Concern about the impact of seasonal pressures over winter on your trust and system(s)
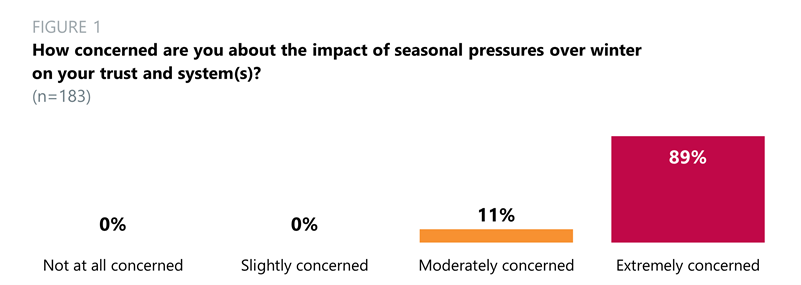
- Almost nine in 10 trust leaders (89%) across all trust types said they were extremely concerned about the impact of seasonal pressures over winter on their trust and local area. 11% said they were moderately concerned. Last year, 87% of trust leaders were extremely concerned.
- Many respondents raised concerns over workforce issues, including high numbers of vacancies, challenges with retention, high absence rates, and staff wellbeing.
- Respondents also highlighted issues surrounding patient flow, with ambulances queueing outside emergency departments in some areas, long lengths of stay, and difficulties in discharging patients from hospital in a timely way due to social care capacity not keeping up with demand. Other areas of concern identified included the risk of COVID-19 resurfacing and the risk of a bad flu season. Respondents from mental health trusts stressed that the pressures on those services were not sufficiently recognised.
The number of patients in our intermediate care units and urgent community response teams who are ready to move on to other services is already at an all-time high at the end of September. 70% of these delays are directly attributable to a lack of social care options.
Chair, community trust
There used to be a cycle of seasonal pressures, whereas it now feels as though summer is the new winter. In addition, staff are exhausted from COVID-19 and all the changes that have occurred and there has been no respite before we hit the onslaught of winter.
Company secretary, acute trust
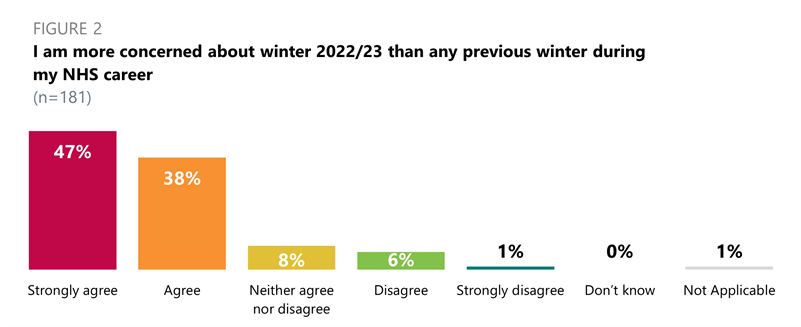
- When asked if they are more concerned about winter 2022/23 than any previous winter during their NHS career, most respondents (85%) strongly agreed (47%) or agreed (38%) across all trust types.
What is your trust doing to ensure you are in the best position to sustain high quality services for patients this winter?
- The most common themes emerging from the responses to this question included partnership working and making plans to support staff wellbeing, including cost of living initiatives. Many respondents mentioned the need to improve patient flow by opening additional capacity and virtual wards. Members also stated that they are trying to increase their workforce capacity through recruitment, including new joiners from overseas.
What is/are your ICS(s) doing to ensure your trust and its partners are collectively in the best position to sustain high quality services for patients this winter?
- The most frequent responses to this question focused on: encouraging collaboration with system partners across services, joint winter planning initiatives, and holding regular winter response meetings. Other, less common answers included mutual aid, creating extra capacity and winter funding.
Confidence that ICB(s) allocations will account for additional in-year cost pressures since the start of 2022/23
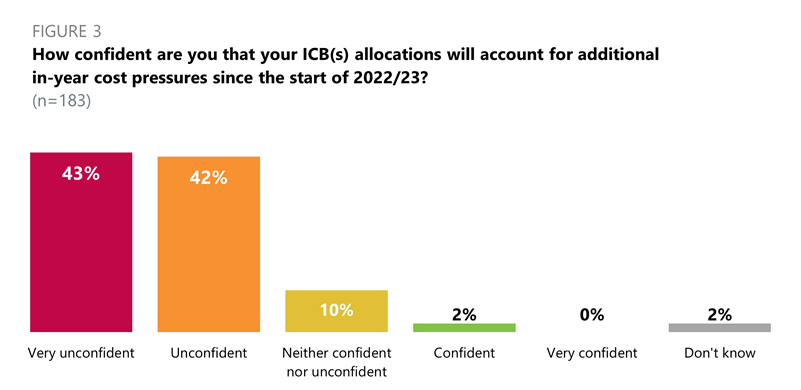
- Across all trust types, 85% of respondents were very unconfident (43%) or unconfident (42%) that their ICB(s) allocations will account for additional in-year costs since the start of 2022/23.
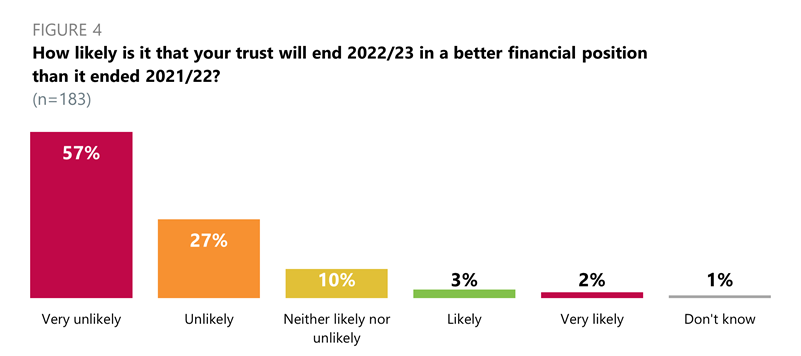
- Across all trust types, 84% of trust leaders said it was very unlikely (57%) or unlikely (27%) that their trust will end 2022/23 in a better financial position than it ended 2021/22.
