In recent years, there has been a growth in guidance on the role of the NHS in addressing health inequalities, particularly from NHSE. In our guide for NHS trust board members - Reducing health inequalities – we have collated and summarised the key policy documents relevant to trusts (NHS Providers, 2024a). In our survey, we were keen to determine the extent to which these national policies have filtered down into local priorities for trusts.
Respondents were most likely to say that the Core20PLUS5 for adults was fully embedded or partly applied in their health inequalities work and/or strategy, with 82% of respondents selecting fully embedded (31%) or partly applied (51%) for this policy document. 74% of respondents stated that the Core20PLUS5 for children and young people was embedded. Core20PLUS5 is NHS England's framework for reducing health inequalities (NHS England, 2021b). It encourages NHS trusts and ICSs to prioritise attention on specific patient population groups and clinical areas. Feedback from executive leads suggests that Core20PLUS5 is well known and understood by the majority of trusts - most executive leads referenced that the framework shaped their health inequalities work, which has contributed to trusts taking a condition-specific approach to their work (Figure 4). However, some executive leads we spoke to from specialist providers felt that the five clinical areas were not applicable to them and there were suggestions for future versions of the framework to include rare diseases and other conditions where inequalities are known (such as sickle cell and HIV).
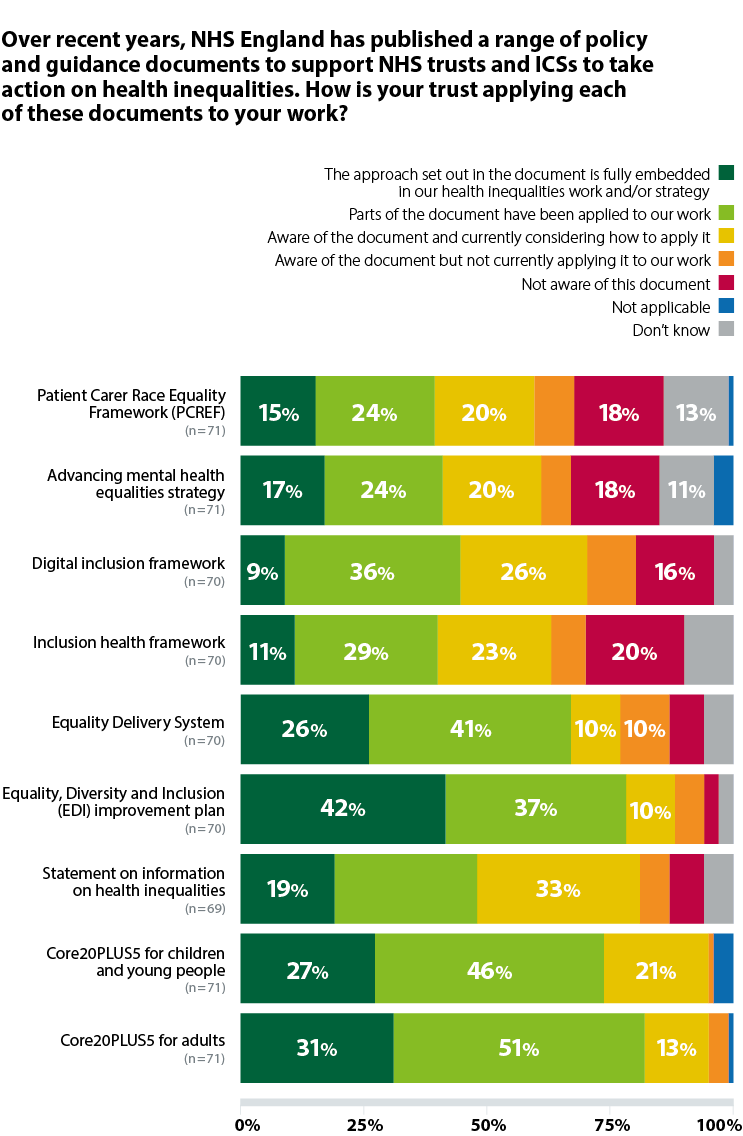
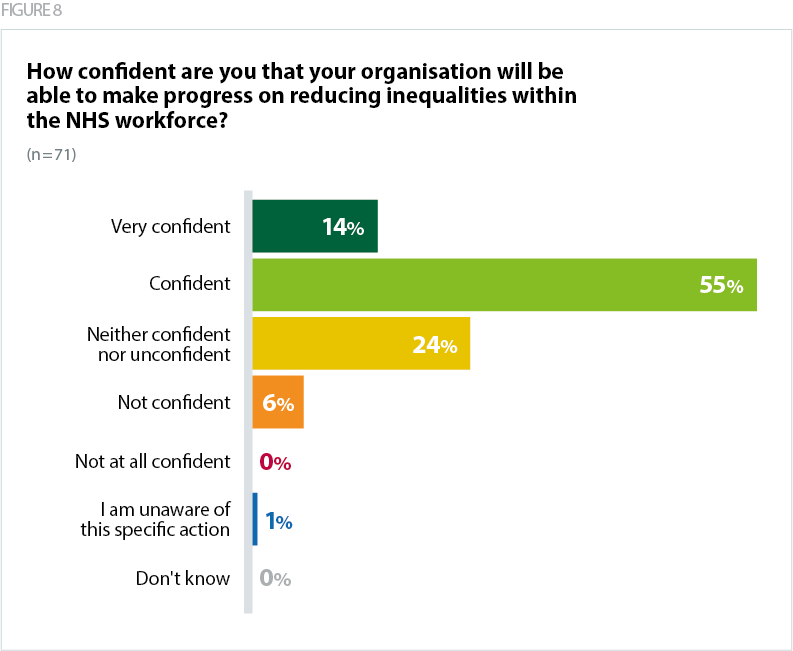
42% of respondents stated that NHSE's equality diversity and inclusion (EDI) improvement plan (NHS England, 2023b) was 'fully embedded in our health inequalities work and/or strategy'. The EDI improvement plan (NHS England, 2023b) sets a specific action for trusts to target inequalities within the workforce by April 2025. There are high levels of confidence among trust leaders that their organisation will be able to make progress on this action – with 14% of respondents very confident and 55% confident they will reduce inequalities within the NHS workforce. Also, an earlier survey question found that 75% of trusts are taking action on 'addressing inequalities within the workforce' (Figure 4). There were a range of approaches trusts are taking in this area - such as offering free Vitamin D supplements or access to smoking cessation services. Others were focused on improving staff wellbeing and mental health.
The least well-known and embedded national policy documents among the survey respondents were the inclusion health framework (20% not aware), the advancing mental health equalities strategy (18% not aware), Patient Carer and Race Equality Framework (PCREF) (18% not aware) and the digital inclusion framework (16% not aware). PCREF, the digital inclusion framework and the inclusion health frameworks were all released in 2023 - it may take time before trusts are fully aware of and embedding these documents within their health inequalities work. Feedback from a small number of executive leads expressed a want and desire to do more work on digital inclusion specifically, identifying it as a current blind spot.
