On Monday the prime minster talked through the government's roadmap out of national lockdown. The plan heeded the four evidence-based tests we set out in a letter to government last week. Central to our call for a cautious approach in easing restrictions, was the need to focus on the data and not dates.
The latest COVID-19 and winter reporting data from NHS England and NHS Improvement reinforces that message, showing that although the number of COVID-19 patients in hospital has reduced by 21% when compared to last week, pressure in critical care in particular remains a concern.
COVID-19 data
As a result of the national lockdown, we are seeing numbers falling across the country for a range of measures, including new COVID-19 cases, new COVID-19 hospital admissions, the total number of people in hospital with COVID-19, and those in mechanical ventilated beds. Here are some of the latest trends:
- as of 21 February, COVID-19 patients made up 19% of the total number of patients in England
- on 24 February, 8,644 new cases were reported in England, 21% fewer cases than last week
- hospital admissions also continue to decline. As of 22 February, there were 980 admissions, 26% fewer than the week before
- on 24 February there were 1,931 people in ventilated beds, down by 19% from the prior week.
Winter sitreps data
The data this week shows that demand for NHS services remains elevated, with high bed occupancy and more ambulance activity. Pressure remains steady in critical care and, although the number of COVID-19 patients is declining, trusts are only now starting to think about reducing some of the surge capacity they have opened to deal with the additional patients. This week’s data shows:
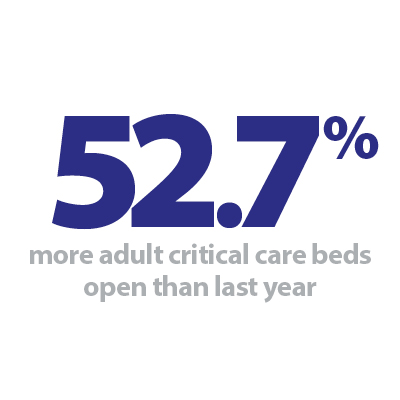
- the number of adult critical care beds open this week is 4.0% lower than last week. This equates to 236 fewer beds open, on average, each day. But this remains 52.7% higher than the same time last year
- the number of adult critical care beds occupied also fell this week by 5%, meaning there were on average, 321 fewer patients each day. This also remains well above the level at the same time last year - 45.8% higher
- this week, the adult critical care bed occupancy rate has fallen to 77.4%, down from 79.7% last week. At the same point last year, occupancy was 81% but this was with far fewer beds open so is not really comparable
- nationally, general and acute bed occupancy rose slightly this week to 85.2%, up from 84.4% last week
- the total number of general and acute beds open fell by 0.4% (354 fewer G&A beds open)
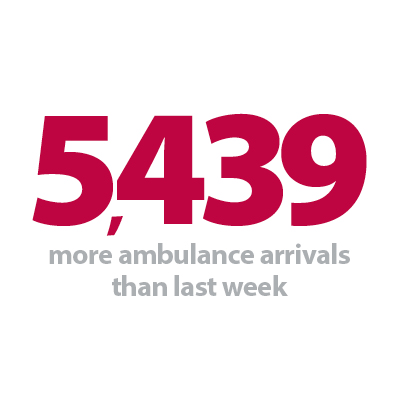
- the number of ambulance arrivals was 6.4% higher than last week, meaning 5,439 more arrivals
- as a result, there was an increase in ambulance handover delays this week. 9.5% of arrivals were delayed by 30+ minutes (up from 7.1% last week) and 2.1% were delayed by 60+ minutes (up from 1.0%)
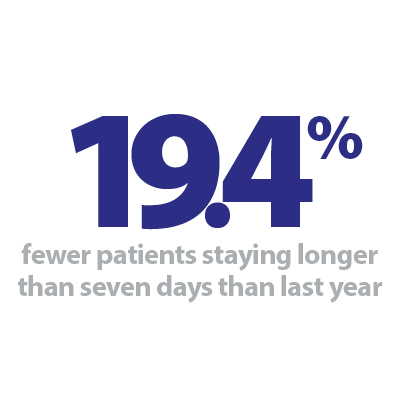
- as we have seen over the whole of this winter, the number of long stay patients, and prevalence of diarrhoea and vomiting, norovirus and flu all remain much lower than last year.
