
Introduction
Trusts across the country are working under challenging circumstances while undertaking an ambitious catch-up plan to clear care backlogs. Workforce and operational challenges continue to be felt, with staff absences remaining high: between 9 June and 6 July, an average of over 71,000 staff absences were registered, of which 23% (16,413) were COVID-19 related.
Additionally, NHS staff continue to provide COVID-19 care to an increasing number of patients as infection rates soar. Hospital data (13 July) showed over 13,000 beds occupied by patients with COVID-19, representing the highest figure in three months and an increase of almost half since 1 July.
As we saw last month, trusts continue to work tirelessly, increasing activity across their services to tackle long waiting times even when demand climbs. Today's data show yet again the incredible work of staff determined to meet the recovery plan milestones.
This month's performance figures
Each month, NHS England publishes statistics looking at activity and performance across a range of services including urgent and emergency care, routine care, cancer, and mental health. Below we set out the latest trend for each clinical area.
NHS 111: Fewer calls received than in April 2022, but activity is at similar levels compared to the month before.
- There were an estimated 1,740,510 calls received in May 2022, equating to an average of 56,145 a day. This is a decrease of 6,116 calls per day compared to the previous month.
- Of these, 1,481,971 were answered (85.1% of calls received). There were 6.8% fewer calls received since the previous month and a similar number of calls answered since the previous month (-0.6%).
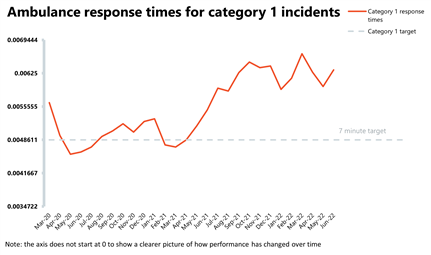
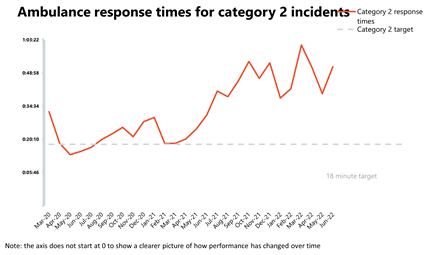
Ambulance: Average response times deteriorated, particularly for category 2, while category 1 incidents are almost 40% higher than before the pandemic.
- In June, the number of category 1 incidents increased by 1.9% compared to the month before to almost 80,000 and were 37.5% higher than three years ago before the pandemic. As for category 2 incidents, June saw a small decrease of nearly 2% to over 372,000.
- National targets continue not to be met and in June the average response time for category 1 calls worsened by 30 seconds to 9 minutes and 6 seconds. The average response time for category 2 also deteriorated remarkably from 39 minutes and 58 seconds last month to 51 minutes and 38 seconds in June, greatly missing the 18 minutes target.
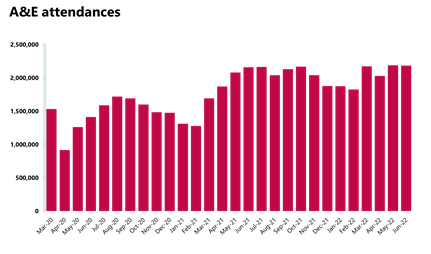
A&E and emergency care: Busy month with high numbers of attendances and admissions, both higher than pre-pandemic levels.
- There were about 2.18 million A&E attendances in June (similar figure to the one observed in May), but this number is 1.1% greater than one year ago and higher (3.6%) than three years ago before the pandemic.
- Performance against targets for all A&E types deteriorated slightly this month.
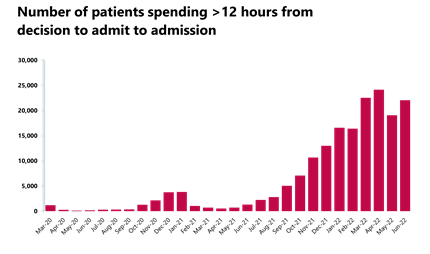
- The number of patients waiting more than 12 hours from the decision to admit to admission increased to 22,034 (15.6%) compared to last month but this figure is still 4,578% higher than three years ago before the pandemic.
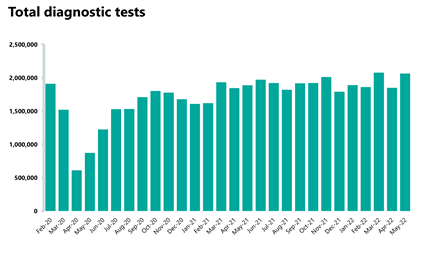
Diagnostics: Although the waiting list is slightly higher than the month before, activity has increased and is currently above pre-pandemic levels.
