Introduction
Today, NHS England publishes a range of activity and performance data across physical and mental health services. Below we detail the trends across specific services. Today also marks the first in five days of strikes by junior doctors.
This month's data highlights that despite crucial activity gains across many areas, demand continues to outstrip supply across services, resulting in bigger waiting lists. Furthermore, the NHS remains under relentless pressure as industrial action continues to add to an already challenging operational context
This month's performance figures
Each month, we look at activity and performance statistics across a range of services including urgent and emergency care, routine care, cancer, mental health and community services. Below we set out the latest trend for each clinical area.
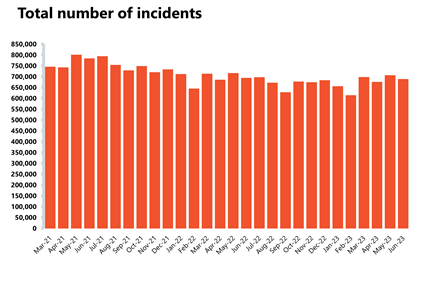
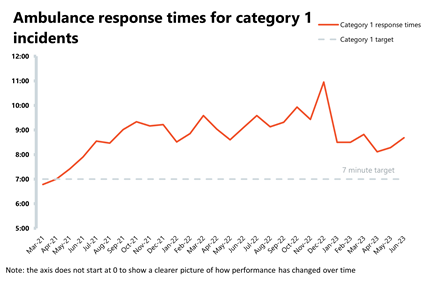
Ambulance: June saw increases in category 1 incidents, with average response times also increasing and targets for both category 1 and 2 being missed.
- Ambulance category 1 incidents increased by 1% to 77,063 (906 more incidents). There are 3% fewer incidents compared to a year ago but incidents are a third (33%) higher than four years ago, before the pandemic (April 2019). Ambulance category 2 incidents decrease by 2% in June to 367,670 (8,622 fewer incidents). Compared to four years ago, category 2 incidents are down by 2.5%.
- The average response time across England for category 1 calls increased by 24 seconds to 8 minutes 41 seconds, missing the 7-minute target. The average response time for category 2 calls also increased by 4 minutes and 25 seconds, reaching 36 minutes 49 seconds, missing the 30 minutes target.
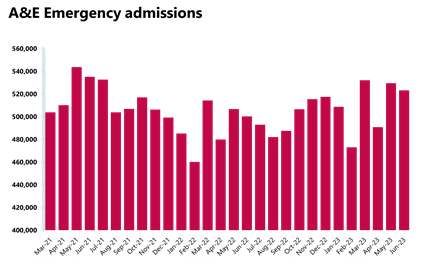
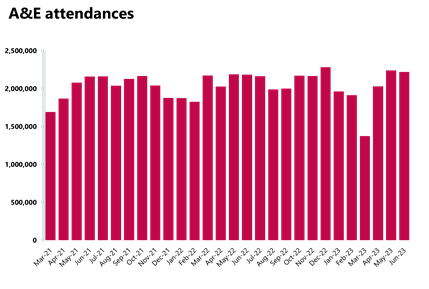
Emergency care activity: Busy June with over 2.2 million A&E attendances, and the number of patients waiting more than 12h from the decision to admit remaining high, despite a 6% drop from the month before.
- There were 2,220,954 A&E attendances, a slightly smaller number compared to the month before (-1%). There were 523,231 emergency admissions in June, also a 1% decrease on the previous month. However, this figure is 5% higher than last year (June 2022).
- Performance against the 95% target for all A&E types slightly decreased and it's now 73.3%. The performance against the type 1 target slightly decreased to 60.2% this month from 60.4%, remaining above 60% for the third consecutive month.
- The number of patients waiting more than 12 hours from the decision to admit to admission has decreased by 6% to 26,531 since the month before. This figure is still over 5,500% higher than the same month four years ago before the pandemic (June 2019), when this number was 471.
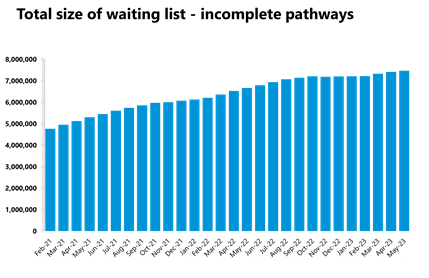
Elective care: Activity has increased across the board in May, but the waiting list increased again and it's now at an all-time high of 7.47 million showing demand still outstripping supply.
- The number of admitted inpatient pathways and non-admitted pathways increased by 18% and 20%, respectively. The number of new RTT pathways in May also increased on the previous month from 1.5m to 1.7m.
