Introduction
Today, NHS England published the latest figures for performance and activity across physical and mental health services. Below we detail the trends across specific services. These statistics, as always, offer valuable insight into the pressures facing the provider sector.
With winter fast approaching, trusts continue to work incredibly hard to clear backlogs. The latest data highlights the progress being made in bringing down the number of patients who are waiting the longest despite significant challenges facing the sector. October saw more beds occupied by Covid-19 patients again, up by over a quarter from the month before. As well as this, the NHS remained under pressure from ongoing industrial action, adding to the already challenging operational context as we head into winter.
This month's performance figures
Each month, NHS England publishes statistics looking at activity and performance across a range of services including urgent and emergency care, routine care, cancer, and mental health. Below we set out the latest trend for each clinical area.
NHS 111: Over 55,000 calls a day were received in September, with 24% more calls answered than before the pandemic.
- In September 2023, 1.65m calls were received by NHS 111 and of these 1.43m calls were answered. This equated to 55,079 calls answered a day in September.
- NHS 111 answered 24% more calls compared to four years ago, before the pandemic (September 2019).
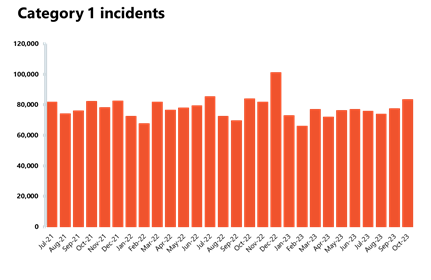
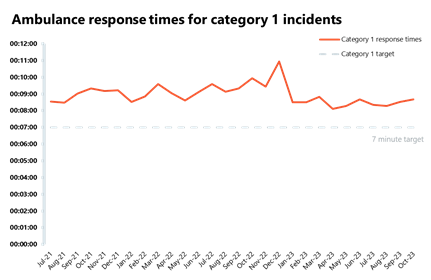
Ambulance activity: A busy October for ambulance services, with over 724,000 total incidents, up from September and above levels seen last year (676,000). Average response times deteriorated for both call categories.
- October saw a 7% increase in ambulance category 1 incidents to 83,326 (5,773 more incidents). There were around 1% fewer incidents compared to a year ago, but incidents were 35% higher than four years ago, before the pandemic in October 2019. Ambulance category 2 incidents also increased this month, with 16,759 more incidents. Compared to four years ago, they were down by about 4%.
- National targets were not met again in September, and the average response time across England for category 1 and category 2 calls increased.
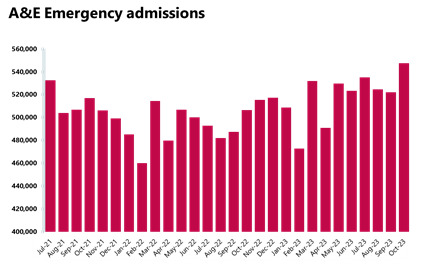
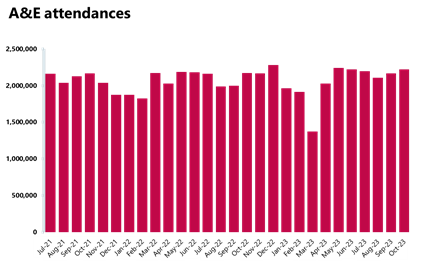
A&E and emergency care: Busiest October on record for A&E attendances, with almost 2.22 million people attending A&E services.
- October saw 2,219,000 A&E attendances, a number 2.5% higher compared to the month before and also 2% higher than last year. Compared to four years ago before the pandemic (October 2019), this figure is slightly higher (+2%).
- Performance against targets for all A&E types decreased.
- The number of patients waiting more than 12 hours from the decision to admit to admission has increased by 35% to 44,655 since the month before. This figure is over 6,050% higher than the same month four years ago before the pandemic (October 2019), when this number was 726.
