
Today saw week six of the winter sitreps released, with continued high demand and pressure widespread throughout the system.
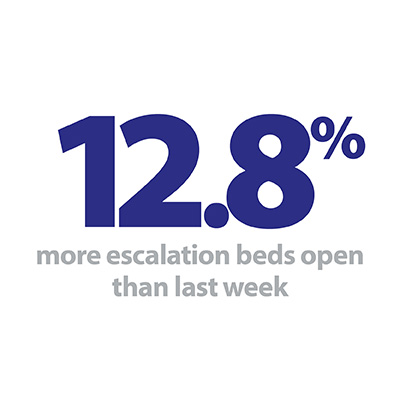
Bed occupancy reached a new high for 2019/20 as 95.1% of all beds were occupied, and 112 trusts out of 132 hit 95% over the week. In response, trusts opened more escalation beds than at any point in the last two years, this week’s figure of 4,441 representing a 12.8% increase on last week alone. More patients are staying longer in hospital, and while ambulance arrivals fell slightly since last week, handover delays are still considerably worse than last winter.
Key headlines from week six’s data include:
- Bed occupancy is 95.1%, the highest it has been all winter.
- This is despite more beds being open than at any time over the last two winters. There were 4,441 escalation beds open this week, 12.8% more than last week as trusts try to meet the surging demand (505 more escalation beds).
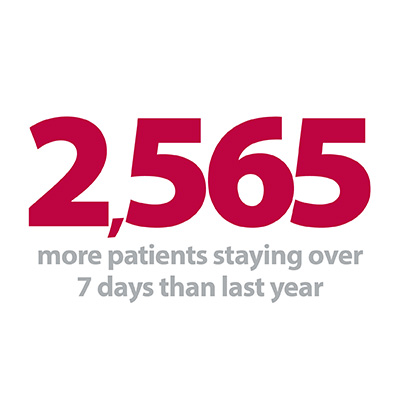
- More patients are staying longer in hospital this week. There were 4.1% more patients staying longer than 21 days compared to last week (674 more patients). There are many more patients staying longer than at the same time last year.
- those staying longer than 7,14 and 21 days are up by 6.1%, 8.5% and 6.7% respectively.
- Beds closed with D&V and norovirus jumped back up to 804 this week, 45% more than last week and 30% more than the same time last year.
- Ambulance arrivals fell by 4.8% this week to 95,738 (4,831 fewer arrivals). Handover delays improved slightly for the week, but are still much higher than last year.
The start of January typically sees a ratcheting up of the pressures experienced before Christmas, and this year appears to be no exception. The national audit office recommends that occupancy in general and acute beds should be no higher than 85% to avoid impacting on the quality of care, but this figure was exceeded by every trust except two in the country this week. In the short term this has detrimental effects on the speed that patients can be moved between departments in a hospital, but over an extended period this can also lead to decisions to cancel planned operations.
The start of January typically sees a ratcheting up of the pressures experienced before Christmas, and this year appears to be no exception.
Indeed, week six saw more patients staying longer than 7, 14 and 21 days than at any point since the exceptionally harsh 2017/18 winter. This is especially worrying when the mild conditions to date in 2019/20 are taken into account, and trusts will be nervously monitoring the forecasts in the coming weeks. The sudden jump in beds closed due to D&V and norovirus this week does not bode well, with 53 trusts now affected.
Ambulance arrivals have been one of the most watched indicators this winter as ultra-high numbers have been recorded each week, but this week they provided some rare positive news as 690 fewer patients arrived per day compared to last week. This led to an easing of handover delays, but these remain persistently higher than last winter as the squeeze on patient flow is felt throughout the system. Across the 2019/20 winter so far, 16.2% have been delayed by 30 minutes or more, compared to 10.8% at the same point in 2018/19. When looking at delays of 60 minutes or more, the 2019/20 figure of 4.3% again exceeds the 2018/19 figure of 2.2% by some margin.
In such trying times trusts seek support from wherever it can be found, and in the guest contribution this week we hear from British Red Cross service manager at Weston General Hospital Michelle Phillips, who tells us about the contribution their workers and volunteers are making to the NHS as part of the ‘first call’ support at home service that helps patients in the South West of England.
How the British Red Cross staff and volunteers support the NHS and patients
British Red Cross service manager at Weston General Hospital Michelle Phillips tells us about the contribution Red Cross workers and volunteers are making to the NHS as part of the 'first call' support at home service that helps patients in the South West of England. It is one of several Red Cross services that have received extra funding to scale up this winter to help deal with the extra pressure.
For us at the British Red Cross, it's all about quality rather than quantity.
