Trusts have emphasised the complexity of the task they face in planning their journey towards a ‘new normal’. When asked about the challenges they face in returning to a level of service comparable to pre-COVID-19, trusts agreed that they continue to face a number of constraints:
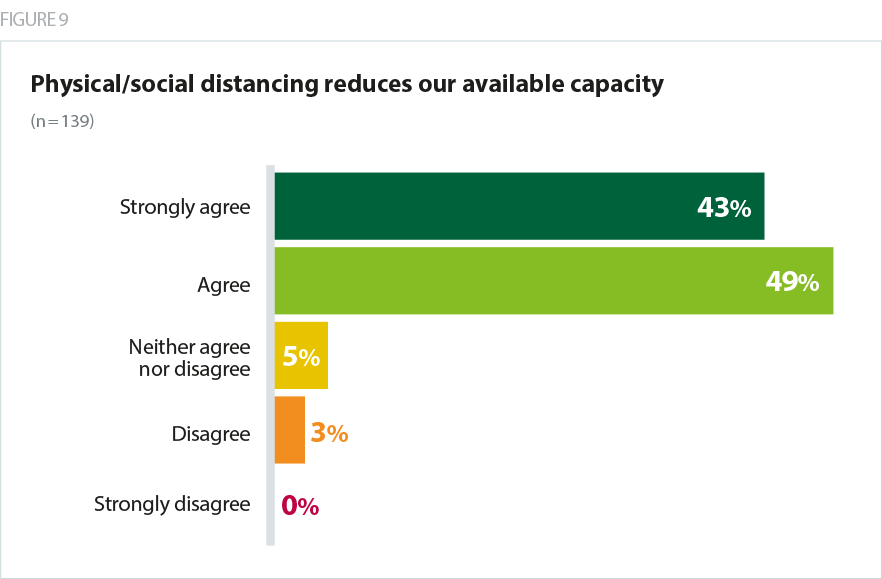
- In particular, the need for social distancing and its impact on available capacity was almost universally a concern. More than 9 in 10 (92%) agreed that physical distancing reduces their available capacity. This will manifest in numerous ways, for example:
- atients will need to be more spaced out on hospital wards, reducing bed space. Average bed spacing in hospitals ranges between 1.6m in older buildings and 1.8m in newer hospitals, and space between staff around beds must also be taken into account. Trusts estimated that the 2m rule reduced bed space by up to a third, and a change to the rule reducing the distance to 1m, when supported by PPE and testing, is a welcome boost to capacity.
- A&E departments will face similar restrictions with a need to provide adequate distance between patients in waiting areas and treatment bays, raising questions for trusts about how they will accommodate all those who need treatment.
- Fewer ambulance trusts (80%) and community trusts (73%) are experiencing this challenge relative to their acute (95%) and mental health (90%) colleagues but significant proportions of those responding still highlighted these concerns. This reflects the same requirements for physical distancing in community hospitals, mental health services and when visiting people’s homes, and the increased requirement for infection control and deep cleaning in the ambulance sector.
The majority (89%) of trusts expect to see an increased backlog of people waiting for care, with a knock-on effect on their ability to return to a normal level of service. Some trust leaders responding estimated that it would take a year to clear waiting lists for outpatient services, elective surgery, but also immunisation programmes, children’s services, health visiting and safeguarding caseloads. This is coupled with the likelihood of a surge in the number of people needing care following the easing of lockdown measures. Mental health services in particular are already seeing a rapid rise in need among those who have experienced mental health problems either during, or as a direct result of, the coronavirus outbreak and lockdown. Community trusts are faced with a number of patients who have been critically unwell with COVID-19 and will need support and rehabilitation.
The problem is our previous capacity was already outstripped by unmet and unfunded demand, because of the treatment gap, and the post-COVID mental health surge will compound that. We have kept a remarkable amount going through the pandemic; we will need well over 100% to keep pace afterwards and staff are tired and in chronically short supply, especially the highly trained people we need for more complex cases - and that is what we are seeing.
