The survey asked trusts to describe the barriers they face in addressing health inequalities. Figure 2 demonstrates the range of factors that can prevent trusts from taking action. However, if each of these obstacles could be overcome these would be enabling factors for achieving success.
The operational pressures trusts are facing have clearly had a stark impact on the ability of trusts to prioritise health inequalities. Close to three quarters of respondents (73%) selected 'wider system pressures and operational challenges', closely followed by 'lack of operational resource' (55%) and 'financial pressures' (53%). Each of these factors has increased in significance since the same question was asked in 2021. Another major barrier identified by trusts is 'lack of funding for health inequalities initiatives' (51%). This option was added to the survey in 2024 and we do not have comparative data for 2021, but it contributes to the broader picture of over-stretched demands on organisational finances.
"Sheer operational pressures of UEC, recruitment and retention and industrial action (it’s been a killer)."
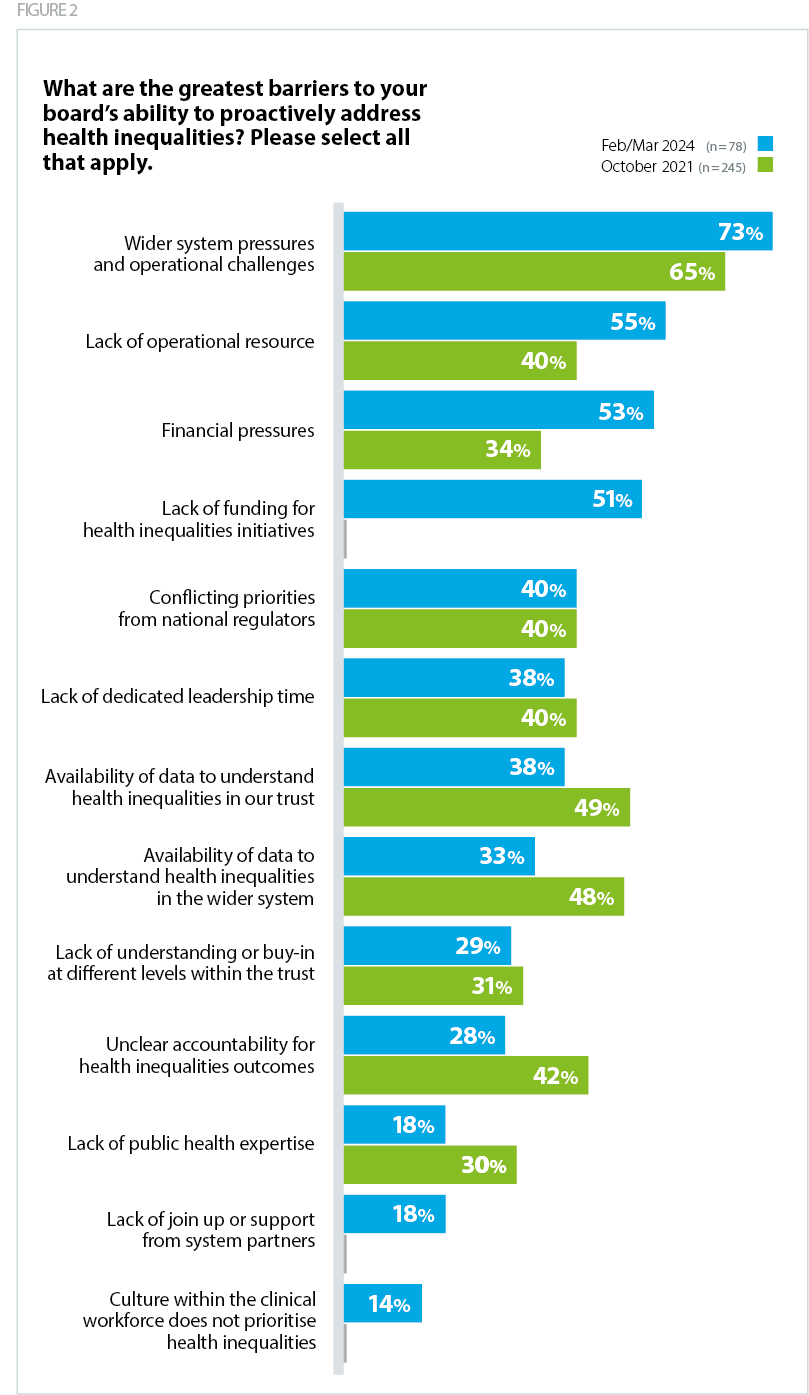
Comparing the responses to this question between 2021 and 2024, we can see that improvements have been made to overcome some of these barriers. Both the availability of data at trust-level and system-level were major barriers for trusts in 2021 (49% and 48%), but these have now fallen and are less of a priority problem in 2024 (38% and 33%). Similarly, 'unclear accountability for health inequalities outcomes' was a barrier for 42% of respondents in 2021 and just 28% in 2024. 'Lack of public health expertise' was a barrier for 30% in 2021 and this has fallen to 18%. These results are heartening and demonstrate progress in key areas, but there remains more to be done to fully overcome these barriers.
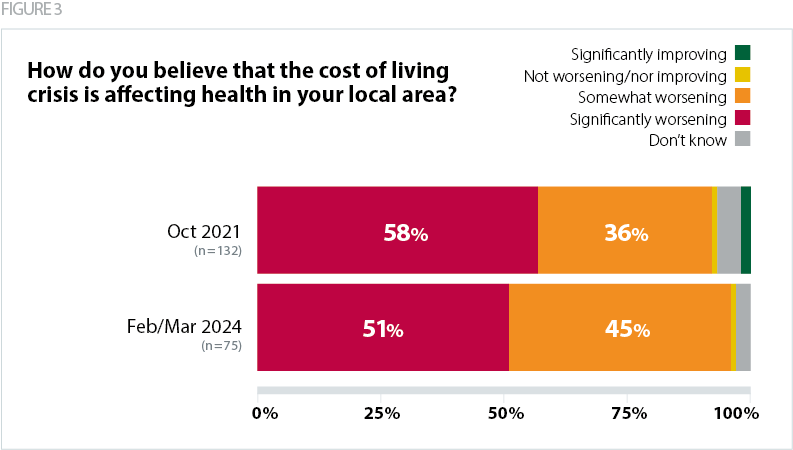
The wider context and external environment have also exacerbated inequalities and impacted on the ability of trusts to effectively mitigate against diverging health outcomes during this period. Survey responses suggest that the knock-on impact of the cost-of-living crisis on health has stayed consistently high over time. In 2024, over half (51%) of respondents said that the cost-of-living crisis was 'significantly worsening' health, in comparison to 58% in 2022. This is directly impacting upon the way in which patients access healthcare services.
"It is disproportionately affecting areas of higher deprivation. … "I can't afford to take time off work to see a doctor" is common. The gap in life expectancy between IMD Quintile 1 and 5 in our main town is widening between areas that are just a mile or two apart."