

Introduction
Trusts are continuing their efforts to clear backlogs and meet the ambitious elective recovery plan, facing challenging circumstances with a rise in COVID-19 cases and consequent staff absences. The latest figures for 5 October show 10,522 patients in hospital with COVID-19, more than double the number seen last month and 92% more than at the same time last year. In the month of September, over 63,000 staff absences were observed, of which 12% (7,818) were COVID-19 related. As COVID-19 activity in hospitals continues to rise, the additional pressure of this across the entire health and care system is evident in this month's urgent and emergency care figures. Trends once again show an upward tick in A&E attendances and ambulance response times after a small decline the previous month.
This month's performance figures
Each month, NHS England publishes statistics looking at activity and performance across a range of services including urgent and emergency care, routine care, cancer, and mental health. Below we set out the latest trend for each clinical area.
Ambulance: Despite a slight fall in incidents, response times deteriorated in September.
- August registered 69,458 category 1 incidents, a small decrease of about 4% from the previous month (3,012 fewer incidents). Compared to a year ago, incidents are down by 9% but remain 25% higher than three years ago before the pandemic. Ambulance category 2 incidents have also decreased this month by about 3% to 345,642 since the previous month (11,812 fewer incidents).
- National targets are still being missed, with the average response time across England for category 1 and category 2 deteriorating this month, the latter missing the 18 minute target by nearly half an hour.
A&E and emergency care: Another busy month in A&E with about 2 million attendances and the number of patients waiting over 12 hours from decision to admit increasing this month.
- September registered about 2 million A&E attendances, a similar (+0.6%) figure to the one observed in August. There were fewer (-6%) attendances than one year ago (September 2021) and these are now lower (-7%) than three years ago before the pandemic.
- Performance against targets for all A&E types remained relatively similar to last month's (71%).
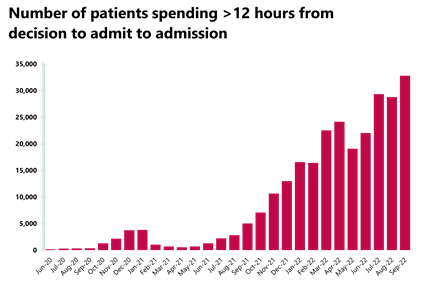
- The number of patients waiting more than 12 hours from the decision to admit to admission has increased again by 14%, compared to the month before, to 32,776 , but this figure is still over 7,000% higher than three years ago.
Diagnostics: Busiest August on record for diagnostic activity, remaining above pre-pandemic levels this month.
- An August record of 2 million diagnostic tests were carried out, with activity increasing by about 3% from the month prior (66,414 more tests than in July). This is above levels seen this time last year, with 10.1% more tests carried out compared to August 2021. Diagnostic activity is also above pre-pandemic levels, with over 98,000 (+5%) more tests carried out compared to August 2019.
- The number of MRI and CT scans have increased compared to last month, up by 2.4% and 3.6%, respectively. However, the number of colonoscopies has decreased slightly by 0.6%.
- The diagnostic waiting list has fallen again this month but remains high at over 1.5 million (1,512,216). Compared to August 2019 before the pandemic, the waiting list has grown by 52%.
Elective care: Activity has increased but so has the waiting list, now at over 7 million.
- In August, the size of the waiting list increased again to 7 million (7,003,256, +2% on the previous month).
- The number of those waiting more than 18 weeks and those waiting more than 52 weeks have both increased by 3% and 2.5%, respectively.
- However, the number of those waiting more than 104 weeks has decreased for the seventh consecutive time by 8% to 2,646. This figure peaked on 22 January at 23,778 but is now 89% smaller. Equally, the number of people waiting more than 78 weeks has decreased again and this figure is now at 50,888.
- The number of admitted inpatient pathways increased (+4%) with over 270,000 inpatient treatments carried out, and the number of non-admitted pathways also increased by about 5% on the previous month, with the NHS delivering over 1 million (1,061,667) elective non-admitted pathways.
