
Introduction
Today the weekly winter situation reports by NHS England were published, alongside the monthly performance and activity statistics. As always, these provide a valuable insight into the situation on the ground as trusts continue to brave an exceptionally hard winter for the NHS.
These data show how staff are working tirelessly under severe pressures to deliver an ambitious catch-up plan, while dealing with high demand, system wide pressures, surges in seasonal illnesses and strikes which have led to 137,000 appointments being postponed.
Meanwhile, the monthly activity and performance statistics offer useful context to the state of the sector. Key points include:
Ambulance activity: The number of category 1 incidents decreased compared to the month before, but remain higher than the figures observed before the pandemic. Average response times for category 1 and category 2 incidents improved, particularly the latter (from over 1.5 hours to just over half an hour).
Emergency care activity: The number of attendances dropped by 14% but remain close to 2 million. The performance against the targets increased for all A&E types, and the number of patients waiting for more than 12 hours from the decision to admit to admission has decreased by about 22%.
Elective care: Elective care activity decreased from the previous month. The waiting list remains very high at 7.2 million and we saw an increase on those waiting for more than 18 weeks.
Diagnostics: Activity also decreased this month, but remains slightly above pre-pandemic levels. However, there was a small reduction in the diagnostic waiting list.
Cancer: Although activity decreased in all cancer pathways, it remains above pre-pandemic levels. Performance against the waiting time standard has improved for all pathways but the key national targets are still not being met.
Urgent community response: As of December 2022, 76% of urgent community response referrals met the two-hour standard for delivery.
Winter situation report (30 January – 5 February)
A&E closures and diverts: There were no A&E closures again this week. There were a total of 17 A&E diverts, seven more than the week prior.
Adult critical care: Critical care bed occupancy was similar to last week at 79.4%, a higher figure compared to the one observed one year ago (75%).
Ambulance arrivals: A total of 80,502 patients arrived by ambulance in the latest week. This is an increase of 2.6% since last week and down by 5.3% compared to the same week last year.
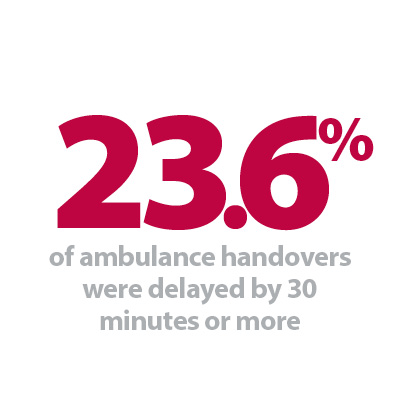
Ambulance handovers: 23.6% of ambulance handovers were delayed by 30 minutes or more, up from 18.2% last week. 9.6% were delayed by 60 minutes or more, this is up from 5.6% last week. A total of 16,113 hours were lost to ambulance handover delays.
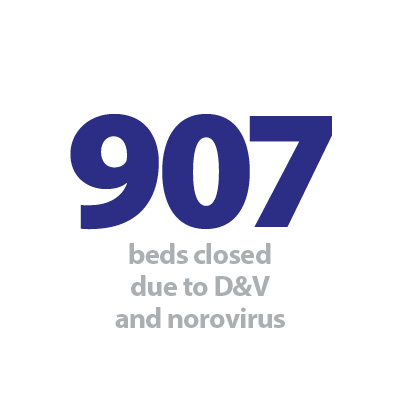
Diarrhoea and Vomiting: The number of beds closed due to diarrhoea and vomiting (D&V) and norovirus has increased a lot this week, with an average of 907 beds closed per day. This is up from 495 last week and above levels seen this time last year (382).
Discharges: There were an average of 23,772 patients each day who no longer met the criteria to reside, an increase of 256 patients from the week prior. However, compared to last week, a similar proportion (58.8%, or 13,975) of patients remained in hospital this week.
Flu: This week the average number of general and acute (G&A) beds occupied by flu patients each day decreased by 25.6% to 895. An average of 66 critical care beds were occupied by flu patients each day this week (24.1% fewer than the week before). Compared to the same week last year, the average number of G&A beds occupied by flu patients each day has increased by 2,567% (862 more).
