

The final week of the 2019/20 winter sitreps were released today, marking the end of our Winter Watch campaign. The data shows a system still under considerable operational pressure at a time when trusts typically hope to gain space to tackle backlogs in other areas such as elective care. With the country on high alert due to coronavirus, it will feel far from relaxed in the NHS going into spring.
Key headlines from the week 13 sitreps:
- Overall bed occupancy was 93.9%, a small increase from 93.7% last week, and a daily peak of 94.9% was reached on Tuesday 25 February.
- There were almost 900 fewer ambulance arrivals than last week, but a higher proportion of these had delayed handovers.
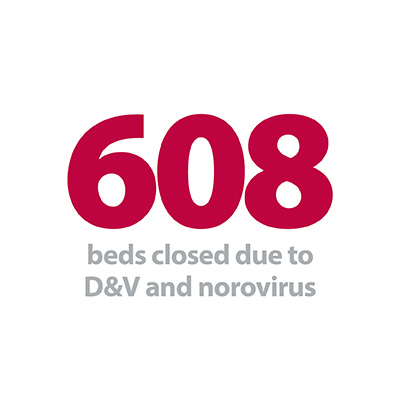
- Beds closed with D&V and norovirus jumped by 19.9% to 608 (101 more beds).
- Continuing the recent trend there were further small reductions in the number of patients staying in hospital more than 7, 14 and 21 days this week, but these all remain higher than last year.
As wintery weather swept through parts of the country, bed occupancy rose to almost 95% early in the week, significantly higher than the 92% limit specified in the 2020/21 planning guidance, which is shortly to come into effect. While trusts are doing all they can to respond to variations in demand for their services, it is clear they have little margin for handling any large increases right now.
The government’s action plan to contain, delay and mitigate against the impact of a wider outbreak of coronavirus was welcomed earlier in the week, but there is understandable concern within the health service and wider community about the potential scale of the issue.
The government’s action plan to contain, delay and mitigate against the impact of a wider outbreak of coronavirus was welcomed earlier in the week, but there is understandable concern within the health service and wider community about the potential scale of the issue. The NHS has extensive tried and tested measures to deal with situations of this nature, and the commitment from government to ensure the service has the necessary resources will be welcomed by trusts. If a widespread outbreak does occur, broader impacts on services may be felt for some time.
In week 13 there were 43,157 patients staying in hospital longer than seven days, 0.6% fewer than the previous week and the lowest total since before Christmas. While the numbers staying longer than seven, 14 and 21 days have all incrementally dropped after reaching an early peak in the first week of 2020, across the whole of this winter there have been considerably more people staying longer than last winter. Focusing on the seven day data-point, there were over 23,000 more people who stayed longer than a week this winter compared to 2018/19, a 4.3% increase. On the 14 and 21 day measures, the respective total increases since last year were 5.8% and 5.3%, as trusts continue to battle to maintain patient flow into more appropriate care settings.
Focusing on the seven day data-point, there were over 23,000 more people who stayed longer than a week this winter compared to 2018/19.
Ambulance arrivals and handover delays were extremely high at the start of winter but since week five they too have eased, with this week's total arrivals figure the second lowest of the 13 week period. Slightly surprisingly, handover delays increased this week, with 12.9% delayed by 30 minutes or more, up from 12.1% last week. This could partly be explained by localised weather-related issues, but trusts suffering higher than average delays will be hoping this is a temporary rise and not a sign of things to come.
In this week's contributor blog we hear from our own Nicole Hardy, NHS Providers' lead press officer for Winter Watch, who reflects on the 2019/20 campaign, the stories that were in the spotlight and the insights gained from trusts around the country.
Winter watch is over for this year, but winter pressures will continue in the NHS
Over the last 13 weeks we have been analysing and reporting on the weekly winter sit-rep figures released by NHS England and NHS Improvement in our Winter watch campaign. Beyond the figures, we have tracked some of the innovations and plans trusts have put in place to help ease winter pressures, despite facing increases in demand and 100,000 staff vacancies. We have heard how winter has played out on the frontline this year, one year on from the publication of the NHS long term plan which set out ambitions to transform and modernise the NHS into a world-class service.
It goes without saying that the health service is largely operating under extreme pressure, and winter is traditionally a highly challenging period for trusts. Coming out of the 2018/19 winter, the NHS was not given the usual chance to recover, as surges in demand continued through summer and into the autumn. Performance against the four-hour standard continued to slip as we headed towards the 2019/20 winter months. Critically, we were also hearing from trust leaders that they knew that they were going to incur significant extra costs this winter and needed additional financial support to help with these unplanned expenses. Although a dedicated winter fund did eventually become available and was greatly welcomed, the delay impacted trusts' ability to plan for winter.
The NHS was also thrust into the spotlight as it became a central focus of campaigning in the lead up to the general election in December.
At the same time, the NHS was also thrust into the spotlight as it became a central focus of campaigning in the lead up to the general election in December. The Conservative party ran a highly publicised campaign, promising an increase in NHS funding in real terms for day-to-day services, as well as £1.8bn of capital investment, which included green flags for six hospitals to begin proposals to modernise their infrastructure. Boris Johnson also committed to finding a solution to the pension taxation issue affecting NHS staff, promised to tackle the social care crisis and pledged to boost workforce numbers. Meanwhile, the Labour party also pledged more money to the NHS – including free prescriptions and car parking, as well as pledging to end privatisation, restore public health grants, and ensure that the NHS becomes a net zero carbon service. No matter your political position, the NHS was at the forefront of voters’ minds across the country in the months leading into winter.