- The size of the waiting list slightly increased by nearly 1% and is now at 7,472,052 (7.47 million, 56,700 more people than on the previous month). The size of the waiting list is still 65% greater than four years ago before the pandemic.
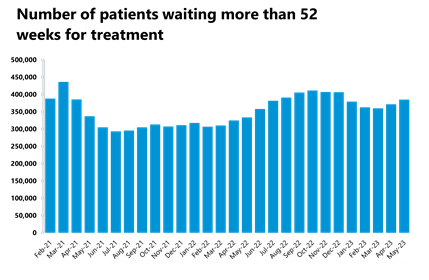
- The number of those waiting more than 18 weeks has decreased compared to the previous month (-2%). Conversely, the number of those waiting more than 52 weeks increased and is now at 385,022 (+4%).
- The number of patients waiting more than 78 weeks decreased by 31, and this figure is now at 11,446. However, this still represents a decrease of 91% since its peak in September 2021 (124,911) and a decrease of four fifths since the start of 2023 (54,882 in December 2022).
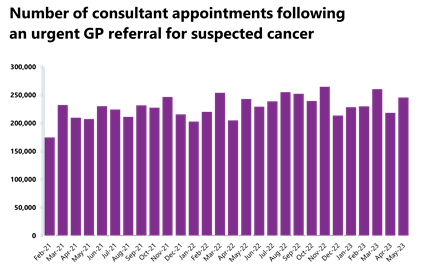
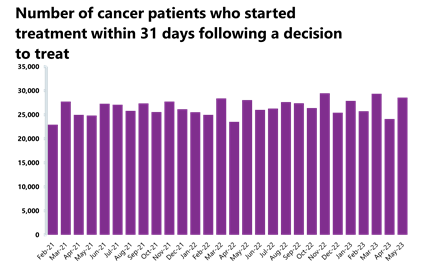
Cancer: Increases in activity across all pathways, with all figures above pre-pandemic levels, but performance is still falling short against the waiting time standards.
- Nearly 250,00 patients were seen within two weeks of an urgent referral for a suspected cancer pathway, a figure up by 13% from April and above levels seen one year (+1%) and four years ago (+23%) before the pandemic. Over 28,500 patients (+18%) completed the 31-day pathway, which aims to begin treatment within one month from the decision to treat, a figure now above pre-pandemic levels (+11.5%)
- Over 15,500 patients completed the 62-day pathway (+17%), which aims to start a first cancer treatment within 62 days from an urgent GP referral. Activity for this pathway is slightly higher than it was this time last year (+1%) and above pre-pandemic levels (+15%).
- Performance against the waiting time standard was not met this month – it deteriorated for the 31 and 62 day pathways, remained the same for the 28 day pathway, but improved for the two week pathway.
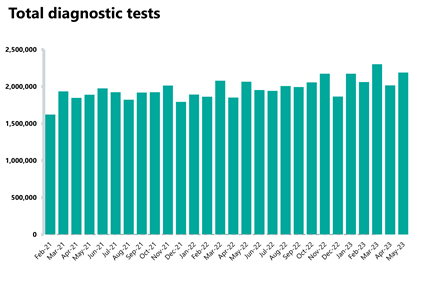
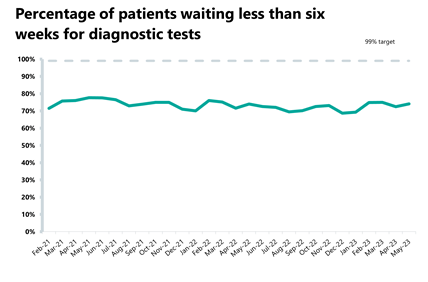
Diagnostics: Over two million diagnostic tests were carried out in May, an increase from the month before and above pre-pandemic levels, however, the diagnostic waiting list has slightly increased to over 1.58m showing persistent demand.
- 2.19 million diagnostic tests were carried out, an increase of 8.5% from the month before. Activity for the latest month is 6% higher than one year ago (122,143 more tests) and is 10% higher than pre-pandemic levels, with 191,568 more tests carried out compared to May 2019.
- The number of MRI, CT scans and colonoscopies all increased compared to last month, up by 4%, 7% and 11% respectively. Activity for these is also above pre-pandemic levels, up by 15%, 26% and 23% respectively.
- After a decrease last month, the diagnostic waiting list increased by 1% this month to 1,583,543. This is also 1% higher than May last year. Compared to May 2019 before the pandemic, the waiting list has grown by 49%.
- The number of patients waiting six weeks or more for a test is at 25.9%; this is down slightly from the month before (27.6%) and is still missing the 1% target.