G&A: There were an average of 101,375 G&A beds open each day – 4.1% higher than the same time last year (3,963 more). On average each day, 260 beds were unavailable and void to non-COVID infections. Average bed occupancy remains high at 94.4% and slightly up from last week (94%). This is 1.8 percentage points higher compared to the same week last year.
Long stay: The number of patients staying in hospital longer than seven, 14 and 21 days has slightly fallen this week, by 0.3%, 0.7% and 0.3% respectively.
Neonatal intensive care unit: Occupancy has remained similar at 66.8% compared to 66.9% last week, and up from 67.4% the same week a year before. The average number of care beds open is at 1,706, 0.8% more beds open compared to last year.
Paediatric intensive care unit: Occupancy has increased this week to 83.5% (it was 81.4% last week) However, this is still higher than the same week last year (75.4%). The average number of care beds open has increased by two beds to 359.
Respiratory syncytial virus (RSV): An average of 25 paediatric beds were closed this week due to RSV symptoms, down from 30 last week and up considerably from three last year.
Staff absences: There were an average of 49,333 total absences each day this week, of which 9% were COVID-19 related (4,522). The total number of staff absences increased from the week before but the proportion of COVID-19 related absences slightly increased by one percentage point.
Our view
Despite experiencing one of the toughest winters for the NHS, the hard work of trust leaders and staff across the service is showing promising results. Despite high demand for urgent and emergency care services, ambulance response times have considerably improved.
Equally, diagnostic and cancer activity remains above pre-pandemic levels, and performance against the cancer waiting time standard has improved for all pathways in this latest release.
That said, we are still observing ongoing issues with high bed occupancy above safe levels and high proportions of patients staying in hospital for longer than they need to, challenges no doubt exacerbated by workforce absences and continued industrial action. Winter pressures therefore continue to be felt in trusts across the country.
Tackling backlogs and reducing waiting times at St George's
Shamim Umarji, clinical director for surgery at St George's University Hospitals NHS Foundation Trust, discusses how the organisation is tackling backlogs and reducing waiting times through their dedicated surgical hubs.
It's no secret that the pandemic has had a significant impact on people waiting for elective care across the country. That's something no one wants to see, let alone clinicians like myself, and my colleagues who just want to deliver the best possible care for patients. Tackling backlogs and reducing waiting times is a huge priority here at St George's – and thanks to our dedicated surgical hub we are doing just that, treating about 600 people a month.
Since it opened in June 2021, the hub – which is based at Queen Mary's Hospital and supports patients in south west London – has carried out 7,000 operations, from plastic surgery procedures for skin cancer and orthopaedic hand operations, to cystoscopies for cancer. Its four dedicated operating theatres and recovery areas are protected to perform high-volume, low-complexity surgical day cases to allow more patients to be seen more quickly, and in a more convenient location.
There are so many benefits to doing this. Clearly, the patients who have had surgery now have a better quality of life and are no longer in pain. They will have recovered more quickly than previously and are also less likely to deteriorate and end up needing emergency treatment. But it also means we can keep our theatres at St George's free for urgent and emergency operations.
We are now ahead of our plan for 52-week waits, which is really encouraging to see. Our waiting lists are shorter than the national average, and we are on track to meet NHS England's target to eliminate waits of more than a year-and-a-half by next month. That's not to say it's all been a completely smooth process, and we have learned things along the way, too. For example we have drastically improved the efficiency of the hub and how it is used, by improving booking numbers and reducing patient cancellations through better planning. It's resulted in a 48% increase in use from 2021/22 to 2022/23.
We are still exploring ways to utilise the hub better. Ultimately, our priority is doing the right thing for our patients – so we are looking at being more efficient and finding new and innovative ways of working, such as adding to the type of procedures we currently do here. Quality and safety remain paramount.
And we'll continue to work closely with our partners. The hub provides extra capacity, not just for our surgeons, but teams across London. In south west London we also have an acute provider collaborative, where trusts tackle challenges as one – because, ultimately, we all want what's best for our patients. This isn't the time to be competitive – in fact, it's really quite the opposite as we move forwards as a sector by offering mutual aid.
We'll continue to work hard to ensure patients who are waiting for surgery are seen quickly – but I'm also looking forward to seeing what we achieve in the future and to build on the foundations already established.