of beds and staff.
"The national lockdown has been important in helping to reduce ambulance arrivals and the subsequent improvement in handover times this week, as well as keeping any outbreak of flu at bay. The number of people staying in hospital over a week also remains lower than last year.
"In order to slow the spread of COVID-19 and reduce the number of patients being admitted to hospital, it is vital that we all continue to play our part by sticking to lockdown measures. While the vaccination brings hope, we must not be complacent. These figures show clearly the challenge the NHS and its staff still face each day to care for all the patients it needs to.
"The wellbeing of NHS staff continues to be a key priority of trust leaders. We owe the workforce – across acute, ambulance, mental health and community services – so much as they treat COVID and non COVID patients under extremely difficult circumstances, tackle usual winter pressures, and roll out the vaccination programme."