- There were 2.1 million diagnostic tests carried out in May, the most checks ever for that month and an 11.6% increase from April. Activity is at a higher level to this time last year, with 9.3% more tests carried out compared to May 2021 during the pandemic (176,223 more tests). Activity is above pre-pandemic levels, with 69,425 (3.5%) more tests being carried out compared to May 2019.
- The number of MRI, CT and colonoscopy tests have all increased compared to the previous month, up by 7.1%, 7.7% and 17.9% respectively.
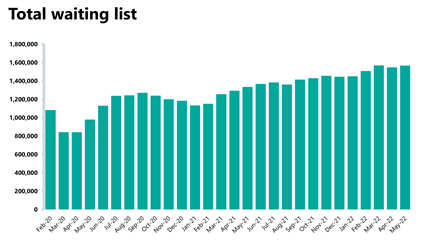
- The diagnostic waiting list has increased and is now at 1,566,168. This is 1% higher than the month before (19,168 more) and is 17% higher than the same time last year. Compared to May 2019 before the pandemic, the waiting list has grown by 48%.
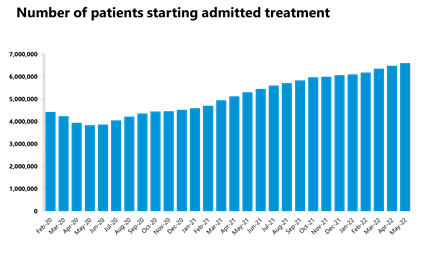
Elective care: Similarly, the size of the waiting list continues to grow but inpatient elective care activity has also increased and those waiting more than 104 weeks has decreased for the fourth consecutive month.
- In May 2022, the size of the waiting list increased again to 6.6 million (2% increase on the previous month), meaning it is about 51% greater than three years ago before the pandemic.
- The number of those waiting more than 18 weeks has decreased by 3% on the previous month but remains 318% greater than three years ago. The number of those waiting more than 52 weeks increased by about 3% in May to 323,093. However, the number of those waiting more than 104 weeks has decreased for the fourth consecutive month by 37% to 8,028.
- Inpatient elective care activity has increased with more admitted and non-admitted pathways (20% and 17% more, respectively).
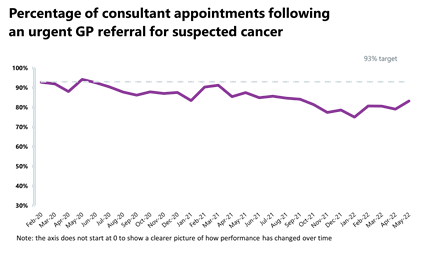
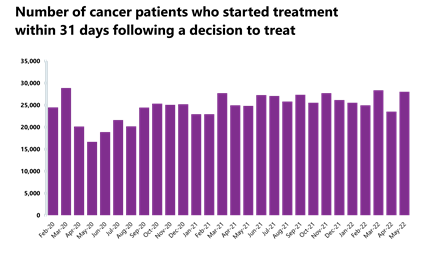
Cancer: Activity for all cancer pathways has increased compared to the previous month and the number of patients seen within two weeks of an urgent referral registered its third highest month on record.
- In May 2022, there were 242,691 patients who were seen within two weeks of an urgent referral for a suspected cancer pathway, the third highest month on record. This is 18.5% higher than April 2022 (37,873 more appointments). Activity for the two-week pathway is 17.1% higher than this time last year during the pandemic, and 20.9% higher than three years ago before the pandemic.
- Activity for the 31-day and 62-day pathways (which aim to start treatment within one month or 62 days from an urgent GP referral) have both increased from the month before by 19% and about 20%, respectively, and activity is above pre-pandemic levels.
- There were 238,452 patients who completed the 28-day faster diagnosis pathway, aiming to either diagnose or rule out cancer within 28 days of an urgent GP referral for suspected cancer. This is up by 19.4% from April 2022.
- Performance against the waiting time standard has improved for the two-week pathway and remained the same for the 28-day faster diagnosis but has deteriorated across the 31- and 62-day pathways. The NHS is still missing all key national targets.
Delayed discharges: A high proportion of patients continue to remain in hospital despite no longer meeting the criteria to reside, highlighting issues with patient flow and the challenges of supporting patients to recover closer to or at home.
- On 30 June there were 22,980 patients who no longer met the criteria to reside in hospital. Of these, 54% remained in hospital on that day (12,400). This is an increase from 52% on the last day of May.
- For the week commencing 20 June, 118,463 had stayed seven+ days since they met the criteria to be discharged, 107,287 had stayed 14+ days, and 93,703 had stayed 21+ days.