In the weeks that followed, the UK also faced seasonal weather. Although temperatures this winter have been relatively mild, there has been snow and bouts of stormy weather. In recent weeks the NHS has ramped up preparations to contain and delay an outbreak of the coronavirus – an unexpected situation adding to the challenges faced by an already-stretched system. This week the government published an action plan setting out measures put in place to help provide the health service with the resources it needs to tackle the virus, to keep people safe, and to reduce the social and economic impact of a potential widespread outbreak.
To help alleviate ongoing pressures, trusts have put in place winter plans, strategies to keep staff safe and well, developed and implemented innovations, and kept people out of hospital where appropriate by administering care closer to home. In this year’s Winter watch we heard from NHS trusts, across all sectors – acute, ambulance, mental health, and community – as well as from the British Red Cross and Care Quality Commission who work hand-in-hand with trusts to improve services and the experiences of patients and service users.
Key examples from our winter blog series included from Simon Barton, chief operating officer of Sherwood Forest Hospitals NHS Foundation Trust, and separately from Simon Sethi, chief operating officer of Yeovil District NHS Foundation Trust, who shared the preparations they undertook leading up to winter to help prepare for higher demand. For Sherwood, this included re-running their bed demand and capacity model, and listening to both clinical and non-clinical colleagues about their experiences of the previous year to find out what worked well and what challenges were faced. They embedded actions to reduce demand and increase capacity, as well as investing in flu management for the workforce. Yeovil also highlighted the importance of listening to staff.
We've made clear that improving flow is about improving the quality of care our patients receive. Our staff are the experts in what needs to be done to improve care and reduce delays, so by maintaining a continual dialogue with them we can prioritise actions appropriately and effectively support their implementation. It is through talking to them we have developed our daily patient flow focus.
Bev Allingham, deputy chief nurse at University Hospitals Plymouth NHS Trust, also described how their trust promoted the flu jab as a means of protecting staff and patients over winter through Unicef’s Get a jab, give a jab campaign. The drive encourages staff to take up a free flu vaccine and in turn, their trust makes a donation to Unicef, which is spent on programmes to vaccinate vulnerable children globally against life-threatening and preventable diseases such as tetanus. Steffi Camm, fundraising officer at Unicef, describes the tools and resources they provide to trusts to help spread the message across internal communications.
In another contribution, Anne Motley, assistant director of inpatients and unplanned care, and Rita Thakaria, assistant director of community and crisis care, at North East London NHS Foundation Trust discussed how innovative schemes have helped them treat patients in the community this winter. Anne illustrated how they have been able to support elderly people to go home rather than be admitted into a hospital bed, and how they have a step up and step down facility for those patients requiring intermediate care, offering them time to build strength and independence. Additionally, Rita highlighted how the trust has been working in partnership over the past few months with others to triage 999 calls successfully.
The initial phase over the summer period showed approximately 89% of patients [who initially called 999] are believed to have remained at home, all patients received treatment within three and a half hours of their 999 call with a conservative estimate of £65,000 cost savings to the system.
Innovations were a key theme of our contributions this year. North West Ambulance Service director of quality, innovation and improvement Maxine Power discussed the ‘Every Minute Matters’ programme in the North West, now being scaled up due to its success, which works with system partners to reduce the delays in admitting people into emergency departments. Meanwhile, Lewis Thomas, working in site operations at Imperial College Healthcare NHS Trust, described how his trust has improved patient flow and capacity through the implementation of an in-house command centre with digital data solutions.
This innovation is not just about improving operational performance, it is about delivering on the true universal mission which brings each of us into work each morning: continually striving to improve the experience of each and every one of our patients and delivering high-quality patient-centred care.
What’s clear from all these contributions is that the NHS, although stretched and under immense pressure, is continuously adapting and innovating to manage winter and to deliver. From leaders, to clinicians, to nurses, to porters – staff come together as a force to deliver high-quality care and to improve the experience of patients and service users across the system.
However, the health and care system is likely to continue to face significant pressures, and in the coming weeks, staff will continue to strive to tackle the threat of the coronavirus. Traditionally trusts would be moving into the time of year where they could shift attention to handling any backlog built up over winter, but with the threat of coronavirus, this year there will continue to be competing priorities. The weekly winter data may be over for another year, but winter is not truly over in the NHS.
NHS continues to be stretched and under pressure this winter
Responding to the latest weekly winter reporting data published by NHS England and NHS Improvement, the director of policy and strategy at NHS Providers, Miriam Deakin said:
"This week’s figures show that the NHS continues to be stretched and under pressure. The proportion of beds occupied by patients has risen over the past week, with more people staying longer in hospital than at this point last year.
"More escalation beds have been opened this week, there has been a jump in the number of D&V cases and there have been more delays admitting patients from ambulances to emergency departments.
"During this busy period, the health system is coming together to continue to contain and delay the coronavirus outbreak, as set out in the government’s action plan. It is important to highlight that the NHS has extensive procedures in place at national, regional and local levels to tackle situations such as this, and has a sound track-record of handling similar challenges.
"However, if the virus does continue to spread, it is inevitable that the NHS will face increased staffing and cost pressures, and that some patients will have to be prioritised for treatment. It is likely that intensive care units will be particularly affected, but the impact of the virus will be felt beyond acute and ambulance services, in mental health, community services and in the social care sector.
"We welcome the government’s commitment to ensuring that the NHS will have the resources it needs to continue day-to-day business as close to normal as possible. It will be important for the public to play their part by following advice to contact 111 if they believe they have contracted the virus, to use and bin disposable tissues if they sneeze and to frequently and thoroughly wash their hands."