Today's blog contains our regular summary of the weekly winter sitreps from NHS England and NHS Improvement, as well as key developments in other related publications that help explain conditions on the ground for trusts right now. It is clear that the COVID-19 pandemic is escalating still further and the pressure on the NHS has never been higher.
The latest monthly performance and activity statistics, also released today, provide further insight into which parts of the service are most affected, while today's NHS sickness absence figures for early January are a stark reminder of COVID-19's impact on the workforce. While the current picture is undoubtedly extremely difficult for those working on the frontline and for patients alike, the progress of the vaccination programme offers hope for the future, and the latest data shows the roll-out gathering pace.
Key headlines from the latest data:
COVID-19 daily figures
- in recent days, the number of new cases across the country has started to fall from the record levels seen last week, although it should be noted there have been large fluctuations in the number of people being tested since the Christmas break
- there has been an increasing number of outbreaks in care homes in recent weeks. In the week ending 10 January, there were 35% more care homes affected than the previous week, which is cause for concern as levels approach those seen during the first wave
- NHS hospital activity data, including the number of new COVID-19 admissions, the number of COVID-19 patients in hospital and the number of patients in mechanical ventilation beds, all point to the severe and still rising pressure in trusts. Regionally, London and the South East have been most stretched, and while these regions may be close to the peak of this particular wave, rapid increases in the Midlands, North West, North East and Yorkshire and South West regions in recent days are very concerning
- sadly, the number of deaths continues to rise, with daily totals in recent days passing the highest figures seen in the first wave in April 2020.
Demand for NHS services
- monthly activity data show a similar number of people attending A&E in December than the month before, but compared to the first wave of the pandemic there are now far more people attending and being admitted for care. Unfortunately, more people are waiting longer in emergency departments, and as well as the known difficulties created in terms of delayed care, congestion and overcrowding, this now carries the additional risk of increasing nosocomial spread of COVID-19. In December 2020, 60% more people waited longer than 12 hours from the decision to admit to admission, compared to the same time last year
- there is a mixed picture in non-emergency care, with cancer and elective care activity in November broadly similar to October levels with some small dips in places. However, the number of people waiting over 52 weeks on the elective care waiting list has increased even further this month to nearly 200,000 (192,169), a huge rise from the 3,097 before the pandemic struck in February
- in the weekly sitreps data, bed occupancy is rising across the country with London, the South East and now South West currently having the highest levels
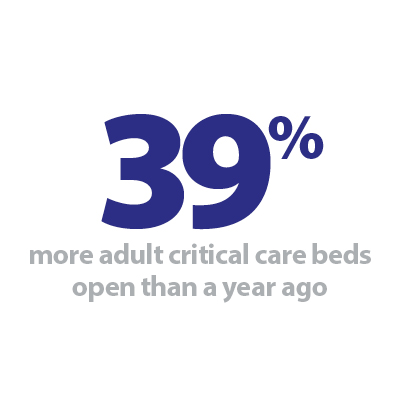
- occupancy of adult critical care beds, which are used for COVID-19 patients who require mechanical ventilation, continues to rise despite extensive efforts to open more of these beds. Compared to this time last year, trusts have worked hard to open 39% more of these beds, and while on a national level beds remain available, in London and the South East there is very little spare capacity at present
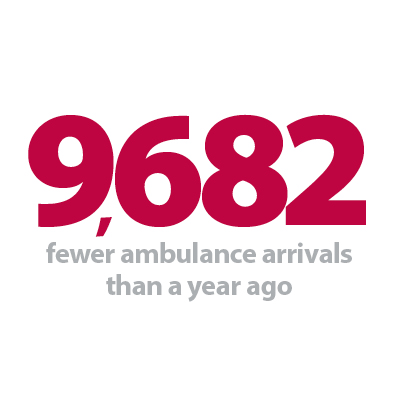
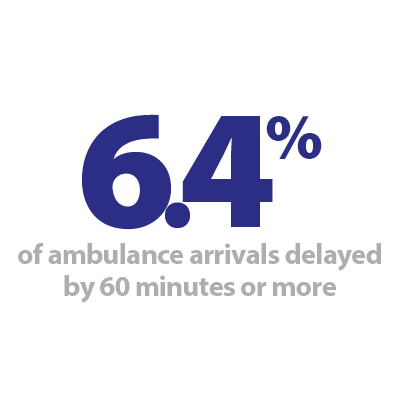
- the number of patients arriving by ambulance was lower in the past week, with the national lockdown likely to be a factor. Worryingly, the proportion of arrivals delayed at handover continues to rise, and in the latest week 6.4% were delayed by 60 minutes or more.