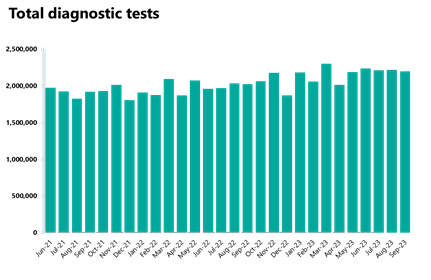
Diagnostics: Highest September recorded for diagnostic tests carried out (2.2m), but the waiting list increased again and remains much higher than before the pandemic.
- In September 2023, 2.2m diagnostic tests were carried out, a slight decrease of 0.9% from the month before. Activity for the latest month is 8.6% higher than one year ago (174,960 more tests) and is 13% higher than pre-pandemic levels, with 253,028 more tests carried out compared to September 2019.
- The number of MRI, CT scans and colonoscopies all decreased compared to last month, down by 2%, 1.4%, and 0.3% respectively.
- The diagnostic waiting list increased this month by 1% but remains over 1.5m (1,582,684). This is 2% higher than August last year and 55% higher than September 2019 before the pandemic.
- The number of patients waiting six weeks or more for a test is at 26.3%; this is down from the month before (27.5%) and is still missing the 1% target.
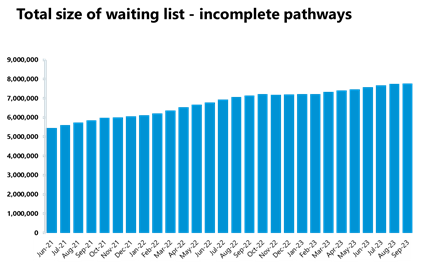
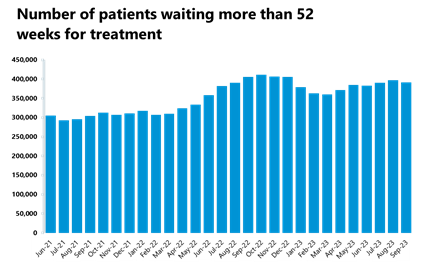
Elective care: Activity has decreased in September for all pathways except non-admitted pathways. The waiting list increased again, now at an all-time high of 7.77m.
- In September 2023, the size of the waiting list increased slightly by 0.3% and is now at a new record high of 7,771,057 (7.77m, 26,027 more people than the previous month). The size of the waiting list is still 70% greater than four years ago just before the pandemic.
- The number of those waiting more than 18 weeks has increased compared to the previous month (+1.3%), but the number of those waiting more than 52 weeks decreased and is now at 391,122 (-1.4%).
- The number of those waiting more than 104 weeks also decreased by 14% to 227.
- Inpatient elective care activity, with the exception of non-admitted inpatient pathways, has decreased in September 2023 from the previous month.
- The number of admitted pathways decreased slightly (-0.7%) from the previous month, and the NHS delivered over 1.1m (1,162,843) elective non-admitted pathways. The number of new RTT pathways in August decreased on the previous month from 1.73m to 1.71m.
- In September 2023, 83.6% of patients on the waiting list were unique patients, therefore the estimated number of unique patients on the waiting list is 6,499,150.
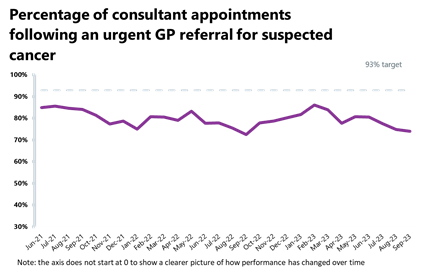
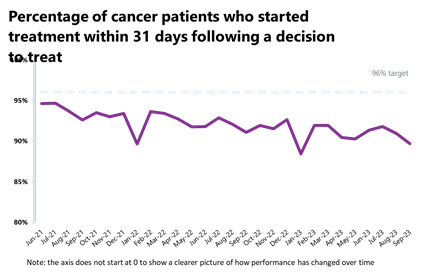
Cancer: Activity is down this month but remains higher than pre-pandemic levels. Performance against the waiting time standard has deteriorated for all pathways and all targets are still being missed.