Hospital capacity and discharge delays: Bed occupancy high at 92.8% and over half of patients who no longer meet the criteria to reside have remained in hospital.
In June 2023, there were 99,910 G&A (general and acute) beds available. This is 0.2% fewer beds available compared to the previous month (177 fewer). Of these, 92.8% were occupied, down from 93.2% last month. Compared to last year, the number of G&A beds available has increased by 1.9%.
- On 30 June (a Friday), there were 24,733 patients who no longer met the criteria to reside in hospital. Of these, half (50%) remained in hospital on that day. For the month of June, there were an average of 22,522 patients who no longer met the criteria to reside. Of these, an average of 12,334 (54.8%) patients remained in hospital. This is lower than the previous month (56.5%).
Community services: Urgent community response teams are meeting their national target, but waiting lists continue to grow.
- As of May 2023, 83% of urgent community response referrals met the two-hour standard for delivery. This is down from 84% in April.
- In May 2023, the total reported waiting list in England was 970,540. This is 3% higher than the previous month and 7% higher than October 2022, when the data collection started. 744,848 of these relate to adult services, an increase of 4% since the previous month and 6% higher than October 2022. 225,692 of these relate to CYP services, a similar number (+0.2%) to the previous month and 9% higher than October 2022.
- For adult services, 99,629 people have been waiting 18-52 weeks for treatment, a decrease of 1% since last month. There were 12,826 adults waiting over 52 weeks, an increase of 5% since last month. For children and young people (CYP) services, 66,941 were waiting 18-52 weeks, a fall of 3% since April. There were 15,798 CYP who were waiting over 52 weeks, an increase of 7% since last month.
Mental health: Caution should be taken when interpreting these figures due to the recent cyber incident. However, impact on the following data is understood to be limited.
- In April 2023, there were 369,056 mental health referrals. This is down by 21% compared to the previous month, up by 5% compared to a year ago and up 22% compared to before the pandemic.
- There were 1,404,106 adult open referrals in April 2023, up by 6% compared to last year and 4% compared to pre-pandemic levels. For children and young people, open referrals were at 465,583, a decrease of 5% compared to the previous month but still considerably higher than pre-pandemic levels (+77%).
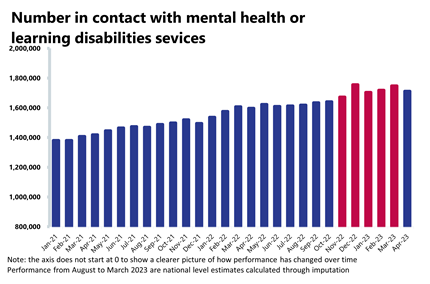
- There were 1,711,569 people in contact with mental health services, a decrease of 2% since last month but up by 27% compared to April 2019. There were 1.8 million care contacts attended in the latest month, a decrease of 19% compared to the previous month, but up by 8% compared to before the pandemic.
- There were 129,753 referrals to talking therapies (IAPT) in April 2023, down by 22% compared to the previous month and down by 3% compared to April 2019 before the pandemic.
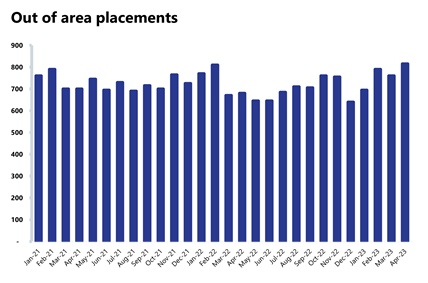
- There were 815 out of area placements, an increase of 7% since last month (55 more OAPs). Compared to a year ago, OAPs are up by 20% (135 more). Compared to pre-pandemic levels, OAPs are up by 1% (10 more).
- In April 2023, 90% of people who had been referred finished a course of treatment in the month, accessed IAPT within 6 weeks, a similar figure to March (90.2%).
Our view
Today's figures show the sustained pressures felt across the NHS, including in emergency care, hospitals, the community and mental health settings.
As the NHS implements the national plan to recover urgent and emergency care services, the demand for emergency care remains extremely high, with data from June showing more A&E attendances than the same time last year, as well an increase in average ambulance waiting times. Inside hospitals, bed occupancy was at an average of 92.8% over June.
Last month in our Activity Tracker, it was evident that activity across many acute pathways dipped. However, this month's figures show that the number of operations, diagnostic tests, suspected cancer referrals and those starting cancer treatment have all increased. Despite this bounce back in activity levels, which exceed the activity of the previous month, the same month last year and before the pandemic across most metrics, the elective care and diagnostic waiting lists have continued to grow in size. Even though frontline staff are doing and delivering more, the demand for services this month has outstripped the faster pace at which the NHS is running.
