Introduction
Today, NHS England has published the latest figures for performance and activity. These statistics, as always, offer valuable insight into the pressures facing the provider sector. They are particularly important now to understand how the NHS is coping as it emerges from a remarkably difficult winter, navigating a turbulent period of workforce challenges, such as high staff vacancies, staff absences and ongoing industrial action.
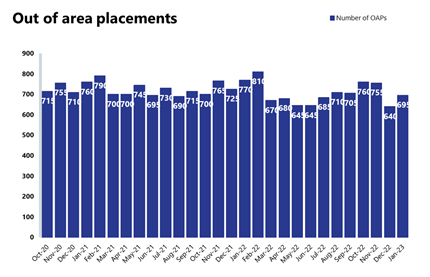
This publication highlights some of the areas of improvement and persistent problems, for example the challenges across urgent and emergency care, as well as the enduring issues with patient flow across the entire system, with mental health and community services under strain.
This month's performance figures
Each month, we look at activity and performance statistics across a range of services including urgent and emergency care, routine care, cancer, mental health and community services. Below we set out the latest trend for each clinical area.
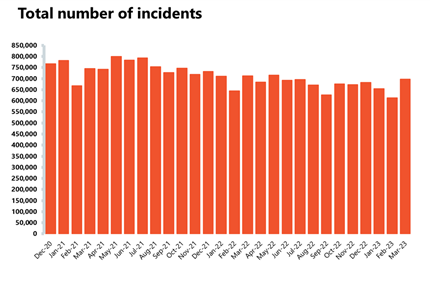
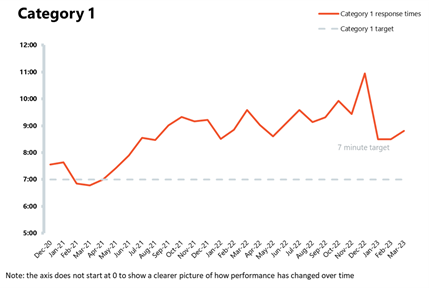
Ambulance: March saw an increase in both category 1 and 2 incidents; the average response times for calls deteriorated and are still missing the targets.
- Category 1 incidents increased by 16% to nearly 77,000, 6% fewer incidents compared to a year ago but 29% higher than before the pandemic in March 2019. Category 2 incidents have also increased by 15%, but there were 3% fewer incidents compared to four years ago, before the pandemic.
- The average response time for category 1 calls increased to 8 minutes 49 seconds from last month, missing the 7 minute target. The average response time for category 2 calls also increased to 39 minutes 33 seconds, missing the 30 minutes target (32 mins 20 secs last month).
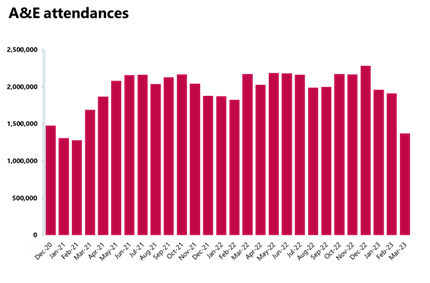
Emergency care activity: A smaller number of A&E attendances were registered in March, but more emergency admissions were observed and targets were missed again.
- There were 1.37 million A&E attendances, a smaller number compared to the one observed the month before (1.19, -28%). There were about 37% fewer attendances compared to one year ago and 10% fewer than three years ago before the pandemic. March saw 532,031 emergency admissions, a 12% increase on the previous month, an increase of 3% compared to a year ago, and up by 24% from three years ago before the pandemic.
- Performance against the 95% target for all A&E types remained the same at 71.5%, whereas the performance against the type 1 target remained steady at 56.8% this month.
- The number of patients waiting more than 12 hours from the decision to admit to admission has increased by 13% compared to the month before, reaching nearly 40,000 in March. This figure is 3,250% higher than the same month three years ago.
- New data from February showed that of the 1.19 million A&E attendances, 11% of people (125,505) waited more than 12 hours in A&E from arrival.
Elective care: Activity has decreased across the board in February, with the waiting list remaining high and stable, but the number of those waiting more than 78 weeks has decreased this month.