- The number of new RTT pathways in August also increased on the previous month from 1,602,408 to 1,649,719.
Cancer: Record levels of activity for the two-week pathway and performance against the waiting time standard has increased slightly for the 62-day pathway.
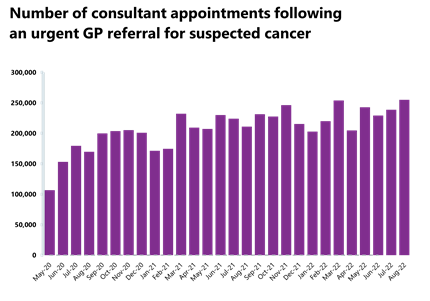
- August 2022 saw record levels of activity for the two-week pathway, with 255,055 patients seen on the two weeks from an urgent referral for a suspected cancer pathway. This is up by 7% from the previous month (16,284 more appointments). Activity for the two-week pathway is above levels seen one year ago (21% higher) and above pre-pandemic levels also (27% higher).
- Activity for the 31-day and 62-day pathways (which aim to start treatment within one month or 62 days from an urgent GP referral) have increased by 5% and 7%, respectively.
- There were 244,661 patients who completed the 28-day faster diagnosis pathway which aims to diagnose or rule out cancer within 28 days of an urgent GP referral for suspected cancer. Compared to last month, this is up by 7%, but this is also above levels seen one year ago (20% more).
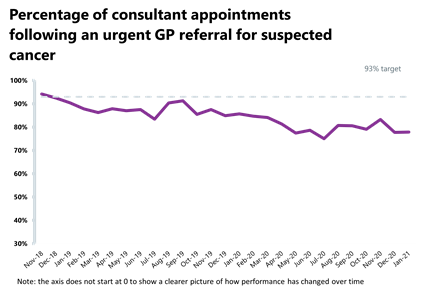
- Performance against the waiting time standard has increased slightly for the 62-day pathway but has deteriorated across the two week, 31-day, and 28-day faster diagnosis pathways. The NHS is still missing all key national targets.
Delayed discharges: Again, a high proportion of patients continue to remain in hospital despite no longer meeting the criteria to reside, highlighting issues with patient flow and the challenges of supporting patients to recover closer to or at home.
- In September 2022, an average of 22,253 patients no longer met the criteria to reside in hospital and an average of 13,305 patients remained in hospital each day. This means an average of 60% of patients remained in hospital per day.
- For the week commencing 26 September, 156,082 had stayed 7+ days since they met the criteria to be discharged, 146,221 had stayed 14+ days, and 132,609 had stayed 21+ days. All three figures represent an increase on August.
Urgent community response
- As of August, 82% of urgent community response referrals were responded to within two hours.
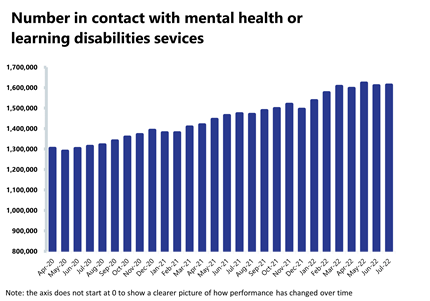
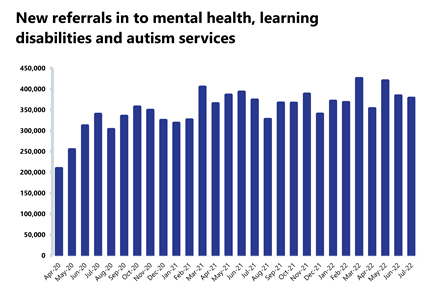
Mental health: Although numbers have decreased for referrals, care contacts attended, and IAPT referrals, these figures remain high, with the second highest number of people in contact with mental services on record at over 1.6 million.
- The number of people in contact with mental health services has increased slightly by 0.2% to 1,612,879 (3,251 more people in contact). This is the second highest number of people in contact with services since records began. Compared to a year ago, this is up by 9% (139,688 more) and this figure is 16% higher (223,770 more) than three years ago.
