

Introduction
Today NHS England published another release of its weekly winter situation reports, providing a snapshot of activity across emergency care and hospitals from 26 December to 1 January.
The 'twindemic' continues to be felt across NHS services. COVID-19 remains a concern, with the number of patients with COVID-19 in hospital rising by almost 1,200 on the previous week, and an average of 9,390 patients in hospital with COVID-19 every day.
This week's flu report shows the influenza-like-illness (ILI) GP consultation rate decreased by about a third, from 31.3 per 100,000 registered population to 20.9 per 100,000. The rate is however higher than the same week in 2019, when it was 12.9 per 100,000. This flu season continues to be more severe than during the pandemic, when there were low flu rates. Today's data also show the extent to which flu is putting additional pressure on already overstretched services, with increasing numbers of beds occupied by flu patients.
We continue to monitor COVID-19 hospital activity and flu indicators as they remain key metrics that sit alongside the winter situation reports and help give us additional context to external factors placing additional stress on the NHS.
The data covering last week once again highlights trends observed the week before, with trusts across England under immense pressure.
Winter situation report (26 December – 1 January)
A&E closures: There were no A&E closures again this week.
A&E diverts: This week there was a total of 17 A&E diverts, the same number as the week before and four fewer than the same week last year.
Ambulance arrivals: A total of 71,211 patients arrived by ambulance in the latest week. This is an increase of 1.5% since the previous week but remains lower than the same time last year (-14.9%).
Ambulance handovers: Nearly 44% of ambulance handovers were delayed by 30 minutes or more, up from 37.4% last week and a considerable increase on 22.8% at the same point last year. More than 26% were delayed by 60 minutes or more. This has risen from 19.9% last week and compares with 9.9% in the same week last year. A total of 54,853 hours were lost to ambulance handover delays – an increase of 51% since last week.
Critical care: Adult critical care bed occupancy dropped slightly this week to 81.5%, down from 81.7%. This is above levels seen in the same week last year (74.4%).
Diarrhoea and vomiting (D&V): The number of beds closed due to D&V and norovirus has increased this week, with an average of 391 beds closed per day. This is up from 337 last week and also above levels seen this time last year (283).
Discharges: There was an average of 20,302 patients each day who no longer met the criteria to reside, a decrease from the week prior. However, compared to last week, a higher proportion (63%, or 12,809) stayed in hospital.
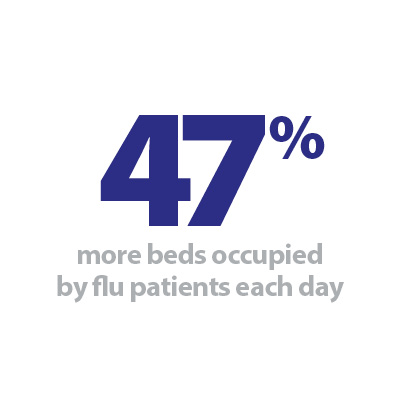
Flu: This week the average number of general and acute (G&A) beds occupied by flu patients each day increased by 47% to 5,105. An average of 336 critical care beds were occupied by flu patients each day this week (26% more than the week before). Compared to the same week last year, the average number of G&A beds occupied by flu patients each day has increased by 13,488% (5,068 more). The average number of critical care beds occupied by flu patients has increased by 21,264% from the same time last year (334 more). These figures are considerably higher compared to this week last year as flu was not prevalent due to COVID-19 restrictions and social distancing.
G&A beds: There were an average of 100,271 G&A beds open each day – 6.1% higher than the same time last year (5,792 more). On average each day, 289 beds were unavailable and void to non-COVID infections. Average bed occupancy remains high at 93.2%. This is a decrease of 5.2 percentage points compared to the same week last year.
Long stay: The number of patients staying in hospital longer than seven, 14 and 21 days has increased since last week (up by 5.9%, 2.3% and 0.9% respectively). Compared to the same time last year, the numbers of patients staying in hospital for longer than seven, 14 and 21 days have all increased (up by 20.6%, 18.6%, and 19.0% respectively).
Neonatal intensive care beds: Occupancy has decreased from last week to 65.5%. This is down from 68.6% last week and compares with 68.2% the same week a year before. The average number of care beds open is at 1,719, 0.5% higher than the week before and 1.6% higher than the same week last year.
Paediatric intensive care beds: Occupancy has fallen this week to 86.3%, down from 88.7% last week. This remains higher than the same week last year (73.7%). The average number of care beds open has fallen slightly to 363 since the previous week (3 fewer care beds open).
Staff absences: There were an average of 59,313 total absences each day this week, of which 12% were COVID-19 related (7,204). The total number of staff absences has decreased from the week before (63,296), and the proportion of COVID-19 related absences has also decreased slightly (down from 13%).
Our view
This week's data continue to highlight the very challenging circumstances the NHS is experiencing. As in previous weeks, hospital capacity remains under serious pressure.
Flu cases in hospital have increased by almost half (47%), with over 5,000 patients with flu in G&A hospital beds, and patients with flu in critical care beds increasing by more than a quarter (26%) to 336. Equally, hospital bed occupancy remains high, with more than nine in 10 G&A beds currently occupied.