- The number of admitted inpatient pathways and non-admitted pathways have decreased by 2% and 6%, respectively, on the previous month. The number of new RTT pathways also decreased on the previous month from 1.7 million to 1.6 million.
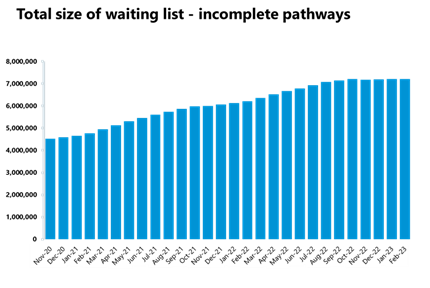
- The size of the waiting list remained somewhat stable (+0.1%) but very high at 7.22 million, now about 58% greater than three years ago just before the pandemic.
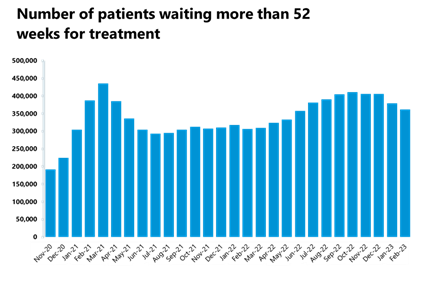
- The number of those waiting more than 18 weeks has also remained somewhat stable compared to the previous month (-0.4%), the number of those waiting more than 52 weeks has decreased (-4%), as well as the number of those waiting more than 104 weeks (-7%). The number of those waiting more than 78 weeks has decreased this month and this figure is now at just under 30,000.
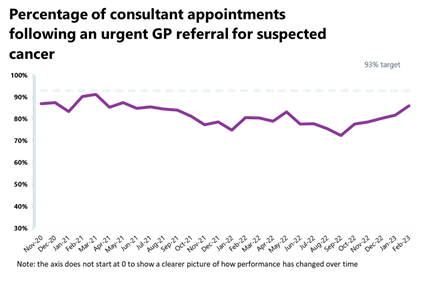
Cancer: Activity remains above pre-pandemic levels for all pathways in February and performance against the waiting time standard has improved across all pathways.
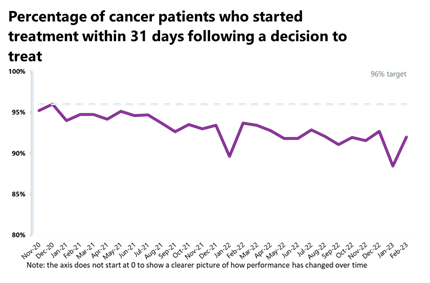
- Although the increase from the month before was very small (+0.7%), activity for the two-week pathway is above levels seen one year ago (+4%) and also above pre-pandemic levels (+21%). Over 25,000 patients completed the 31-day pathway, which aims to begin treatment within one month from the decision to treat, down by 8% from the month before but higher than it was one year ago (+3%) and also above pre-pandemic levels (+5%).
- Despite the 9% drop from the month before, activity for the 62-day pathway is higher (+5%) than it was one year ago, and also above pre-pandemic levels (+10%). Nearly 230,000 patients completed the 28-day faster diagnosis pathway, which aims to diagnose or rule out cancer within 28 days of an urgent GP referral for a suspected cancer, down by 3% from the month before, but up by 5% since last year.
- Performance against the waiting time standard has improved across all pathways and the NHS has met the 28-day faster diagnosis standard for the first time (75%). However, all other key national targets have still not been met: 86% of urgent GP referrals were seen within two weeks, missing the 93% standard; 92% of people started treatment within one month of the decision to treat, missing the 96% target; 58% of people who started treatment did so within two months of an urgent GP referral, falling short of the 85% target.
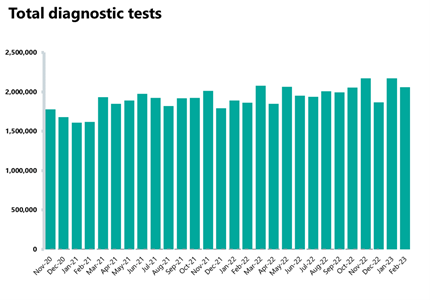
Diagnostics: Highest February on record for diagnostic activity, but the waiting list remains high and climbing.