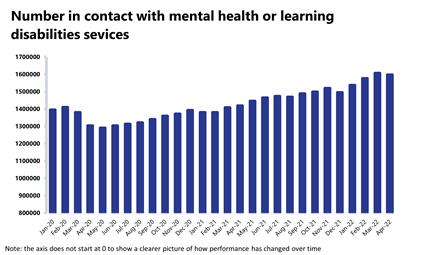
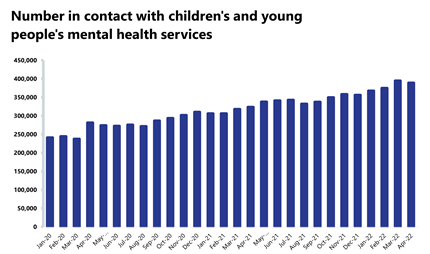
Mental health: Demand remains high, and April saw the second highest number of people in contact with mental health services since records began.
- The number of people in contact with mental health services has slightly decreased this month by 0.6% to 1,596,853 (9,913 fewer people in contact). This is the second highest number of people in contact with services since records began. Compared to a year ago, this is up by 12.6% (178,718 more) and up by 22.5% compared to two years ago (293,215 more than April 2020). In comparison to pre-pandemic levels, figures are up by 18.2% (246,158 more than April 2019).
- Mental health referrals have decreased by 17.0% to 352,866 (72,411 fewer referrals). Compared to a year ago, referrals are down by 3.2%, but are up by 69.0% compared to two years ago (April 2020). Compared to pre-pandemic levels, referrals are up by 16.3% (April 2019).
- There were 1.80 million care contacts attended, a decrease of 16.0% since last month (343,872 fewer care contacts).
- There were 130,064 referrals received to IAPT talking therapies in April 2022. This is a decrease of 21.5% since the previous month (35,567 fewer). Compared to a year ago, referrals are down by 6.9% but are 125% higher than two years ago.
- In April 2022, the number of out of area placements rose to 680, an increase of 1.5% (10 more than the previous month). Compared to a year ago, this is down by 2.9% (20 fewer OAPs).
Our view
This month's data have, one more time, reflected the current pressures trusts are experiencing throughout the country, with ongoing high levels of demand across urgent and emergency care which continue to add significant strains on the pathway, resulting in longer waits for patients. Additionally, we know that the rise in COVID-19 cases in the community translates into more patients in hospital as well as staff absences, which aggravate the already difficult circumstances. Looking ahead, trust leaders remain concerned about the ongoing pressures throughout July as the temperatures keep rising, putting additional strain on urgent care services.
Some of the figures from today illustrate some of these challenges, particularly around patient flow, denoting some of the issues experienced across the social care and health system. For example, we are seeing yet another increase in the number of people waiting more than 12 hours from decision to admit to admission, as well as a larger proportion of patients remaining in hospital after no longer meeting the criteria to reside. Equally, this month's data registered a severe deterioration in category 2 ambulance response times, a reminder of the ongoing pressures being felt by the ambulance sector.
That said, the most notable aspect of these data continues to be the hard work of NHS staff, evidenced once again by the figures we are seeing today. In the face of outstanding pressures, we saw records levels of diagnostic tests carried out for May, now above pandemic levels, the third highest month on record for the number of patients seen within two weeks of an urgent cancer referral, and a fourth consecutive drop in the number of those waiting over 104 weeks for treatment. It is clear that staff are endeavouring to drive recovery while providing quality care during an undoubtedly challenging time.
Leading the way in improving flow and discharge across Bradford District and Craven
Shak Rafiq, the strategic communications and stakeholder engagement lead at Bradford District and Craven Health and Care Partnership, discusses how the use of technology and strong partnership working has helped to improve flow and discharge across the health service.
We are proud of how our place-based partnership has instilled an ethos called Act as One. This sees all partners coming together, acting as one to help us work towards our shared purpose and vision of keeping people 'happy, healthy at home'.
As a result, the Bradford District and Craven Health and Care Partnership has consistently met and exceeded discharge and flow targets, often held up as an exemplar regionally and nationally. Cutting edge technology, innovative practices and strong relationships across partners aligned to a bold vision are the reasons given for the sustained and improved performance. We worked together as partners to respond to the pandemic and manage our collective capacity, given that lack of staff was a major issue for all services. We reviewed our operating model systematically during the summer of 2020, using our data and feedback from our staff teams to optimise flow across acute and community services while continuing with winter planning.
We have been bringing together our workforce using data to provoke conversations between staff groups to facilitate flow, improving outcomes on an ongoing basis and focussing on multi-agency decision making, sharing learning across our two acute hospitals covered by our partnership.