- Mental health referrals have fallen again this month to 378,125 (-1.4% or 5,509 fewer referrals). Compared to pre-pandemic levels, referrals are up by about 12% (39,792 more than July 2019).
- There were 1.9 million care contacts attended in the latest month, representing a decrease of 2.3% since last month (44,165 fewer). Compared to pre-pandemic levels, care contacts are down by 1.7% (32,905 fewer).
- There were 131,766 referrals received to IAPT talking therapies in July 2022. This is a decrease of 2.7% since the previous month (3,615 fewer).
- In July 2022, there were 685 out of area placements (OAPs), 40 more OAPs than the previous month. Compared to a year ago, this is down by 6.2% (45 fewer OAPs). Compared to pre-pandemic levels, this is down by 12.2% (95 fewer OAPs than July 2019).
Our view
It is mid-point through autumn, and it is clear from today's figures that pressures across the urgent and emergency care pathway are impacting performance, with further increases in ambulance response times and longer waits in emergency departments. Trying to improve performance against existing targets is incredibly challenging for all acute trusts with major A&E departments. Data from this month shows the scale of the challenge with none of these trusts meeting the existing four-hour target, and performance ranging from 31.8% to 86.2% against the 95% standard.
In relation to long waits in A&E before admission after the decision to admit; 38 out of the 124 trusts with a major A&E department reported having no patients waiting 12 hours or more. Although the challenges are widespread across the country there is variation. Out of the 86 trusts who had waits over 12 hours, 28 of these trusts had over 500 patients waiting longer than 12 hours in September – this is three fifths of all waits over 12 hours.
These widespread pressures across urgent care are the symptom of lack of flow through the health and care system. Today's discharge figures show that on average each day only 40% of patients that are medically fit, were discharged. Trust leaders tell us that the delays relate to difficulties in arranging adequate care packages at home, in the community or in social care.
Despite blockages across the system, trusts are increasingly collaborating and working together to tackle waiting lists. This month saw record levels of diagnostic tests and people being seen on the two-week pathway for a suspected cancer, exceeding pre-pandemic activity. Numbers in contact with mental services also continue to exceed pre-pandemic levels.
These data show that in the face of demand continuing to outstrip supply and the knowledge that patients are often waiting longer than anyone would like, NHS staff continue to work incredibly hard, delivering more activity than ever to help patients.
Delivering timely ambulance handover to keep patients at hospital and in the community safe
This month we feature a case study from Walsall Healthcare NHS Trust. The organisation's chief operating officer Ned Hobbs shares how their whole-trust approach to urgent and emergency care has supported timely ambulance handover despite significant pressures.
Walsall Healthcare NHS Trust has delivered the best ambulance handover performance in the West Midlands for 18 of the last 19 months, measured by the percentage of ambulances handed over from West Midlands Ambulance Service to the trust within 30 minutes of arrival.
The trust is a small to medium sized integrated provider of acute and community care, with approximately 550 inpatient beds at Walsall Manor Hospital and is the lead provider for the Walsall Together place-based partnership with NHS, local authority and voluntary sector partners, which is a key asset to the borough. The trust has been on an improvement journey having exited Care Quality Commission special measures just three years ago, in 2019, and has adopted an organisation-wide approach to managing urgent and emergency care (UEC) pathways.
Ned Hobbs, the chief operating officer at Walsall Healthcare NHS Trust, explored what factors have helped the organisation to maintain timely ambulance handovers when many other trusts have struggled to do so. Ned was clear that there is no single intervention, or 'silver bullet' to solve this problem. He described the cumulative impact of multiple improvement interventions all the way along the UEC pathway, both in hospital and community settings, as ultimately supporting timely ambulance handovers. Ned felt that there were four particularly significant factors that contributed to the trust's success.
