ICSs have a clear remit in improving outcomes in population health and tackling inequalities in outcomes, experiences, and access. There is a great potential for trusts to collaborate with their system partners to drive forward work on health inequalities. There is a sense from trusts that ICSs could provide an opportunity for providing overall strategic direction, alongside sharing good practice and facilitating collaborative working on joint health inequalities projects. However, rates of development and maturity vary between places, which has impacted on the extent to which ICSs have prioritised or focused on the topic of health inequalities. Trusts also recognised the value of working with other system partners on the health inequalities agenda, such as local authorities and VCSE organisations.
We asked trusts about their involvement in system approaches to reducing health inequalities, with the vast majority (61%) positively selecting that 'our ICS/s have a developed health inequalities plan and we are actively involved in delivering it'. In another survey question (Figure 6), 81% of respondents said that their 'health inequalities work is closely aligned and linked to work on health inequalities at the wider system level (such as ICBs and provider collaboratives)'.
"By aligning goals and priorities across ICS and Place, and across Places, we can achieve maximum impact for the population we serve. Mutual reinforcement of a smaller number of priorities would increase the focus of effort in our partnerships and the chance of improvement at a time when services are under considerable pressure."
"There is a need for system working but it is difficult to work across the system...this is improving but it is slower than we would like."
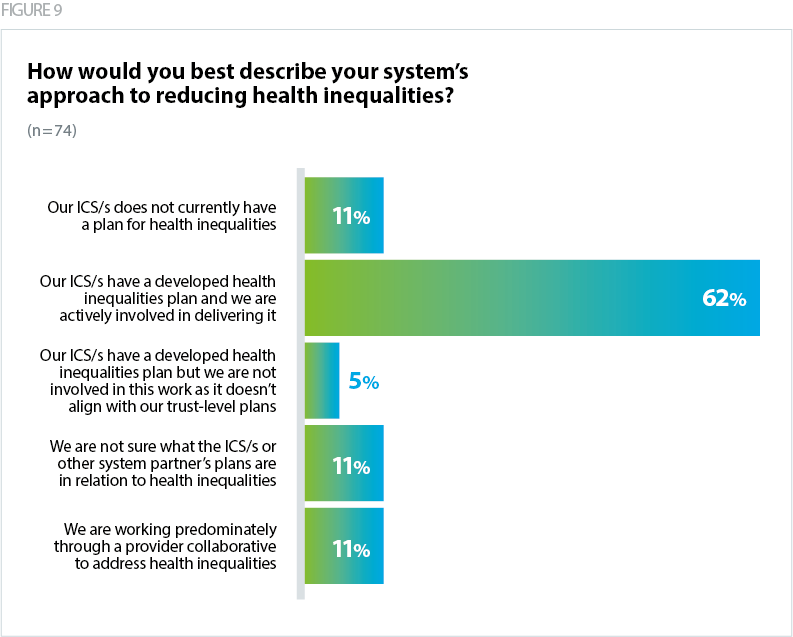
It is welcome to see that 11% of respondents are working through provider collaboratives to deliver their health inequalities work. Elsewhere, we have highlighted the benefits of working in these models around population health – see this case study from the West Yorkshire Mental Health, Learning Disabilities and Autism Collaborative.
However, Figure 9 shows that there are a large number of trusts (27%) that are not engaging with their system on health inequalities work – with 11% of respondents 'not sure what the ICS/s or other system partner's plans are in relation to health inequalities', a further 11% stating that 'our ICS/s does not currently have a plan for health inequalities', and 5% where the ICS has a health inequalities plan but the trust is not involved as it doesn’t align with the trust's plans on health inequalities.
Feedback from our insight calls with executive leads provides a mixed picture on how well system working around health inequalities is going. Levels of maturity have impacted on the speed that ICSs have made progress on addressing health inequalities.
The main concern noted by trusts was around a lack of focus and unclear responsibility and accountability structures at system level. Trusts raised a need to clearly outline who within the system is best placed to lead on different aspects of reducing health inequalities. For some, their ICB had not outlined what the role of providers was and for another the system-focus on health inequalities was aimed solely at primary care. In reality, this lack of join up has led to a sense of confusion, with providers "doing their own thing", resulting in everyone doing different things and having to have repetitive conversations across the system.
"The ICS is developing a strategy for health inequalities - the trust is slightly ahead of this and already has approved strategy and work programme."
"System could better coordinate between different sectors and convene more - has a slightly scatter gun and uncoordinated approach."
Ambulance trusts noted sector specific problems relating to system working. They typically cover a broader geography and so are required to work with multiple ICBs, each of which are likely to be at different stages of development, not in communication with each other and operate with different commissioning and data sharing arrangements.
The requirement for ICBs to develop joined-up action plans to address health inequalities and implement the Core20PLUS5 approach is a welcome opportunity to streamline approaches and take a collaborative approach, with clear expectations for each part of the system (NHS England, 2024).
"Trust has brought together key, partner organisations and fellow anchor institutions … These include public health representatives from the two local authorities; Higher Education Institutes (HEIs) - university and colleges; Healthwatch; Youth Zone; Local Constabulary; Voluntary, Community, Faith and Social Enterprise (VCFSE) sector; local Community Football Trusts amongst others. The group meet every six weeks to table and discuss health equity problems pertinent to the area. It is envisaged that by fostering strong community relationships, a wider health equity lens can be applied to specific projects that originate via the Trust and vice versa."