We introduced new roles to assess for discharge in hospital, moving social workers out of hospital to assess people's longer-term needs. The trusted assessors for the council-managed enablement service (BEST) and short-term social care beds work closely with the discharge team and voluntary and community sector (VCS) providers. As a result, we are seeing improved outcomes in terms of capacity and benefits to the person.
Digital innovation
We have advanced digital infrastructures in place across both Airedale NHS Foundation Trust and Bradford Teaching Hospitals NHS Foundation Trust. At Bradford, bed occupancy levels are monitored through our AI powered command centre. The command centre, the first of its kind in the UK, provides real-time information to help make informed decisions on managing patient care and flow. At Airedale, our digital care hub delivers remote monitoring technology such as Telemedicine and MyCare24 but also acts as our multi-agency referral hub providing joint triage of discharges.
We achieve top quartile performance in the country in lengths of stay in hospital. On a weekly basis, hospital admission is avoided for 20-30 people. Despite the workforce challenges in social care, the independent care sector has, on average, supported 40 people a week out of hospital or to short-term home support.
Working with our VCS
We had already invested as a system (adult social care and health) in the VCS, with care navigators working alongside the discharge team, home from hospital and through a multi-agency support team (MAST) to reduce demand on adult social care. Further investment was made into MAST to expand the capacity during winter 2020-2021 which particularly made a difference for people with mental health challenges and alcohol dependency.
MAST is one of our flagship partnership projects. The MAST team consists of VCS organisations based across both hospitals (Bradford Royal Infirmary and Airedale Hospital) delivering interventions and health messaging in emergency departments and across some wards to support the health system and provide support around some of the identified 'pressure points' in the system.
The team works across emergency departments and wards as appropriate, identifying patients, at all stages of their admissions from triage to the ward, who would benefit from mental health, older person's services or alcohol interventions.
During 2020-2021, MAST has achieved the following:
- Supported 1,912 people in hospital, delivering 2,737 sessions of support
- Supported 555 people in the community, delivering 1,643 sessions of support
- Helped reduce the percentage of people feeling disconnected and unsupported from 61.7% to 20%
- Before accessing community support, 47.8% of people expressed they were able to seek support independently. This increased to 72.8% after receiving support.
As a result of the successful implementation of the new models, it was recently confirmed that a further £1.2m in winter funding is being invested into the VCS Alliance to set up wellbeing hubs in communities at place level.
Our system successes
We continue to see great energy and engagement from teams and plan to continue to scale up the implementation. We have already started to integrate this work into our urgent community response pathways and we're also building it into our virtual ward place plans. A few examples of our joint successes are:
- Launching and embedding Right to Reside/criteria to discharge in line with national policy. This has promoted and facilitated timely discharge from the trust along the appropriate pathway
- Goals set around reducing long lengths of stay
- Agreed an updated model of working as a multi-agency team, including joint triage and decision making around discharge pathways
- Developed a dashboard/data set which we continue to work on to provide us with 'one version of the truth' for our whole place.
The Department for Health and Social Care set improvement targets for length of stay in hospital and transfers out of hospital in December 2021, with targets to be achieved by the end of January. We achieved those targets by the first week in January – the best performance across the North East and Yorkshire.
A&E
Cancer
RTT

Diagnostics
Ambulance
Mental health
No let up in pressure on NHS
Responding to the latest NHS England performance figures, the director of policy and strategy and interim deputy chief executive of NHS Providers, Miriam Deakin, said:
"These figures reflect incredibly tough challenges facing the NHS.
"With the country now in the grip of a heatwave, hospitals and ambulance services especially are already feeling the heat from levels of demand normally witnessed in winter.
"Trusts and staff are doing everything they can to get back to and even exceed pre-pandemic activity levels. In May the number of people waiting more than two years for planned treatment came down for the fourth month running while more than 2 million diagnostic tests were carried out – the highest ever for that month. It was also the third highest month on record for the number of cancer patients seen within two weeks of an urgent referral. And 80% of community providers met the new urgent community response target.
"Mental health services saw the second highest number of people in contact with them since records began too.
"Meanwhile COVID-19 is resurgent. With more than 13,000 people in hospital with COVID-19 – up by almost half in less than a month – on one day in July alone almost 27,000 staff were absent due to the virus.
"There is huge pressure on beds, we have more than 100,000 staff vacancies across the NHS currently, and a lack of social care capacity means that hospital patients can't be discharged as soon as they could be to recover closer to home. Delayed discharges were worse in June than they were in May, having a serious knock-on effect on the rest of the health and care system – particularly on ambulances left queuing up outside busy A&E departments waiting to admit patients.
"It's a huge credit to trust leaders and frontline staff that we are seeing progress on some measures, but this is a very worrying picture at a time of year when you would hope to see some respite in these pressures."