We have seen many improvements in how trusts are addressing health inequalities, yet there is still much more to be done to shift the dial and see demonstrable progress in improving health outcomes across the population. Operational pressures have intensified in recent years, leaving trusts little headspace or resource to prioritise efforts on actions considered to be not immediate or urgent. But not addressing health inequalities now will increase the burden and pressure on health services later down the line – this is the time to act.
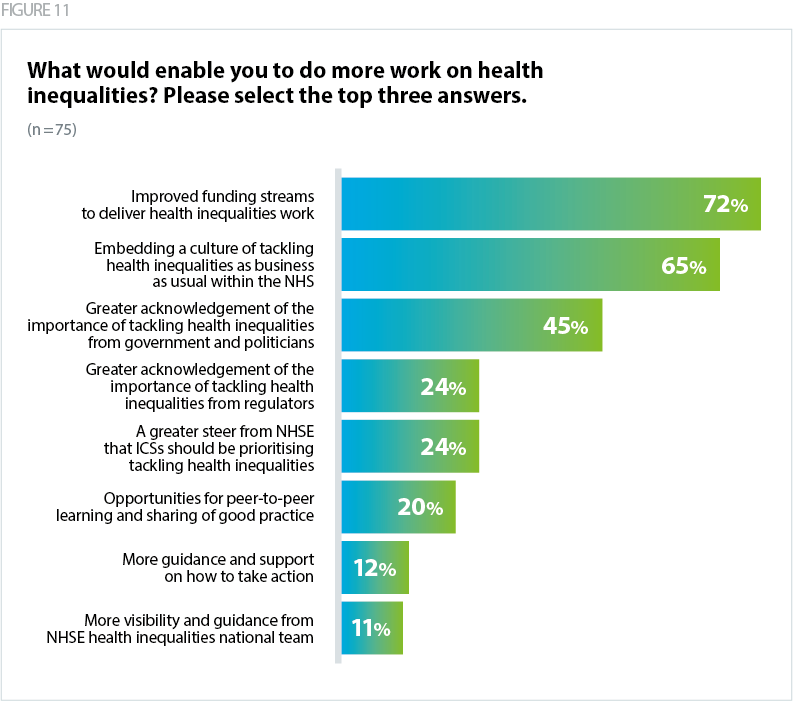
Our research has shown that trusts know and understand the scale of the challenge ahead of them. The evidence-base is clear and the policies that exist provide a roadmap to change. Trusts are not calling for more guidance and support (12%). The overwhelming majority of trusts (72%) say they require 'improved funding streams to deliver health inequalities work'. Without investment and resource, well intentions to reduce inequalities are hampered. Many trusts have requested long-term, ring-fenced funding to deliver on this agenda.
As discussed, clarity is also needed on the different demands placed on trusts from NHSE and national bodies, which don't always prioritise or incentivise action on health inequalities. In fact, sometimes national policies can exacerbate trends in inequalities. There is a desire for improved alignment on policy priorities from the centre and development of a national NHS strategy for tackling health inequalities.
"The culture of the NHS is currently one of reaction; this is not unique to our trust. The national direction from NHSE is clear, but the national imperative from central government contradicts this and therefore NHSE are limited in their ability to mandate this work. The CMO's annual report is helpful, but is advisory at best. Short term performance improvement lays the foundation for long term cultural change, but the long term cultural change has to be an equal priority, not an afterthought."
In order for meaningful change to occur, tackling health inequalities cannot be viewed as one part of the trust's operation. Siloing action may mean that the rest of the activity in the organisation is worsening inequalities elsewhere. Trusts have identified that 'embedding a culture of tackling health inequalities as business as usual within the NHS' is a key enabler to making progress (65%). Our guide for NHS trust board members Reducing health inequalities provides a set of objectives for trust boards to address health inequalities outlining the different responsibilities of each member of the board (NHS Providers, 2024a). Setting a culture of shared responsibility at the top of the organisation could reap benefits across the wider trust.
Executive leads shared with us the challenges of establishing a culture of business as usual in addressing health inequalities. For some, there is a sense that it is viewed as an addition to the day job, with one trust asking "how can you add these responsibilities onto an already exhausted workforce?". Trusts may look to provide training for different staff groups to better understand the role they can play in tackling disparities.
"Capacity - it is still seen as a nice to do which is cultural but when facing extreme system pressures this is one of the first areas to be paused."