We have significant vacancies driving pay underspends so while the financial position looks healthy, we want to recruit as quickly as we can.
Chief executive, community trust
It is unlikely that all recurrent efficiency targets for 2022/23 will be identified and delivered putting additional pressure into next financial year (2023/24), this coupled with further reduction in non-recurrent COVID-19 allocations will mean 2023/24 will be even tougher than this year. Recurrent pressures in 2022/23 that are not fully funded, e.g., pay award.
Ambulance trust
Accessing operational and national capital funding over 2022/23
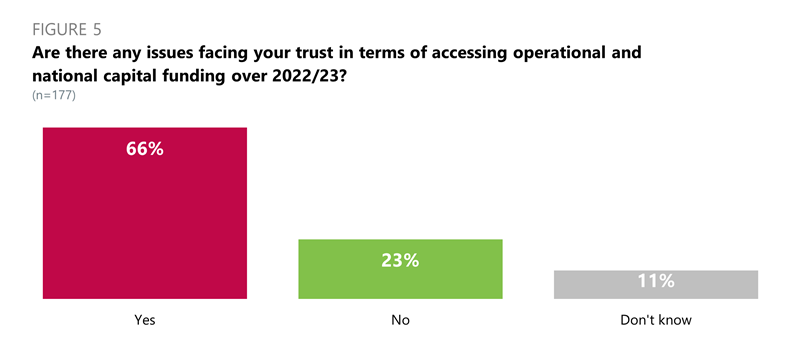
- Two thirds of all trust leaders (66%) said there were issues facing their trust in terms of accessing operational and national capital funding in 2022/23.
- In the comments, the main concerns expressed by members were around capital department expenditure limits (CDEL) being too low and restricted. Respondents also mentioned challenges in the process, highlighting delays in approvals and application turnaround speeds which were Further issues reported by members included poor estates, a last-minute 'bidding culture', and mental health and community trusts losing out to the acute sector.
Our existing building projects have seen dramatic cost inflation. Only by squeezing, begging and rephasing works can we afford to continue with what was previously agreed. We have a deep sense of foreboding for future years. Capital investment needs increasing.
Chair, mental health/learning disability trust
CDEL is a massive struggle for us and, as we are building a new community hospital, the capital position for next year is of concern, even though we have our own capital identified within the trust.
Chair, combined acute and community trust
What do you see as the biggest risks to the services that you, or those in your system(s), provide?
- There was overwhelming concern for the workforce, with respondents highlighting issues surrounding recruitment, retention, absences, morale, burnout, and the potential for industrial action.
Workforce capacity including loss of goodwill from staff following the pay award.
Combined mental health/learning disability and community trust
Workforce gaps continue to be a huge risk, and the more challenging it becomes the more likely people are to find alternative employment that rewards them better financially during the cost-of-living crisis.
Strategy director, combined mental health/learning disability and community trust
- Many respondents also emphasised underinvestment and lack of capacity in the social care sector and the knock-on effect this has on patient flow particularly due to delayed discharges. Responses also commonly reflected concern about financial pressures exacerbated by the cost-of-living crisis, the heightened demand for services and increased respiratory illnesses over the winter.
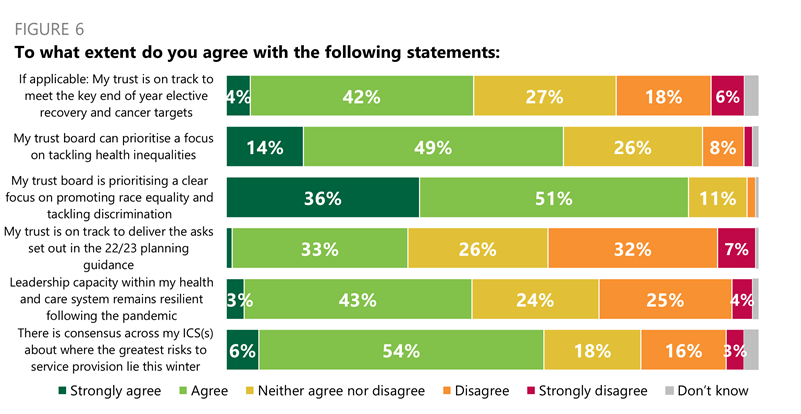
- When asked if their trust was on track to meet the key end of year elective recovery and cancer targets, nearly half (46%) of trust leaders strongly agreed (4%) or agreed (42%).
- Almost two thirds (63%) of respondents strongly agreed (14%) or agreed (49%) that their trust board can prioritise a focus on tackling health inequalities.
- An even larger proportion (87%) strongly agreed (36%) or agreed (51%) that their trust board is prioritising a clear focus on promoting race equality and tracking discrimination.
- However, only about one third (34%) of respondents strongly agreed (1%) or agreed (33%) that their trust was on track to deliver the asks set out in the 2022/23 planning guidance.
- Nearly half (47%) strongly agreed (3%) or agreed (43%) that leadership capacity within their health and care system remains resilient following the pandemic.
- Six in 10 (60%) trust leaders strongly agreed (6%) or agreed (54%) that there is consensus across their ICS(s) about where the greatest risks to service provision lie this winter.