Additionally, we continue to see that delayed discharges remain a problem for trusts across the country, with almost two thirds of medically fit patients remaining in hospital, an increase from the week before. This is a reminder of the system wide challenges felt across the health and care sectors.
Similarly, pressures across urgent and emergency care remain high, with over two fifths of ambulance handovers delayed by 30 minutes or more, a figure considerably higher than at the same point last year. As with delayed discharges, this metric signals system wide-issues with patient flow. A total of almost 55,000 hours were lost to ambulance handover delays – an increase of over half since last week.
Workforce gaps also continue to exacerbate these ongoing issues, with vacancies, staff absences and industrial action all contributing to what is a very difficult winter.
Working at scale across Sheffield to manage the winter challenges
Andy Hilton, the chief executive of Primary Care Sheffield reflects the ways working at scale across Sheffield has helped the organisation respond to the current winter challenges.
I'm a general practitioner (GP) in Sheffield as well as chief executive of Primary Care Sheffield – the city's general practice-owned not-for-profit primary and community care provider – so I get a fairly unique view of the interplay between general practice and the rest of the health and care system.
What I've been struck by this year is that the pressures from last winter never really went away – demand for services remained critically high all through the summer. It's clear that the ongoing pressures are not driven purely by seasonal changes, but more a chronic mismatch between resource, capacity, and demand.
Given that we are already starting from this high-water mark I think that what general practice in Sheffield is achieving is remarkable. Indeed, the whole system seems to have found an extra gear as we prepare for what undoubtedly will be the most difficult winter we have known.
Delivering additional appointment capacity at-scale
One of the ways in which Primary Care Sheffield has been able to support services has been to deliver additional appointment capacity at-scale. One of the great benefits of this has been the flexibility we are able to offer – ramping up capacity when and where it is needed.
For example, earlier this month our team were able to quickly launch additional GP paediatric streaming appointments for A&E. This in the face of surging demand which was placing unprecedented pressure on primary care as well as the emergency department at Sheffield Children's NHS Foundation Trust. We also increased advanced nurse practitioners (ANP) and home-visiting capacity at the beginning of November and stand ready to do more when required.
What could that look like? Well, last winter that included a direct access service for domiciliary care providers to garner remote GP advice and a paramedic visit, separate hot-hub capacity for COVID-19 positive patients, providing 'active-recovery' support for domiciliary care clients, additional citywide ANP appointments, creating a new citywide paramedic home-visiting service, and a phlebotomy home-visiting service. All of this improved access for patients, reduced pressure on primary care, ambulance service, domiciliary care, and prevented avoidable admissions into secondary care.
We have also worked with the integrated care system to deliver a third-party provider primary care staff bank which helps us attract the staff to deliver additional capacity at pace. This meant that practices in 2021/22 Sheffield were able to create a total of 85,000 additional appointments outside of core general practice.
The domiciliary care visiting service was based upon providing direct primary care access to our most vulnerable patients to avoid 999 calls and admissions. It was funded with a one-off pot of money to run for 12 weeks. We thought we'd need ongoing nurse capacity to keep people at home but found what was required was rapid access to GPs before the carer left the premises, and a follow up visit. It proved difficult to quantify, but best estimates suggest 50% of patients visited avoided at least an ambulance attendance, if not an admission; which is an amazing outcome. However, activity was lower than expected due to the short-term nature of the service, which meant by the time carers were engaged the service was closing.
The citywide hot-hubs, ANP appointments and paramedic and phlebotomy visits were much better utilised, as practices were booking their patients directly using the appointments as same-day over-spill.
Working together on primary and community transformation
Strategically we require underpinning robust contracts with longevity to fund and grow our infrastructure to be able to continue to step up and down services at pace. Our biggest operational challenge remains the difficulties with IT system interoperability.
At the same time as providing that additional capacity we must not take our focus off the longer-term work to innovate and redesign mental health, elective care and urgent care services. In Sheffield we are leading the way nationally in these areas. That's one of the reasons why Primary Care Sheffield was named as 'primary and community care provider of the year' at this year's HSJ Awards.
Primary Care Sheffield, Sheffield Health and Social Care NHS Trust and voluntary sector organisations continue to work together on primary and community mental health transformation. The aim is to work with people who are falling through the gaps in current mental health care and is designed to prevent people's mental health from worsening, reduce A&E attendance, and improve their quality of life. The service is currently being trialled in some of the most deprived parts of the city.
At the same time our clinical assessment support and education service (CASES) is an elective care re-design programme that aims to reduce the pressure on elective services and makes sure that patients in Sheffield receive their care in the most appropriate setting from the most appropriate clinician. The last year saw more than 23,000 patient referrals being GP peer reviewed with advice and guidance offered to referring GPs and learning shared through briefing documents and learning events. Overall CASES has resulted in an average 23.7% reduction in referrals across all specialties. The service delivers high quality education and upskilling to Sheffield primary care clinicians based on evidence gained from the screening process.
At the moment we are hanging in there – like the Wile-e-Coyote's final gravity defying moments after running off the edge of a cliff.
However, without longer-term transformation work alongside proper national strategies for primary care workforce and estates – the eventual plummet onto the rocks below is inevitable.