One of the key lessons learned from the evolution of testing during the pandemic is the need for greater local involvement with and buy-in to national plans. Indeed, this lesson is relevant to a number of challenges over the past few months, including the provision and supply of PPE. While the testing framework has been developed and managed nationally, and credit needs to be given to the government for recent sustained increases in daily capacity and positive trends through the test and trace service (Department of Health and Social Care, July 2020), the story of the next few months will be centred around local resilience and response.
This has already come to light through the focus on local outbreaks and local management of spikes in transmission in Leicester, Blackburn and, inevitably, elsewhere. Trusts have emphasised the need for greater coordination between the national testing service – including test and trace – and local public health teams and systems. The delays in sharing critical, detailed testing data (Financial Times, June 2020) with local officials did not help Leicester as its leaders sought to respond to the city’s outbreak, and this approach should not be repeated if and when outbreaks emerge in other parts of the country.
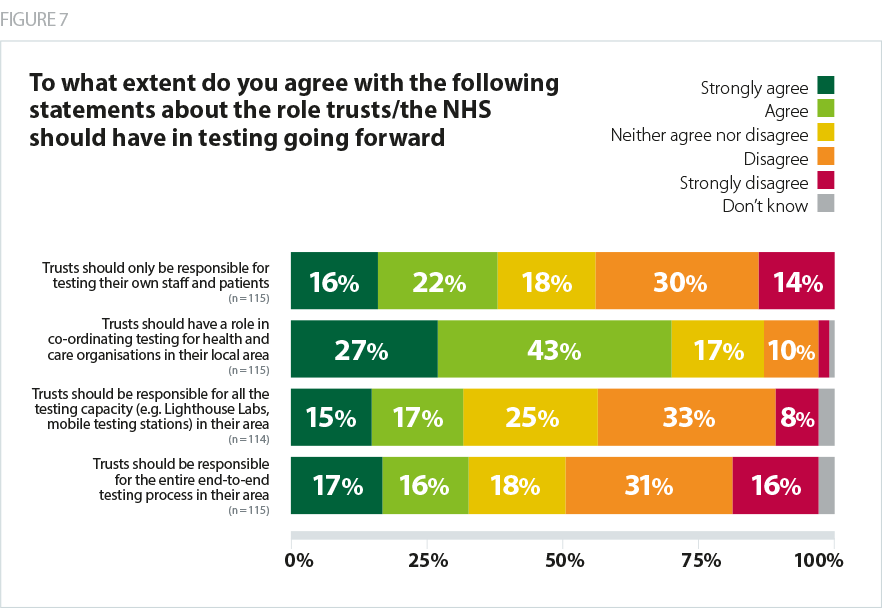
Our survey clearly showed that trusts want to take on a greater role in the management of testing locally, with a strong majority of respondents (70%) agreeing that their organisation should have a role in co-ordinating testing for health and care within their local area. More significant involvement for key local partners was also a development many would support, including for primary care providers (67% of trust leaders agreed they should have a bigger role), and local authorities (58% agreed).
However, it should be noted there is a clear message in feedback from trusts that, while greater involvement and coordination of testing for their organisations and local partners would be beneficial, shifting responsibility entirely to each local area would not be favoured as a solution. Less than a third of respondents (32%) felt trusts should be responsible for all the testing capacity (e.g. Lighthouse Labs, mobile testing stations) in their area, and similarly less than a third (32%) said trusts should be responsible for the entire end-to-end testing process in their area.
When looking in more detail at those who did indicate a desire to take on responsibility for all the testing capacity or the entire end-to-end process in their local area, the same trust leaders responded positively to both statements. However, there was no clear split between acute trusts (who are more likely to have their own testing facilities and subsequently receive results much faster) and other trust types, suggesting the appetite for greater oversight is driven by a range of reasons, some of which are likely to be specific to local conditions and relationships.
Another indication of the range of opinions towards testing held by trust leaders was seen in responses to the question about current involvement in surveys or research on antibody testing (e.g. Public Health England SIREN study). Two thirds (67%) said their trust is taking part, but many expressed doubts about the immediate value in the short term and the services they are trying to deliver. Wider epidemiological benefits were recognised, and participation was noted in having a positive effect on staff confidence, but the time and effort required at a time when resources are scarce brings into focus the difficult balancing act faced by trusts.