

Week two of the winter sitreps was released today. The data was broadly similar to week one and continues to reflect a sector under serious pressure much earlier in the season than usual.
Week 2
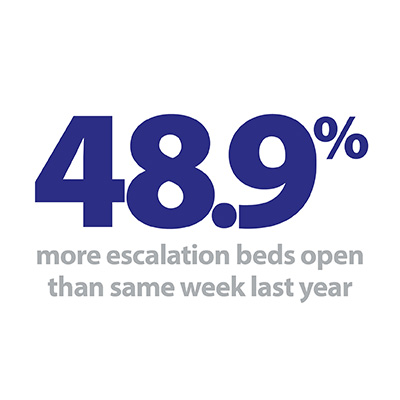
Demand remains exceptionally high, with bed occupancy in week two running at 94.93%, very slightly above last week's mark of 94.90%. The total number of beds has risen by 393 since last week, with escalation beds almost 50% higher than the same point last year. Ambulance arrivals were extremely close to breaking the 100,000 barrier for only the third time on record, and there were noticeably more handover delays than last week. This reflects the pressure across all partners in the health and care system.
Key headlines from the week two data include:
-
Bed occupancy is higher than it has ever been at this point in the season, with 94.93% of general and acute beds occupied
-
There were 97,068 total beds open, 0.4% more than last week (393 more beds) and 1.4% higher than the same point last year (1,346 more beds)
-
There were 3,349 escalation beds open, 5.6% more than last week (177 more beds) and 48.9% more than the same point last year (1,099 more beds)
-
Length of stay data improved marginally this week, but remains worse than at the same point last year
-
There were 99,958 ambulance arrivals this week (171 fewer than last week), but handover delays jumped on both the 30 minute and 60 minute waits
-
Beds closed with D&V and norovirus fell to 892, 13% lower than last week, but still much higher than anything seen last year.
It is clear that trusts already face little room for manoeuvre, with the ambulance handover figures pointing towards worrying issues with patient flow before the usual crunch point in the new year. The number of patients arriving by ambulance this week was just shy of 100,000, 171 fewer than last week, but both weeks so far this season occupy places in the top four all-time weeks for ambulance arrivals. 16.3% of arrivals this week were delayed by 30 minutes or more, up by 1.7 percentage points on last week, meaning 2,322 patients per day were delayed this week.
The length of time people are spending in hospital this week showed a small improvement on the previous week, with those staying longer than 7, 14 and 21 days down by 0.8%, 0.8% and 0.1% respectively.
The length of time people are spending in hospital this week showed a small improvement on the previous week, with those staying longer than 7, 14 and 21 days down by 0.8%, 0.8% and 0.1% respectively. However, there are approximately 5% more patients staying longer than 7, 14 and 21 days compared to the same point last year, when improvements to patient flow were rightly flagged as a rare positive in trying circumstances.
The NHS has opened 393 more beds this week compared to last week, and the total of 97,068 is 1.4% higher than the same point last year (1,346 more beds). The number of escalation beds increased by 5.6% (177 more beds) to 3,349 this week, an unprecedented level for December pointing to trust leaders' concern that we are seeing higher levels of demand earlier than normal.
There was a welcome reduction in beds closed with D&V and norovirus this week, but these illnesses are still having a greater effect than at any point last year. It remains to be seen whether this is the beginning of a downward trend.
Overall trusts will be approaching the Christmas break with trepidation, again relying on the high levels of commitment from staff to meet the needs of their patients.
Overall trusts will be approaching the Christmas break with trepidation, again relying on the high levels of commitment from staff to meet the needs of their patients.
As we continue to publish different frontline perspectives of winter, this week Simon Sethi, chief operating officer at Yeovil District Hospital NHS Foundation Trust, highlights some of the actions undertaken at his trust this year to help manage the pressures they face.
Winter challenge means we must rethink the way we manage demand and flow
The challenge
I'm writing this blog as we recover from a very challenging 24 hours during which we saw 30% more admissions than expected, creating serious bed issues then compounded by a Norovirus outbreak. This is not an isolated experience, as with most trusts across the UK, pressure has been growing over a sustained period - Yeovil's emergency department is currently seeing 28% more people per day than it did three years ago.
Whilst we're still achieving the target of seeing and treating 95% of patients within four hours this year to date, this is becoming increasingly challenging as we attempt to treat more and more patients within a department not designed for such volumes. The scale of the challenge demands that we rethink the way we manage demand and flow across the entire hospital to ensure we provide the best care for our patients and the best working environment for our teams.
So how have we gone about managing these pressures over the last few years? The actions we've taken are in the hundreds but some key themes stand out.
Firstly, we've made clear that improving flow is about improving the quality of care our patients receive. Our staff are the experts in what needs to be done to improve care and reduce delays, so by maintaining a continual dialogue with them we can prioritise actions appropriately and effectively support their implementation. It is through talking to them we have developed our daily patient flow focus.