Outside hospitals, urgent community response teams are meeting their national target. However, the new community waiting list data shows further growth in the backlog.
For mental health services the data published today, relating to April, indicates a reduction in referrals and care contacts. These dips in activity mirror the trends observed in the April data for elective, diagnostic and cancer services, which we highlighted last month.
Continued and sustained industrial action is having an impact on services and on what staff can deliver, right across the NHS. However, the data published today shows that despite the hot weather, bank holidays and strike action in May, NHS staff managed to recover activity levels across many services, helping to retain access to planned care.
Industrial action and severe workforce shortages are making the NHS recovery journey more challenging. Trust leaders know that many people are still waiting to access treatment far longer than is comfortable. Nevertheless, it is important to view these activity gains as small successes along the way. This is testament to the commitment and hard work of staff who are working in a very difficult operational context.
Secondary care must support prevention to help sustain services and resilience
Dr Christopher Odedun, consultant in emergency medicine at Newham Hospital, discusses how the support from secondary care can help sustain services.
Working at a busy hospital in a vulnerable and deprived area of East London focuses the mind on how we can sustain our services for the future.
Something has become more and more apparent to me in these pandemic-influenced times, since I completed training and started a consultant career: if we don't tackle the root cause of patients' problems now, we will be overwhelmed in the future. We simply cannot do more of the same and need to take a new approach, including in emergency care.
In my opinion, we need to invest more time in taking stock and noticing how we are. For me, this looks like committing effort to identifying our most vulnerable groups and considering how population health initiatives could help. I believe secondary care can advocate for our patients in a different way, one better understood within a vulnerability framework. This could ultimately reduce the size of our future workload, but unless we think longer term, we are unlikely to succeed.
In Newham, the population is socially deprived and home to a community of undocumented migrants, with many facing unstable housing and work, and living in an environment of tangible vulnerability. Infectious diseases, vaccine under-reach, modern slavery, gang violence, substance abuse and decompensated chronic illnesses like chronic obstructive pulmonary disease (COPD) and diabetes are everywhere. These patients often use our emergency department as primary care for many reasons.
It's never been clearer that people need to have the wider determinants of their health addressed alongside their medical issues. A good starting point is addressing equity and health inequalities, and encouraging secondary care clinicians to consider them whenever they can, ideally in every consultation.
The Core20Plus5 initiative led by Dr Bola Olawabi, Director of Health Inequalities at NHS England, has already made strides in focusing minds around particular at-risk groups. Using a population health management approach to deliver more personalised care to individuals in these groups could further improve outcomes.
But what can we do in secondary care? Perhaps the first step for you, the reader, is simply acknowledging and supporting the approach. Who are your most at-risk groups, and what strategies and funds are currently being used to improve their outcome measures, whatever they are?
Data-driven decision making at place and neighbourhood level is leading to a redesign of services through partnerships within integrated care systems, sometimes in the form of provider collaboratives. Emergency care needs to be ‘in the room’ for these discussions. Using analytics and data to identify cohorts of patients with specific risk factors - loneliness/social isolation, frailty, a damp house or musculoskeletal problems - is the beginning. Done correctly, these initiatives will have a direct impact on my day job in emergency care, and that's why we need to support and invest in them to succeed.
The high intensity user model uses this approach to identify and reach out to individuals who need focused, multi-disciplinary help. In the medium term it can reduce use of emergency resources better assigned elsewhere. This has worked well in our area and others, but we need to ensure such services continue and are worked into everyday commissioning, especially when times get tough financially. This is where the weight of support from secondary care can really ensure these programmes thrive.
NHS England recently published its Intelligence Functions Guidance illustrating some of the best ways to set up analytical capability in a system. It can seem a long way away from the hospital, but this structure is where we start as a system in identifying, personalising and preventing.
Working with our voluntary sector colleagues is crucial. Despite the challenges many of my patients face, the community and its leaders can be a huge asset in co-producing, supporting and embedding new approaches.
Music, for example, is a great passion of mine and I'm keen to understand how we can use cultural capital and its inherent ability to connect and inspire people, and impact positively on their health and wellbeing. We're also doing this in-house at Newham Hospital, in a collaboration with the London Symphony Orchestra, who regularly attend the hospital to provide music therapy to patients.
I still have many questions about how we can begin to turn the tide. Integrated care systems can certainly promote the collaboration necessary to improve local relationships. We must maintain this shift away from reactivity if we want to meet the demands of today and tomorrow.
For more information about Population Health Management visit the Population Health Academy on FutureNHS which is free to join
A&E

Cancer
RTT
Diagnostics
Ambulance
Mental health