- In February 2023, there were 2.1 million diagnostic tests carried out, a decrease of 5% from the month before, but representing the highest February on record, with 11% more tests carried out compared to a year ago and ensuring diagnostic activity is also above pre-pandemic levels.
- The number of MRI, CT scans, and colonoscopies have all decreased compared to last month, down by 3%, 6%, and 3% respectively, but activity remains higher than the same time last year and above pre-pandemic levels.
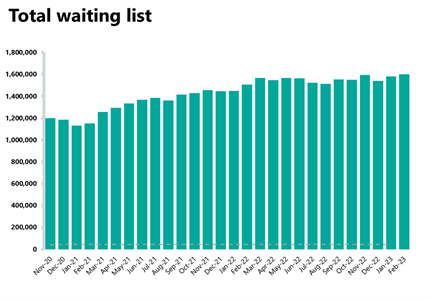
- The diagnostic waiting list remains high at 1.6 million, a 1% increase from the month before but nearly 50% bigger than before the pandemic. A quarter (25%) of patients are waiting six weeks or more for a test, an improvement since the month before (31%) but still missing the 1% target.
Discharge delays
- In the latest month, there were an average of 23,112 patients who no longer met the criteria to reside. Of these, an average of 13,304 (57.6%) patients remained in hospital. This is a smaller proportion than last month (58.5%), although remains high.
- For patients with a length of stay of 21+ days, there was an average of 109,722 additional days in total where patients have remained in hospital since the criteria to be discharged decision was made.
Community services
- As of February 2023, 81% of urgent community response referrals met the two-hour standard for delivering urgent community response services.
- The total reported community health services waiting list was 897,263 in February, 4% higher than the previous month but 1.5% lower than October 2022, when the data collection started. 684,053 of these relate to adult services (up by 5% since January), and 213,210 of these relate to children and young people services (-0.4% since January).
- For adult services, over 100,000 people have been waiting 18-52 weeks for treatment, accounting for 15% of the total adult waiting list. There are 11,568 people who have been waiting for over 52 weeks, accounting for roughly 2% of the adult waiting list. For children and young people's services, over 62,000 have been waiting 18-52 weeks, making up nearly 30% of the total children and young people's waiting list, whereas 12,060 have been waiting over 52 weeks.
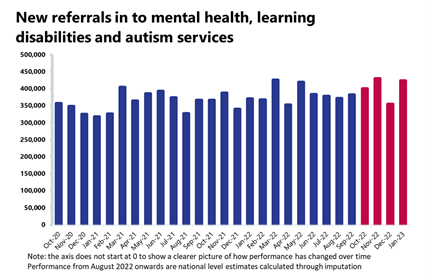
Mental health: Performance from August 2022 to January 2023 was calculated through estimation techniques, so caution should be used when interpreting these statistics.
- January saw an increase of nearly 20% in mental health referrals, a figure also up by 14% and 20% compared to one and three years ago, respectively. Open referrals for adults and for children and young people both fell (by 2% and 6%, respectively) but are higher than pre-pandemic levels, particularly those of children and young people (+71%).
- There were 1.7 million people in contact with mental health services, a decrease of 3% since last month, but up by 11% and 22% compared to one and three years ago, respectively. There were 2.1 million care contacts attended in the latest month, an increase of 16% from the previous month, but also higher than one year ago (+5%) and pre-pandemic times (+8%).
- Although referrals to IAPT talking therapies are somewhat similar to pre-pandemic levels (+0.3%), January saw an increase of nearly 50% since the month before.
Our view
Following what many called the worst winter on record, the NHS endeavours to meet key milestones on a very ambitious catch up plan, while juggling high demand for care and workforce challenges.
Today's figures continue to reflect these relentless pressures, with huge demand seen in the high numbers of A&E admissions and ambulance incidents this month, for example. The picture for urgent and emergency care shows system-wide flow problems, as we see nearly 11% of patients waiting over 12 hours in A&E from arrival in February, as well as nearly 40,000 patients waiting 12 hours from the decision to admit to admission in March.