- In September, there were 258,858 patients who completed the 28-day faster diagnosis pathway which aims to diagnose or rule out cancer within 28 days of an urgent GP referral for suspected cancer. This is down by 2% from the previous month but up by 8% from last year and 15% from two years earlier.
- Activity for the two-week, 31-day and 62-day pathways registered the highest September on record, with increases of 32%, 7% and 14% from before the pandemic, respectively.
- Performance against the waiting time standard has deteriorated for all pathways and the NHS is still missing all key national targets.
Delayed discharges: A high proportion of patients continue to remain in hospital despite no longer meeting the criteria to reside, highlighting issues with patient flow and the challenges of supporting patients to recover closer to or at home.
- On 31 October (a Tuesday), there were 23,469 patients who no longer met the criteria to reside in hospital. Of these, 54% remained in hospital that day.
- For the month of October, there were an average of 22,486 patients who no longer met the criteria to reside. Of these, an average of 55.6% remained in hospital. This is slightly higher than the previous month (55.1%).
Urgent community response:
- As of August, 85.3% of urgent community response referrals met the two-hour standard, up from last month.
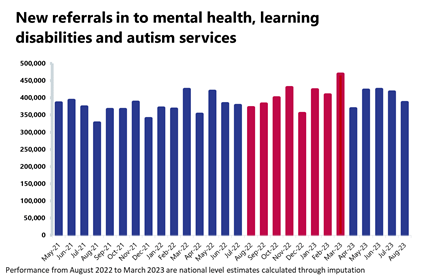
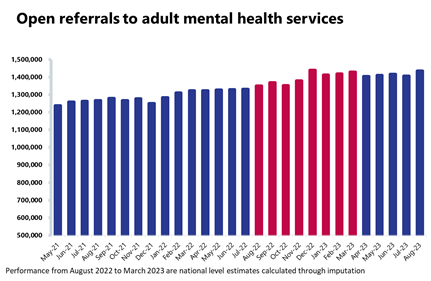
Mental health: Referrals have fallen again but remained high in August with over 386,000 mental health referrals, 34% more than before the pandemic.
- There were 1.76 million people in contact with mental health services, a similar number to last month. However, this is up by 8% compared to a year ago and up considerably by 28% compared to August 2019.
- In August 2023, there were over 386,000 mental health referrals, a figure down by 8% compared from the previous month but up by 4% compared to a year ago, and 34% above pre-pandemic levels.
- There were 1.97m care contacts attended in the latest month, a similar figure to last month but 19% higher than pre-pandemic levels.
- There were 146,659 referrals to NHS talking therapies in August 2023, a decrease of 2% compared to the previous month. Compared to a year ago, referrals are up slightly by 1% and up by 12.3% compared to August 2019.
- In August 2023, there were 845 out of area placements (OAPs), same figure as the previous month and the highest number of OAPs observed since March 2019.
- New urgent referrals of adults to crisis teams have fallen to 30,783 (-2%) since last month but remain considerably higher than last year (+78%).
- Children and young people's urgent referrals to crisis teams also fell this month, to 2,080, but remain considerably higher than last year (+67%).
Our view
Today's figures once again reflect the incredible efforts of staff working under relentless pressure. The NHS faced an increase in demand for urgent and emergency care; this was the busiest October yet for A&E departments, with over 2.2 million people seeking emergency care. The rise in category 1 incidents – the most serious 999 calls – emphasises the strain on emergency services, and another worrying aspect was the deterioration in response times, with those for category 2 incidents reaching the highest recorded this year.
September saw some slight decreases in activity across cancer and diagnostics, although both remain above pre-pandemic levels. There were also small dips in elective care activity, contributing to the waiting list reaching a new all-time high of 7.77m. This is a pressing concern, given the number of patients waiting for necessary surgeries and treatments. However, it is important to note that the number of those waiting more than 52- and 104- weeks has decreased, showing a positive trend in reducing long waits.