combined mental health/learning disability and community trust
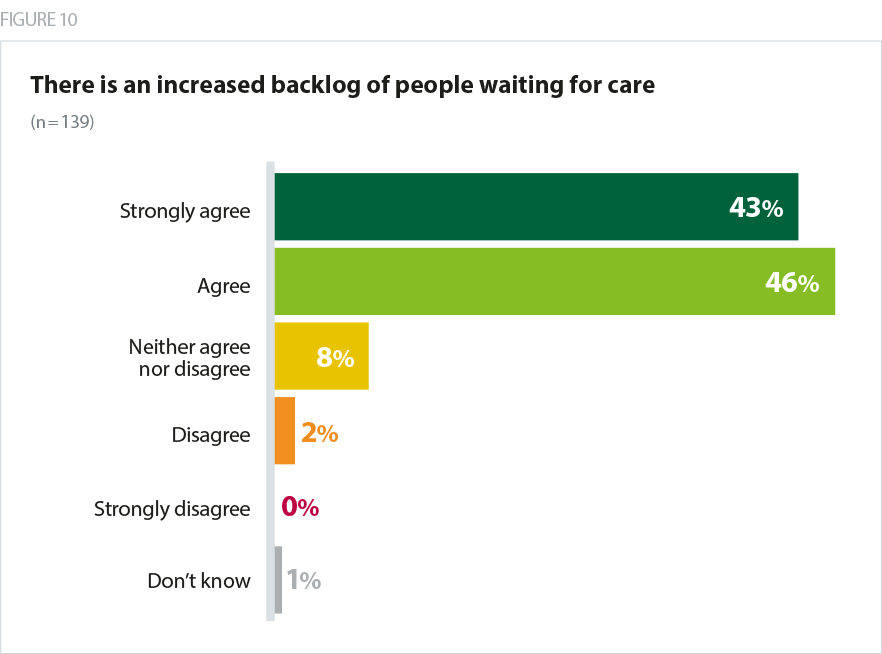
Trusts emphasise the complexity of the modelling required to project the capacity required to meet demand from new and existing patients over the coming months. The combined effect of a long pause in normal service provision, a backlog of new demand, lockdown-generated demand, and a reduction in normal capacity, is likely to be significant.
Further impacting on capacity is the need to retain surge capacity to deal with an unpredictable level of COVID-19 demand, with 80% of trusts agreeing that this has a bearing on how long it will take to return to full capacity.
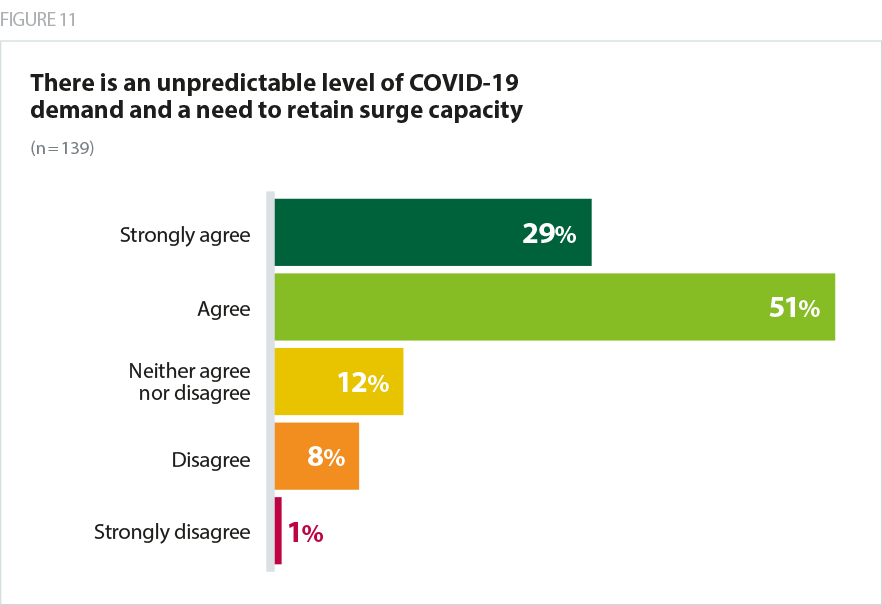
While cases continue to fall, trusts are alive to the possibility of future waves of the outbreak as social distancing measures are eased. The rapid response to the outbreak in March entailed a highly disruptive process of switching off services, cancelling planned care, redeploying staff and repurposing wards and operating theatres to scale up ICU capacity. Not wanting to go through this process again, trusts are cautious as to how quickly, and how closely, they return to business as usual without compromising their ability to retain surge capacity.
PPE and COVID-19 testing capacity remains a concern with more than half of trusts agreeing each of these is an issue (53% and 57% respectively).