The NHS cannot tackle health inequalities alone. Shifting the dial requires action across all sectors that impact on the wider determinants of health – housing, education, local authorities, and the private sector. Spending power in local authorities has fallen by 26% between 2010/11 and 2020/21 (National Audit Office, 2021). The public health grant – which provides resource for delivering preventative services, such as weight management and smoking cessation – has been cut by 28% on a real-terms per-person basis since 2015/16, and the largest cuts have been seen in the most deprived areas of the country (Finch, 2024). Trusts in our research have called for greater investment in upstream services that will prevent inequalities and reduce the burden on the NHS, including investment in local government functions.
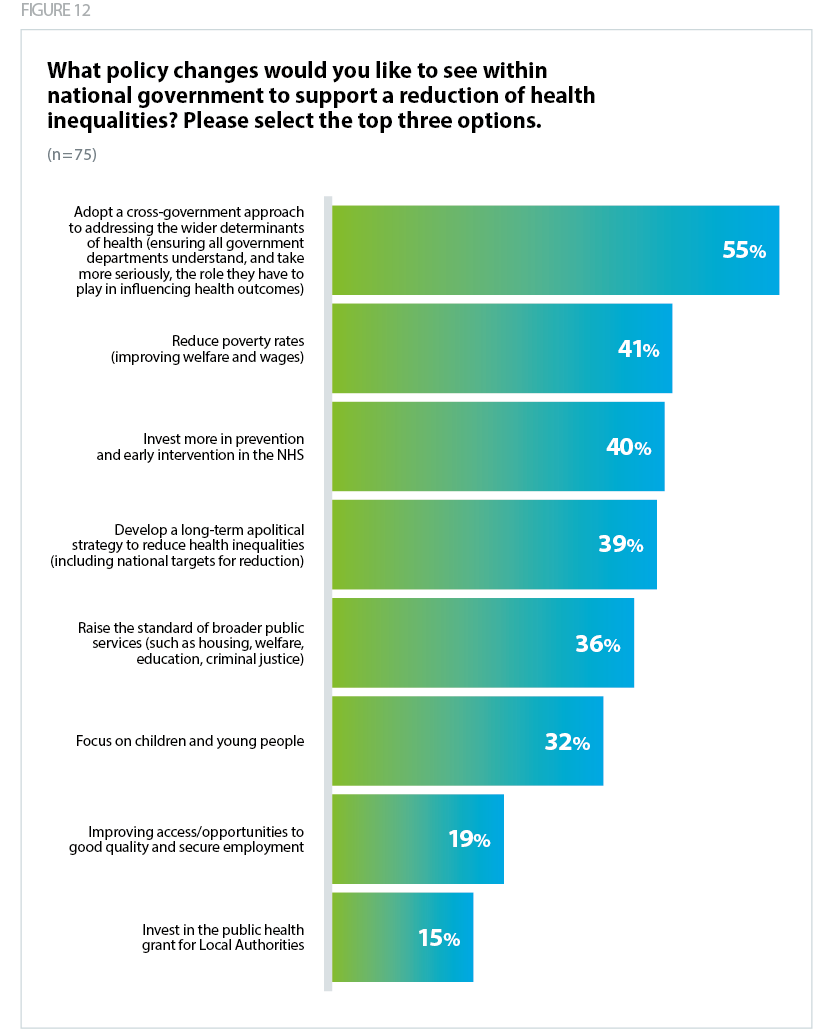
As we are approaching a general election we have outlined shared commitments for working with government to deliver the next generation NHS and create a picture of health that is responsive, effective and continuously improving (NHS Providers, 2024c). We are calling for collaborative action to address the wider determinants of health, including implementation of a whole-government health and care strategy which looks across the needs of the whole population, now and over the decades to come. Our survey respondents agree, when asked what changes they would like to see within national government, over half (55%) said 'adopt a cross-government approach to addressing the wider determinants of health'.
"The country needs a long term strategy on improving health that doesn't change with each incoming government. Improve overall public services, e.g. everyone to have basic level of income, secure employment and housing. This will help improve health outcomes when people don't have to stress and worry about heating their homes or putting food on the table."
"We need to see services such as housing and employment as part of the wider determinants of health AND as key contributors to care pathways.”
How is NHS Providers responding?
The insights from this research will inform the work of our organisation on the topic of health inequalities. We will utilise the results to advocate on behalf of our members' needs to achieve the changes we are all striving for in the reduction of health inequalities.
We are also supporting members to identify and fulfil their role in addressing inequalities. Our support offer for trust boards aims to help trust leaders make sense of health inequalities and embed it as part of core business, with resources informed by our research and engagement with trust leaders, through webinars, briefings, peer-to-peer support opportunities, and the dissemination of case studies.