A concerning trend is the delay in discharging patients who no longer meet the criteria to stay in hospital. In October, once again more than half of these patients remained in hospital, as this ongoing challenge continues to affect patient flow.
Although urgent referrals to mental health services have fallen in August, they remain considerably higher than in the same month last year.
Trust leaders also face added pressures from months of industrial action and lack of extra government funding to cover the cost of strikes as they approach what will undoubtedly be a tough winter. As always, NHS Providers will be tracking and commentating on the weekly winter sitrep data from the beginning of December in our Winter Watch series as trusts navigate this challenging period.
Frimley Health trials AI in chest scans to speed up cancer diagnoses
Neil Dardis, chief executive at Frimley Health NHS Foundation Trust (Frimley Health) shares how artificial intelligence is being trialled to give patients faster cancer diagnosis.
Frimley Health is leading a trial of artificial intelligence (AI) in radiology to help cancer patients be treated more quickly. The AI technology was introduced earlier this year to test its ability to scan thousands of breast and chest images and prioritise those that detect cancer and suspected abnormalities.
The initial results have confirmed the potential of using AI for early detection and treatment of lung cancer with 99.7% accuracy in triaging scans as normal. It also identified all cancer cases – even the inconspicuous cancer risk nodules that may have remained unnoticed.
The technology, developed by Qure.ai, highlights abnormal scans so radiologists can focus on reporting the urgent cases first, giving patients a faster diagnosis and quicker access to treatment. The technology also demonstrated the potential to reduce consultant radiologists' workload by up to 58%. This could save radiologists up to two hours per day, freeing up time to concentrate on specialist and complex imaging reports.
Consultant radiologist Dr Amrita Kumar, who is leading the trial at Frimley Health, was named 2022 Top 50 Influential women in AI for leading innovation in the use of AI within the NHS.
Dr Kumar said: "This is a very exciting time for the future of AI Technology within the NHS, and we are delighted to be leading the implementation with this important six-month study. AI has a huge potential impact for assisting clinicians and radiologists with triaging and prioritising urgent findings, speeding up the cancer diagnosis pathway, and improving the patient journey."
Darren Stephens, senior vice president and commercial head UK and Europe of Qure.ai comments: "The looming radiologist shortage, now estimated by Royal College of Radiologists (RCR) to be 40% by 2027, underscores the importance of healthcare AI to help bridge the human resource gap and ensure the delivery of the highest standard of patient care into the future. The study at Frimley Health is testimony to the clinical leadership at the trust in embracing AI as an opportunity for positive change."
Background to the study
Encompassing three hospitals – Wexham Park, Heatherwood, and Frimley Park – Frimley Health provides medical services to approximately 1.3 million individuals. On average, they handle about 140 chest X-ray (CXR) requests daily from GPs and outpatient clinics. Despite focusing on timely radiology reporting and maintaining a very high efficiency and turnaround time overall, Frimley Health recognised the potential benefits of AI, establishing a formal AI working group to bolster workflow productivity and aid clinicians in delivering superior patient care.
The looming radiologist shortage in the NHS workforce, projected to reach up to 44% by 2025 (RCR, 2021), underscores the importance of innovative AI solutions. The integration of Qure's AI application, aimed at streamlining normal CXR sorting, may augment overall reporting efficiency. This advancement can enable specialists to concentrate more on intricate cases, such as lung cancer. Therefore, this study highlights AI's pivotal role in optimising radiology department workflows, boosting efficiency, and enhancing patient outcomes.
The solution
The innovative AI solution, qXR, developed by Qure, assists radiologists in deciphering chest X-ray images. This CE Class IIb MDR cleared solution effectively differentiates between normal and abnormal scans, enabling priority assignment to abnormal cases, thereby lightening the consultant radiologists' burden. Moreover, qXR can detect subtle findings such as lung nodules that are suggestive of lung cancer, as well as indications of heart failure that might be overlooked.
A&E
Cancer
RTT
Diagnostics

Ambulance
Mental health