Firstly, Ned referred to the importance of culture and leadership. He described a very strong ethos at the trust, saying that "the patient who has dialled 999 in our community and needs conveying to hospital is our patient – it is our responsibility to ensure they are promptly handed over to the emergency department (ED)". This culture extends well beyond the ED itself and has been identified in external visits from NHS England and Black Country integrated care board leadership teams.
Secondly, the trust has worked hard to develop and enhance alternatives to ED for patients with UEC needs. This has included:
- Strong community care navigation centre as a single point of access to community services and rapid response team service to deliver urgent community response 8:00am-12:00am.
- Direct ambulance conveyance to ambulatory emergency care (AEC), frailty service, gynaecology assessment unit, surgical ambulatory care unit and same day emergency care (SDEC) units.
- Integrated front door (community-led, hospital-based service) to support ED, acute medical and frailty services to safely discharge patients back to community settings.
- Co-located urgent treatment centre.
Thirdly the trust has developed its rapid assessment and treatment (RAT) function for ambulance arrivals within ED, utilising an emergency care assessment practitioner workforce that is drawn from both registered nursing and paramedic professions. This skilled workforce is highly competent at initial assessment and initiating treatment plans for patients arriving by ambulance, and the experience of paramedic staff helps foster a strong mutual understanding with ambulance service colleagues.
Last, but certainly not least, Ned highlighted comparatively good patient flow out of ED for patients who need onward care in the hospital. The trust still has difficult days, and Ned emphasised has lots more to do to improve further, but relatively good flow out of ED supports the releasing of ED cubicles to in turn ensure the next patient arriving by ambulance can be handed over. Good flow in Walsall is helped by:
- Multiple SDEC units; ambulatory emergency care (under acute medicine), frailty unit (under geriatric medicine), gynaecology assessment unit, paediatric assessment unit and surgical ambulatory care unit (predominantly under general surgery and T&O) that all contribute to over 48% of non-elective admissions at the trust having zero-day length of stay.
- Proactive pull of overnight admitted inpatients from acute medical unit by both AEC and FES first thing each morning.
- Highly functional discharge lounge, open 7:00am-10:00pm (see ECIST video podcast: ECIST Bitesize Podcast Series - Walsall Manor Hospital Discharge Lounge - YouTube).
- Comparatively low medically stable for discharge inpatients as a result of the Walsall Together partnership.
Despite the progress that has been made in Walsall, the trust is mindful of the risk of increased pressure over the winter months ahead and has approved a place-based winter plan at its public board meeting in October 2022 to build further resilience in UEC.
A&E

Cancer
RTT


Diagnostics


Ambulance


Mental health
Latest data underlines ongoing and serious challenges facing NHS
Responding to the latest performance figures from NHS England, the interim chief executive at NHS Providers, Saffron Cordery said:
"Today's figures underline the ongoing and serious challenges facing the health and care sector as we head into winter.
"Despite the best efforts of trust leaders and frontline staff to deliver more tests, checks and scans – including urgent cancer referrals – the level of pressure across the whole health and care system remains concerning.
"A&E performance and ambulance response times in September reflect pressure across the whole system, with the number of people waiting in A&E more than 12 hours after the decision to admit worryingly high.
"The total waiting list for planned procedures has hit another record with over 7 million people now waiting for care. Yesterday's announcement of an amber alert by NHS Blood and Transplant for blood stocks, which could lead to some non-urgent operations being delayed will pile on further pressure.
"And the risk of a 'twindemic' of COVID-19 and flu, which could further hinder efforts to bear down on waiting times, is also looming large.
"Demand for community services continues to be high and trust leaders are telling us mental health services are coming under particular strain with 1.6 million people – the second highest on record – in contact with their services last month.
"The number of people remaining in hospital despite being medically fit to be discharged, often due to the huge demands on social care capacity and staffing, is staggeringly high. It is concerning that only 40% of patients were discharged when ready.
"Local trusts and their social care partners are working together to ease these pressures but until there is real and substantive investment in social care, delayed discharges will continue to hinder the ability of the NHS to deliver timely care for patients."