Secondly, emergency department (ED) crowding isn't just about ED – it's about the whole hospital and system. From improving ward round frequency, to collaborating with community and council teams to create reablement beds outside hospital, to introducing new models of care with local GP practices, the solutions to ED flow often exist outside the department itself.
Finally, we're continually pushing to incrementally improve our system, recognising that small changes, implemented well, can have a significant impact on both flow and patient experience. Each day this week I heard suggestions from hospital colleagues about how to improve our processes and our care. We need to stay agile, continually learning and developing our services to stay ahead of the rising pressures.
I asked Stevan, one of our ED consultants, for his main reflection on how hospitals can manage pressures and help EDs. He told me: "What makes the difference is I’m not just asked my opinion, I also see my suggestions being implemented and know that I’m being listened to. There is also a feeling of belonging across the trust, a knowledge that we're all in it together and can all make a difference. It's never just an ED challenge."
Winter planning
The pressures we're under mean our winter plans are more important than ever. However, since many of our winter actions are now needed all year, it's more challenging to identify what we can do above the usual. Some of our actions this year include:
-
Bolstered medical teams. We generally have about 20% more medical patients from January to March and so have additional senior house officers (SHOs) working to cover this increase.
-
Opening an additional ward to help manage increased medical admissions – we have been able to shut this over the summer due to successfully reducing length of stay.
-
Discharge hit squad. To try and improve weekend discharges we have an additional middle grade or consultant working with an SHO focused purely on discharges at weekends.
-
Nurse transcribing. Our site managers are able to transcribe and complete to take out (TTO) prescriptions to help reduce doctor workload and avoid discharge delays.
-
Social care have introduced a social worker role in ED to prevent admissions for social reasons and expanded their home first service which helps patients get home from hospital earlier and maximises their independence.
-
Our community teams have increased rapid response provision to see people in the community and avoid admissions during winter.

The team
Whilst the actions above have helped us manage pressures, it's evident that we will experience a very tough winter with high demand, risks of norovirus and challenges discharging our most complex patients. That said, in the last couple of weeks I've often found myself standing in site meetings or in our ED reflecting on how lucky we are to have such a positive, hardworking and passionate team. As we approach the festive period, our number one aim needs to be to look after our teams so that they can, in turn, deliver the best for our patients.
Staff going above and beyond to keep patients safe this winter
Responding to the second week of winter reporting data, the director of policy and strategy at NHS Providers, Miriam Deakin said:
"This week's performance statistics show just how hard trusts are working amid challenging winter pressures.
"Bed occupancy rates are higher than all, bar one week, of winter last year. Today's figures reflect how severe pressures are already right across the health and care system. We’re concerned that they're likely to get worse before they get better.
"But trusts are working hard to open more capacity with 400 more beds than last week, showing that the NHS is doing all it can to care for all patients.
"Despite best efforts by paramedics and hospital staff, the time it takes to hand over a patient to be admitted when they arrive in an ambulance has increased this week.
"On a more positive note, D&V and norovirus has decreased by 13% since last week.
"Staff are continuing to go above and beyond to keep patients safe, but we are increasingly concerned that should demand continue to rise throughout the festive period, trusts, their staff and patients may face a very challenging start to 2020."