This framework sets out core principles for understanding and taking action on health inequalities that have developed or worsened as a result of the COVID-19 crisis. It is intended to support NHS trusts during delivery of surge plans, as well as in service restoration and recovery action.
It has been developed by the Provider Public Health Network, a group of public health professionals who work in or closely with NHS provider organisations, with support from Public Health England (PHE), and in conjunction with NHS Providers.
Health and care services worldwide have faced an unparalleled challenge in responding to and managing the impact of COVID-19. The disproportionate impact of the virus has highlighted longstanding health inequalities – marked differences in health outcomes that have been described by The Kings’ Fund as “avoidable, unfair and systematic differences in health between different groups of people”, for example for people from areas with higher levels of socio-economic deprivation, or for those from Black, Asian and minority ethnic (BAME) communities.
The Health Foundation has highlighted that for COVID-19 there are “clear inequalities in exposure to infection, the ability to ‘socially distance’, and in who will bear the brunt of the longer term negative impacts from COVID”.
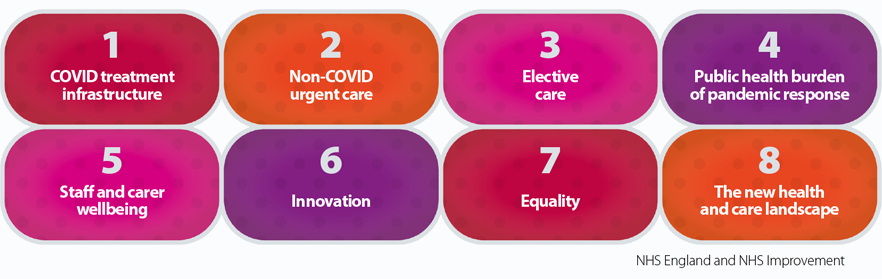
Response planning for NHS trusts to this crisis has been described as falling within three phases of pre-surge, surge, and restoration and recovery, while also preparing for and coping with a second surge. All underscored by the core NHS optimal care delivery principles (figure 1).
NHS trusts have been widely recognised for their significant and sustained efforts to both deliver a COVID-19 surge response, while also undertaking service restoration and recovery, to help meet the broader non-COVID population health and wellbeing needs.
To help address this disproportionate impact of COVID-19, NHS trust boards will be aware of the COVID-19 phase 3 implementation requirement that was introduced, for ”all systems and every NHS organisation should therefore identify, before October [2020], a named executive board-level lead for tackling inequalities”.
Executive leadership can enable coordinated trust-wide efforts to help achieve the health inequalities-related priorities of the COVID-19 response phase 3:
- reducing unmet need and tackling health inequalities, work with GPs and the public locally to restore the number of people coming forward and appropriately being referred with suspected cancer to at least pre-pandemic levels
- specific actions to support any groups of patients who might have unequal access to diagnostics and/or treatment
- management of elective waiting lists and performance at system as well as trust level to ensure equal patient access and effective use of facilities.
NHS phase 3 work is also taking place within the context of a number of catch-up programmes, for example screening and routine vaccinations which were impacted by reduced coverage during the spring 2020 pandemic response, and programmes on deferred elective and other care needs where 89% of trusts had expected to see a backlog of people awaiting care. This is within a context of NHS trusts managing further outbreaks alongside planning for winter and other threats to health including seasonal influenza.
Figure 1
This framework offers principles for a population health level approach to understanding and taking action on health inequalities which have developed or worsened as a result of the COVID-19 crisis that began in 2019/20. It focuses on what NHS acute hospital trusts and mental health and community trusts can do, working as part of an integrated health and care system. The framework is intended to help NHS provider trusts to systematically review, describe, prioritise and further develop their role in addressing health inequalities during response and recovery from the COVID-19 crisis and as part of their broader core efforts to meet the needs of their local population.
In addition to helping deliver against foundation trust and Social Value Act responsibilities, tackling health inequalities as part of core business has been shown to optimise patient outcomes from clinical interventions and surgical procedures.
Some of these activities are already taking place in local government, within health and care partners, and NHS providers. However, systematically strengthening the focus on action to reduce health(care) inequalities is achievable and can make a significant difference in many situations.
This framework was developed by the Provider Public Health Network and builds on the Population health framework previously published with NHS Providers. Examples from practice in NHS trusts are also included in the document COVID-19: Mitigating impact on health inequalities developed by the Provider Public Health network in conjunction with the Royal College of Physicians, PHE and NHS Providers.
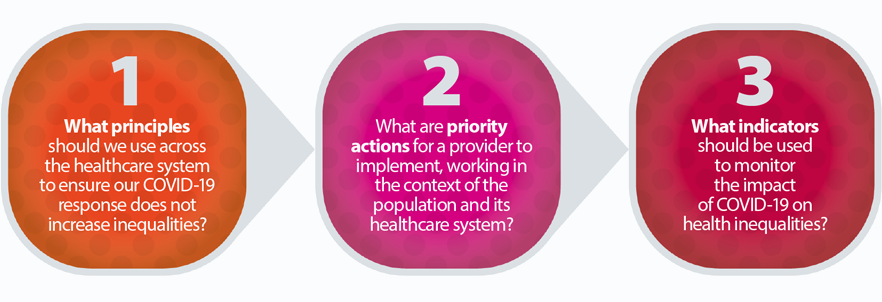
This framework is designed to assist NHS provider trusts to address three main areas: