

This week's data from week 11 of the winter sitreps shows trusts working hard in challenging conditions, largely holding the line on performance across the country. Demand remains high but there were no notable areas where performance slipped from last week.
Bed occupancy is still much higher than trusts would like at 94.0%, but for the second week running this fell by a small amount. Length of stay data and ambulance handovers were very similar to last week, and there was a welcome reduction in the number of beds closed due to D&V and norovirus, down to the lowest level since week five. There may still be difficult times ahead at the tail end of winter if weather conditions worsen, and trusts will remain vigilant over the coming weeks.
Key headlines from week 11:
- Bed occupancy is 94.0%, down from 94.2% last week – positive direction of travel, but still worryingly high.
- There were 97,860 beds open in total, very similar to last week (5 more beds), and 0.3% lower than the same time last year (325 fewer beds).
- Beds closed with D&V and norovirus fell by 11.9% (78 beds) this week to 579, the lowest level since week five when 555 beds were closed.
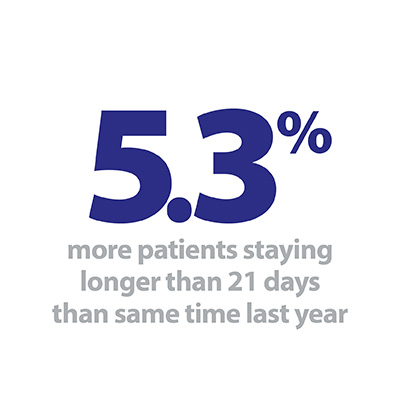
- Length of stay was similar to last week on each of the 7, 14 and 21 day measures, but these all remain considerably higher than last year.
- There were 32 A&E diverts, the highest seen this winter.
- There were 94,510 ambulance arrivals this week, 572 more than last week (0.6% more), but this is 3.8% lower than the same time last year (3,727 fewer arrivals).
- Ambulance handover delays were very similar to last week – of all patients arriving by ambulance, 12.5% were delayed by 30 minutes or more (up from 12.4%), and 2.3% were delayed by 60 minutes or more (down from 2.4%). These are both almost identical to the same time last year.
With extreme weather in the aftermath of Storm Ciara and the arrival of Storm Dennis at the end of the week there was potential for services to be severely disrupted. The higher number of A&E diverts indicates a series of localised issues, but given the destruction and flooding caused by both storms it is a credit to the NHS that performance against key indicators remained largely unaffected.
The higher number of A&E diverts indicates a series of localised issues, but given the destruction and flooding caused by both storms it is a credit to the NHS that performance against key indicators remained largely unaffected.
Overall bed occupancy saw another small reduction, now 94.0%, although this remains higher than the 92% maximum that has been outlined in NHSE’s planning guidance for 2020/21. While the continued efforts of staff are ensuring the elevated number of patients receive the best care possible, it leaves trusts with little room to move if demand picks up suddenly. Preparations for coronavirus are ongoing, and a worrying picture may emerge if the number of patients requiring treatment for this illness increases.
After very high numbers of ambulance arrivals over the first month of this winter, there has been a notable drop since Christmas. For the eighth week in a row the weekly total has been lower than the same time last year, and for week 11 this equates to over 500 fewer arrivals each day. This week a very similar proportion of patients arriving by ambulance had their handover delayed as last week. The figure of 12.5% delayed by 30 minutes or more this week is certainly preferable to the highpoint of 18.1% in week 5, but it still represents almost 12,000 patients delayed this week.
After very high numbers of ambulance arrivals over the first month of this winter, there has been a notable drop since Christmas.
The ongoing workforce shortages experienced in several roles across the country, along with constrained funding mean many trusts have a difficult balancing act to carry out in order to deliver care safely to patients.
Focused A&E inspections over winter help manage pressures and mitigate risks
This week in our guest contribution we hear from Heidi Smoult, CQC's deputy inspector of hospitals and lead for urgent and emergency care. She outlines their programme of focused winter emergency department inspections, and highlights the important role the regulator plays in guiding trusts to make sound decisions through the busy winter period.
For many people in need of care, emergency departments are the first point of contact. National data shows there were 2,114,623 attendances at emergency departments during January 2020 - an increase of 1,210 compared to January last year, and in some fortnightly periods this winter there have been more than 9,000 patients experiencing ambulance handover delays in excess of 60 minutes.
It is in this context that we are repeating our programme of focused winter emergency department inspections where our monitoring of data relating to safety and local intelligence, including patient concerns, identifies potential safety risks. These one day, clinically led inspections use existing key lines of enquiry, but focus specifically on the following five areas which are crucial to maintaining safety during times of high demand:
- Streaming, triage and managing critically ill patients
- Deteriorating patients
- Patient flow
- Work force
- Leadership and culture
So far this year we have carried out 15 of these focused inspections at ten different NHS hospital trusts. Those inspections have shown a variation in the way that hospitals are able to plan for and manage increased emergency attendances and in some cases the negative impact this can have on staff wellbeing and patient care.
It is apparent that system pressures remain a significant issue. When people can't access or are delayed in accessing the care they need in the community, it pushes up demand for acute services, and affects patient flow. Our inspections have seen the direct consequences – overcrowding in emergency departments, delayed ambulance handovers preventing paramedic staff from responding to emergency calls elsewhere, and high numbers of 'super stranded' patients medically fit for discharge but awaiting access to the care and support they need outside of hospital. These are all symptoms of a much wider capacity problem. There is no quick fix, but a collaborative approach involving all parts of the health and social care system working together is essential if emergency departments are to build the resilience required to manage surges in demand.
There is no quick fix, but a collaborative approach involving all parts of the health and social care system working together is essential if emergency departments are to build the resilience required to manage surges in demand.
However, while wider system failures are significant, they are not the only factor impacting on the safety and quality of care in emergency departments. Timely assessment and escalation so that the sickest patients are seen first, maintaining patient dignity, having specialist care available for children and those in mental health crisis and providing a safe environment. These are all things that hospitals can ensure, but that we know are not always happening. In the majority of cases trusts are working hard under immense pressures to safeguard patient safety and dignity. The NHS must continue to strive to ensure that corridor care or the use of inappropriate or unequipped escalation areas do not become normalised. Our focused approach allows us to hone in on such safety concerns and help trusts to quickly identify where they need to make critical improvements.
In some cases, we have used our enforcement powers to ensure trusts take action to mitigate risks to patients. In others we have seen departments that may be struggling but that are better able to maintain safety - supported by strong, involved leadership with clear escalation plans and a focus on the need for constant monitoring and review. Where this is the case there has been whole hospital ownership and trust-wide recognition that maintaining safe, good quality care is about ensuring all departments can support and respond to pressures within the emergency department.
Our inspections are showing that the expected challenges this winter for emergency departments, and indeed the whole health and social care system, have become a reality. Through focused, targeted support and regulation which allows for an immediate response to concerns we are playing our part in supporting trusts to manage the pressures, mitigate any risks and make improvements that benefit both patients and emergency care staff.


Performance has for the most part held steady despite severe winter weather
Responding to the latest weekly winter reporting data published by NHS England and NHS Improvement, the director of policy and strategy at NHS Providers, Miriam Deakin said:
"This week we have seen severe winter weather, with storms affecting many parts of the country, and trusts continue to deal with the impact of coronavirus. Yet frontline staff have clearly been working extremely hard to continue to deliver high-quality care amid these pressures, and today's figures show that for the most part, performance has held steady.
"The number of people in hospital is still much higher than we would want to see, but there has been a slight improvement in bed occupancy, and we have also seen significant headway in the number of people being treated for D&V.
"However, the number of ambulances that have been diverted from busy emergency departments is at the highest its been this winter, potentially due to the bad weather and other localised issues.
"The NHS is facing extreme workforce shortages, and constrained funding, particularly with regard to the capital investment that it needs. Without this, trusts will not be equipped with the resources they need to keep patients safe and treated efficiently.
"We need to see a multi-year capital settlement across all types of trusts, including in mental health facilities, to protect the safety of staff and patients, and to ensure that the NHS continues to offer world class care.
"We also need to see investment in social care and community services to ensure that the health and care system can work together to treat people safely in the most appropriate place – whether that is by admission to hospital or closer to home where appropriate."