Both PCREF and the advancing mental health equalities strategy are applicable to mental health trusts, which may explain why the broader range of trusts involved in our survey were not aware of these. Looking at the responses from mental health trusts specifically, there are higher levels of awareness of these guidance documents. PCREF is 'fully embedded in our health inequalities work and/or strategy' within 39% of mental health trusts, compared to 15% of all trusts. Similarly, the advancing mental health equalities strategy, is 'fully embedded' in 43% of mental health trusts, compared to 17% of all trusts.
NHSE's statement on information on health inequalities expands on the legal duty on trusts to address health inequalities, by outlining a set of data indicators (broken down by factors such as deprivation and ethnicity) that trusts and systems are expected to monitor and report on annually (NHS England, 2023a). Only 19% of respondents said that is 'fully embedded in our health inequalities work and/or strategy' – however, this is perhaps unsurprising since the statement was published towards the end of last year, leaving little time for review and implementation ahead of the annual reporting process. We welcome the value that the statement provides in standardising the approach for collecting, analysing and publishing information on health inequalities, providing a key set of indicators to measure progress in tackling health inequalities over time (NHS Providers, 2023a).
Trusts highlighted a tension and misalignment between the national guidance on health inequalities and other national policies and targets that prioritise action in other areas and may inadvertently exacerbate inequalities, such as those that prioritise performance and activity, rather than health outcomes and meeting the holistic needs of patients. This includes the inconsistent focus on inclusive recovery, as mentioned, and shortening appointment times. Most trusts want to take a more proactive approach to their inequalities work but are limited in their capacity. Trusts need consistent messages from NHSE, from both national and regional teams on the extent to which they should be prioritising this work. There is also a need for a longer-term approach to operational and financial planning that prioritises health inequalities and prevention.
"Operations team are focused on reducing long waiters and backlogs. To them, addressing health inequalities could feel like an additional thing they need to do when they are struggling with workforce challenge, backlog, etc. The board recognises addressing health inequalities as a priority, but it is not yet as well integrated into existing governance structure and business planning as it could be. Contracts and performance targets measures processes (e.g. number of patients waiting under 52 weeks) rather than health outcomes."
"There is pressure on the delivery of financial balance and national activity targets. This does not always allow for consideration of actions that impact health inequalities in the short term and the medium term."