Sickness absence
- Data for December and the start of January shows growing staff absences, mainly driven by a big rise in COVID-19 related absence. On 6 January, 99,934 NHS staff (almost 8% of the total workforce) were absent, of which 49,704 (50%) were COVID-19 related. A month ago, the number absent due to COVID-19 was 27,593, which means there has been an 80% increase in just the last month alone.
Vaccinations
- Since early December more than 2.6 million doses have been administered, of which 15% have been given as second doses. Between 4 – 10 January alone, 1.2 million doses have been delivered as the roll-out programme rapidly gets up to speed. Of the current total, more than half (56%) have been given to those aged 80 and over.
From each of these pieces of evidence it is clear the NHS is in the eye of the storm, and the dedication of trusts and their staff to continue to deliver the best possible care has never been more important. The current wave of the pandemic has seen even greater numbers of patients requiring urgent treatment than the first wave, and with many parts of the service not yet returning to pre-pandemic activity and performance levels, backlogs and growing waiting times for care are likely to increase for some time.
The fast-changing regional picture highlights London and the South East under particular pressure, but as the new COVID-19 variant spreads throughout the country this is quickly becoming the case nationwide. However, progress on the vaccine roll-out offers a positive note for the future, and we watch with anticipation for the effect this will have on the wider population in the coming months.
This week’s Winter Watch contribution is a podcast with our chief executive Chris Hopson. He discusses the challenges faced by NHS trusts in a winter like no other, where the increase in COVID-19 cases has meant increased hospital admissions and pressure to reduce other services, as well as the difficulties that the spread of misinformation and COVID denial pose for health leaders.
Winter Watch: The Perfect Storm
In this episode, Adam Brimelow, NHS Providers director of communications, speaks to Chris Hopson, NHS Providers chief executive, on the current situation in the NHS, the impact of misinformation and COVID-19 denial, and whether the vaccine really is a way out of lockdown. Recorded 12 January 2021.
Performance data highlights how relentless demand is in the NHS
Responding to the latest monthly combined performance data, and winter reporting data from NHS England and NHS Improvement, the deputy chief executive of NHS Providers, Saffron Cordery, said:
"Trusts are under unprecedented pressure, and today's figures highlight how relentless dealing with demand posed by COVID-19, the vaccination roll out and winter pressures is for NHS staff.
"Despite best efforts to address a backlog of care, while simultaneously responding to emergency COVID and non COVID admissions, almost 200,000 people are now waiting over a year for routine care. Trust leaders understand how frustrating this will feel for many, and are doing all they can to prioritise based on clinical need.
"However the latest data showing the numbers receiving cancer treatment, diagnostic tests and operations shows that activity still remains well above the levels carried out in the first wave. This is testament to the lessons learned and the hard work to keep non-COVID services running. We know in some areas this is becoming harder to sustain but it remains a priority of all trust leaders.
"At the same time, staff treated almost 1.5 million people in A&Es in December, though we have seen a worrying increase in the number of people waiting over 12 hours in emergency departments.
"In relation to the latest winter data we know that the number of beds in hospital occupied and those staying over a week in hospital are both continuing to rise nationally.
"Fewer people were taken to hospital by ambulance this week, which is partly a reflection of the national lockdown. But there were more handover delays, with 17% of patients delayed by over 30 minutes and 6% delayed by over 60 minutes. Each delay means a crew cannot respond rapidly to another emergency call.
"We owe so much to our NHS staff – across acute, ambulance, mental health and community services – who are continuing to care for so many of us day in and day out, for months on end, under immense pressures.
"The next few weeks are no doubt going to be the most testing in NHS history, but with compliance to lockdown rules, we know we can reduce the COVID demand and the vaccine continues to offer hope over this extraordinary period."