Our reflections
This week spring has been felt in the air with a jump up in temperatures. Coupled with the trends across the COVID-19 metrics, the roadmap out of lockdown, and the promise that all adults can expect to be offered a vaccine by the end of July, things are feeling more hopeful.
As of 23 February 2021, a total of 15.9 million vaccinations have been administered in England. 15.3 million of these were first doses, meaning 27.4% of the population in England have received their first vaccine – real positive news and a huge NHS success.
Staff continue to go above and beyond – across acute, ambulance, mental health and community services – to care for both COVID and non-COVID patients. As the number of COVID-19 patients begins to fall, trusts are already busy stepping up their elective care work to treat those with the greatest clinical need. They are working with partners across their local systems and with the independent sector to tackle waiting lists.
Trust leaders are once again juggling an array of competing priorities, none more important than supporting their workforce and ensuring people get the time to recover from both this latest peak, but the last year in its entirety. This needs to be considered in the context of the ongoing workforce shortages, with the latest data also published today showing that at the end of quarter 3 2020/21, there were nearly 89,000 NHS vacancies. Addressing the workforce shortages must be a core component of the recovery trajectory.
Overall, today's data re-emphasises how vital it is that the government continues to take a cautious and evidence-based approach over the coming months if this is to be the last lockdown.
In this week's podcast Amanda Pritchard, NHS England and NHS Improvement chief operating officer and Chris Hopson, NHS Providers chief executive, discuss how increased innovation, collaboration and rapid turnaround have helped the NHS better manage staff shortages, tackle the increases in demand, as well as protect us all against the virus. They also cover what the future challenges will be for the NHS.
Winter Watch: Questions with Amanda Pritchard
In this episode Adam Brimelow, NHS Providers director of communications, and Chris Hopson, NHS Providers chief executive, speak with Amanda Pritchard, NHS England and NHS Improvement chief operating officer, on the past year, the legacy the NHS will hold, and her own personal message to health care workers.
Progress is being made, but we are not yet out of the woods
Responding to the latest winter reporting data, from NHS England and NHS Improvement, our director of policy and strategy Miriam Deakin said: "Today's data demonstrates that while we are moving in the right direction, with 21% fewer COVID-19 patients in hospital this week, the NHS is still operating under more pressure than normal. Staff are continuing to go above and beyond – across acute, ambulance, mental health and community services – to care for both COVID and non COVID patients.
"Critical care continues to be under particular pressure, despite the number of patients requiring mechanical ventilation reducing by a fifth this week. As bed occupancy reduces, trusts are starting to very slowly reduce their surge capacity, and the number of beds has decreased by 4% this week. However, there are still 53% more critical care beds than at the same time last year – highlighting the sustained pressure the NHS is still under.
"Meanwhile, the data also illustrates that the NHS is delivering for non COVID patients. The total number of people in hospital is rising, despite a fall in the number of COVID-19 patients.
"This week, 5,400 more people arrived at hospitals by ambulance, adding pressure to emergency departments and across the system. This also can lead to longer ambulance handover delays, as seen this week, but overall this is still faring better than last year. The fewer delays, the better placed ambulances are to answer more urgent calls, and get back onto the road quickly to treat more people.
"This week the government set out its roadmap out of lockdown. The plan heeded the four evidence-based tests we set out to the prime minister in a letter last week, on infection rates, NHS capacity, the progress of the vaccination programme, and our ability to tackle new variants.
"Today's data re-emphasises how vital it is that the government continues to take a cautious and evidence based approach over the coming months if this is to be the last lockdown. While progress is being made, we are not yet out of the woods, with the NHS still operating under more pressure, and with less capacity, than it would normally."