We welcome the publication of the additional metric, time in A&E from arrival. This new measure complements the four-hour waiting time standard and will be a key measure in tracking progress against the two-year urgent and emergency care recovery plan. It will also help identify systems that need additional support from NHS England to improve patient flow.
In addition to urgent and emergency care, pressures are also being felt in other clinical areas. In January, mental health referrals increased by one fifth, and referrals to IAPT talking therapies were up by 50%. In the community sector, waiting lists keep growing too. This is very concerning and highlights demand-driven pressures on trusts across the whole NHS.
However, despite ongoing strain on an exhausted workforce, sustained industrial action, and a high number of vacancies, trust leaders and their staff have achieved remarkable recovery gains. The NHS has met the 28-day faster cancer diagnosis target for the first time, the number of people waiting longest for elective treatment was brought down, diagnostic activity registered the highest February figure ever, and just over eight in 10 urgent community response referrals met the two-hour standard for delivering urgent community response services.
As trust leaders strive to meet key recovery targets they continue to wait for a long-term fully funded workforce plan to address some of these challenges. It remains a concern that the ongoing strikes will only exacerbate the issues we are seeing in today's data. With some of the worst seasonal pressures now over, today's data is a stark reminder that health services remain under significant strain all year round.
Reducing ambulance wait times at Leicester Royal Infirmary
Jon Melbourne, chief operating officer at University Hospitals of Leicester NHS Trust (University Hospitals Leicester) discusses how the trust is tackling ambulance wait times at their single-site A&E, one of the busiest emergency departments in Europe.
One of our longest-standing challenges has been the ability to release ambulance crews quickly when our emergency department is full. We regularly held ambulances longer than the majority of other NHS trusts, impacting both patients and colleagues.
Ahead of Winter 2022-23, we knew that improvement would not be realised through one intervention alone; so, with the support and feedback of teams across University Hospitals Leicester and partners across our integrated care system and beyond, we embarked on a clinically-led improvement programme. Our actions focussed on improving processes and increasing capacity in areas that would enable us to get patients to the right place for their care as quickly as possible.
We opened a care home and a reablement centre, expanded our on-site same day emergency care services, opened virtual wards in over 10 specialities, moved services into the community and improved our discharge policies to enable us to actively manage flow in and out of our hospitals. This was only possible with the support of colleagues at East Midlands Ambulance Service, Leicestershire Partnership NHS Trust, primary care, local authority and our integrated care board partners.
Alongside these interventions, two particularly impactful improvements helped to drive a real change in our ambulance handover position.
The 'pre-transfer unit'
We opened a new 12-bed unit directly outside the emergency department at Leicester Royal Infirmary for patients awaiting transfer to a ward at one of our sites or another hospital. When a patient enters the care of the pre-transfer unit team, it enables the emergency department to accommodate another patient who requires a bed.
The 'escalation facility'
A dedicated medical unit (also outside our emergency department) allowed us to take patients from ambulances at times of significant pressure, giving us the ability to manage variation in patient flow across the day.
Some of the changes have been difficult and they have not always been universally popular, but from January to March, we have sustained significant improvements in our ambulance handover times. Some weeks, wait times have been up to 95% lower than seen in December 2022, allowing East Midlands Ambulance Service to respond much faster to emergency calls.
The teams across University Hospitals Leicester and Leicester, Leicestershire and Rutland have much to be proud of in what they have achieved and continue to achieve every day. We are grateful for the understanding of all colleagues, in particular the teams who work in our adult and paediatric emergency departments.
We have much more to do to sustain the response times that our communities expect of us and to further improve on all our access standards. We are committed to that journey.
This week, we communicated our urgent and emergency care plans for 2023/24 to colleagues across University Hospitals Leicester, seven months earlier than last year. The scale of the challenge we face remains significant, but we are also excited about being able to deliver better care for patients and a better working experience for our colleagues.
A&E

Cancer
RTT
Diagnostics
Ambulance
Mental health