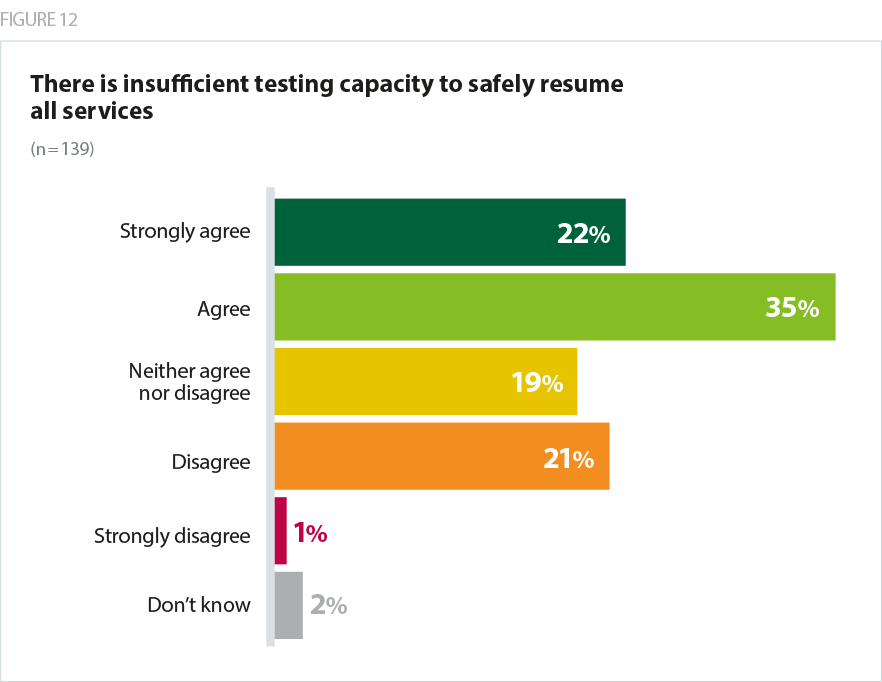
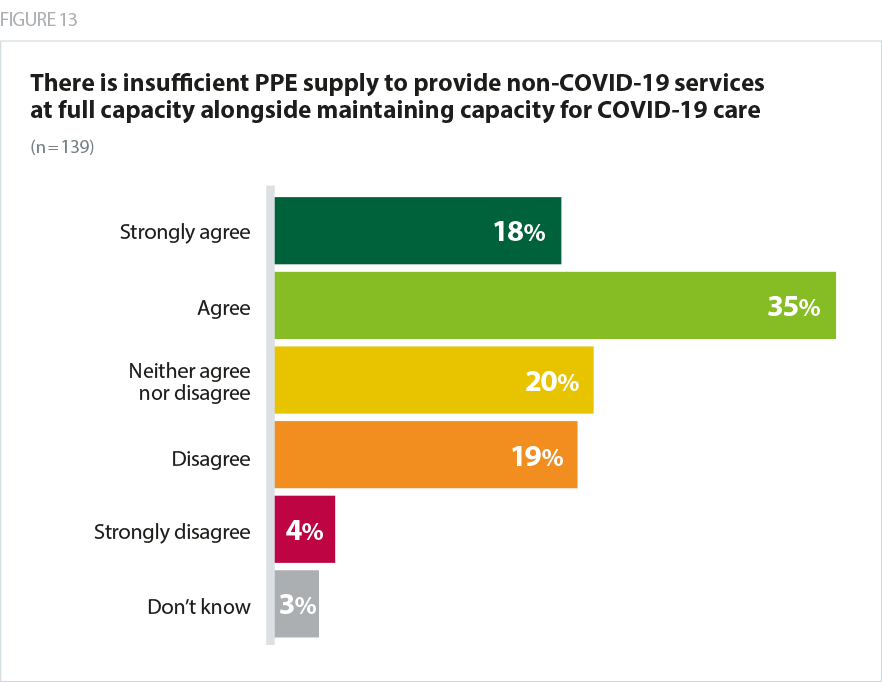
The ongoing insecurity of PPE supplies coupled with new guidance that all staff in NHS trusts must wear masks at all times, leaves trusts with uncertainty about the volume of care they will be able to carry out, and similarly as trusts scale up services the need for the capacity to test patients and staff increases so that the integrity of COVID-19 and non-COVID areas can be maintained. Trust leaders have also raised the challenge of the lack of availability of fit testing for FFP3 masks for community trust staff in particular.
While trusts talk about a surge in demand for care as well as the increased level of need created by a pause in services, they are also concerned that people remain reticent to receive care in hospital due to the risk of catching COVID-19 as an inpatient, and are looking to provide the reassurance patients need to feel safe in receiving care in hospital and mitigate the risk of harm created by delayed treatment. One trust estimated 25% of their patients offered surgery have declined it.
Though we regularly review the longer waiters I am clear that there will be a building level of harm as people do not present and secondary care do not refer. These referrals are a fraction of previous levels.
acute specialist trust
Many of our services are provided for older people who might be reticent about accessing services in the current circumstances which means we need to ensure we can accommodate their concerns appropriately.
community trust