Everyone knows our health services are under pressure and the time of doctors, nurses and other professionals is precious. Our 'first call' support at home service is run by a dedicated team of staff and volunteers who can spend as much time as they need with patients to give them the right support when they go home from hospital.
Whether someone feels safe in their own home or is struggling with their finances can be sensitive issues that take time to talk about and it absolutely makes sense for the voluntary sector to be having those conversations. You don't need medical training to help someone with those things but getting them right can have as much impact on their recovery as going home with the right medication.
People are living longer and with longer-term health conditions and that means a small number will turn up at hospital a lot.
For some, a lack of contact with others can leave them feeling lonely, isolated and helpless and they sometimes turn to hospitals for support because they don't know where else to go.
That's where we come in.


We work closely with patients on the ward and serve as a continuous point of contact for them as they prepare to return home from hospital.
We also help NHS staff by liaising with them about their patient's care.
We help people meet mobility goals, transport them to appointments, pick up medication and help them get the shopping in, or put the heating on when they get home.
We look at a patient's individual circumstances and try to identify where people may have unmet needs – where they might be falling through the cracks because they are not getting the help they need at home and in their community.
We speak to occupational therapists, physiotherapists and GPs, building up a picture and sharing that with social workers so they know what a person needs next.
Our service is flexible, adaptable and creative.
We help people meet mobility goals, transport them to appointments, pick up medication and help them get the shopping in, or put the heating on when they get home.
Just a few weeks ago we helped a lady and her husband. He has dementia and had just had a stroke. He needed round-the-clock care but was stuck in hospital because the couple weren't able to find affordable care at home, so it looked like he would stay there, depriving them of a longed-for family Christmas.
Red Cross staff spent four hours hitting the phones to find a care service that could send someone to the couple's remote rural home. Once that was arranged, they drove him home in a private car, because community transport would have been too much for him. Suddenly, Christmas was back on track to the delight of the whole family. And his hospital bed was now free for someone else who needed it.
I think organisations like the Red Cross and others like St Johns and Age UK will play a key role within the NHS in the years to come and we'll need support from the government if we are to provide additional assistance throughout the year and not just during the winter months.
It's also amazing – especially as we celebrate 150 years of the British Red Cross – to think that we are part of a tradition of volunteering that stretches back beyond the very foundation of the NHS to the First World War.
It's astonishing to think that I'm part of a movement that was already helping people in more than 100 hospitals in the UK all year round and has been offering additional winter support this year in 45.
It's also amazing – especially as we celebrate 150 years of the British Red Cross – to think that we are part of a tradition of volunteering that stretches back beyond the very foundation of the NHS to the First World War.
That's an awful lot of people giving their time over decades but it’s crucial we all play our part to ensure that people in pain, discomfort and distress receive the best care for them and support that can hopefully help keep them out of hospital and healthier at home.
Last year, 87% of the people we helped in hospital over winter said we had "helped a lot" and 80% of NHS staff said our being in hospitals had improved their wellbeing.

It’s a real privilege to be part of something that’s having such a positive impact but it’s so easy to get involved and make a difference.
It's a real privilege to be part of something that's having such a positive impact but it's so easy to get involved and make a difference.
The personal rewards are obvious and you feel incredibly proud to think that the time you give is so valued by those who benefit from it.
So if you see us around in your hospital this winter, come and chat to us! We're here to help. And we're always looking for volunteers. If you or someone you know is interested, please visit redcross.org.uk
Patient flow pressures must be tackled
Responding to the latest weekly winter reporting data published by NHS England and NHS Improvement, the director of policy and strategy at NHS Providers, Miriam Deakin said:
"Trusts are doing all they can to support patients and service users this winter to ensure they receive the best possible care. They are working hard to discharge patients, and where appropriate, transfer them into the community so they are closer to home sooner.
However these figures show just how much strain the NHS is under to keep up with growing demand and increased complexities of treatment.
With bed occupancy up to its highest level so far this winter, and length of stays worsening, patient flow through hospitals is suffering.
The NHS is currently facing 2,500 more people staying in hospital longer than seven days compared to last year, and 2,000 more staying for over two weeks.
The number of escalation beds has also jumped up this week, whilst D&V and norovirus has led to an extra 250 bed closures. The total beds open this winter is higher than at any point last winter.
Staff are under extreme pressure and services are being stretched. Patients are waiting longer for a bed or for elective treatment and this is impacting on trusts' capacity to handle unplanned events.
To combat these patient flow pressures, we need to see more focus and investment in community care and, vitally, social care. We must be realistic about the capacity of the health and care system and ensure that we invest in facilities and the workforce so that the NHS is better supported in handling winter pressures."