After scaling back its approach to regulation to give trusts the space to manage the operational pressures of the pandemic, CQC confirmed that it would move away from its previous approach and introduce a transitional monitoring approach to function as a 'prototype' model ahead of the implementation of its new strategy from summer 2021.
CQC has committed to a stronger focus on safety, access, and leadership, and indicated that regulation will be more intelligence led, less burdensome, with more work done offsite than in the prior inspection-led model. CQC has also been clear that it acknowledges the burden of the inspection regime and plans to move to a leaner approach.
This scaled back approach during the pandemic has subsequently been captured within CQC's new strategy as it reconsiders regulation in the current context and moves towards a more proportionate and risk-based approach. The pandemic has in many ways accelerated change, with providers working more collaboratively within local systems, as well as delivering care in new ways such as through digital channels. CQC has therefore identified the need to transform and ensure its regulatory approach is relevant, flexible, and fit for purpose in an evolving system. As part of this, it has set out an intention to place a greater emphasis on providers' role in systems, how quality of care is measured across pathways, and the need to tackle health inequalities as part of high quality care.
Regulation in the context of COVID-19
In the survey, we asked respondents to reflect on CQC's regulatory approach before the start of the COVID-19 pandemic and during the pandemic to explore the impact the scaled back regulatory approach had on trusts. Despite the helpful measures put in place by CQC to allow trusts to respond to the pandemic, views about its regulatory approach over the past year were mixed.
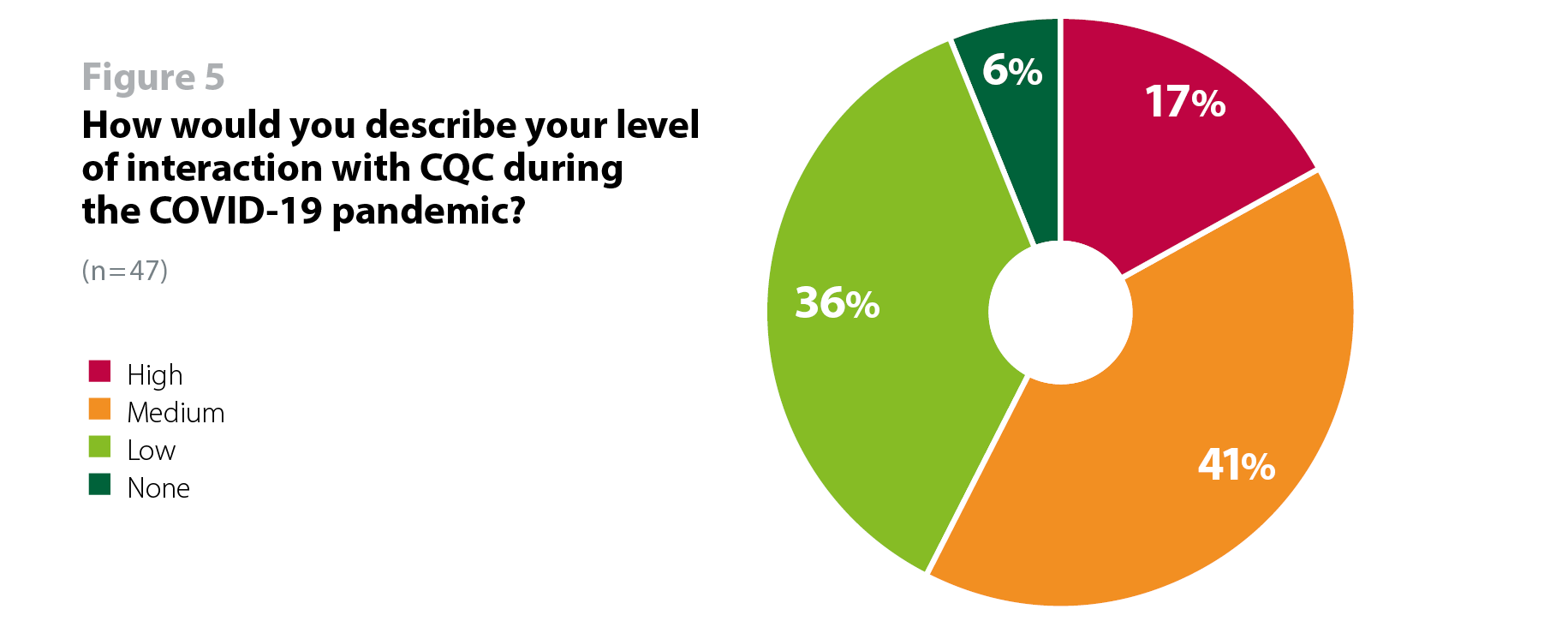
When asked about the level of interaction they had with regulators during the pandemic, respondents reported lower levels of interaction with CQC (high, 17%; medium, 40%) than with NHS England and NHS Improvement (high,38%; medium, 49%) (figure 5). This is indicative of the different roles NHS England and NHS Improvement and CQC played during the pandemic and reflects CQC's scaled back approach in which they shifted from routine inspections and provider information requests (PIR) to a more risk-based transitional monitoring.
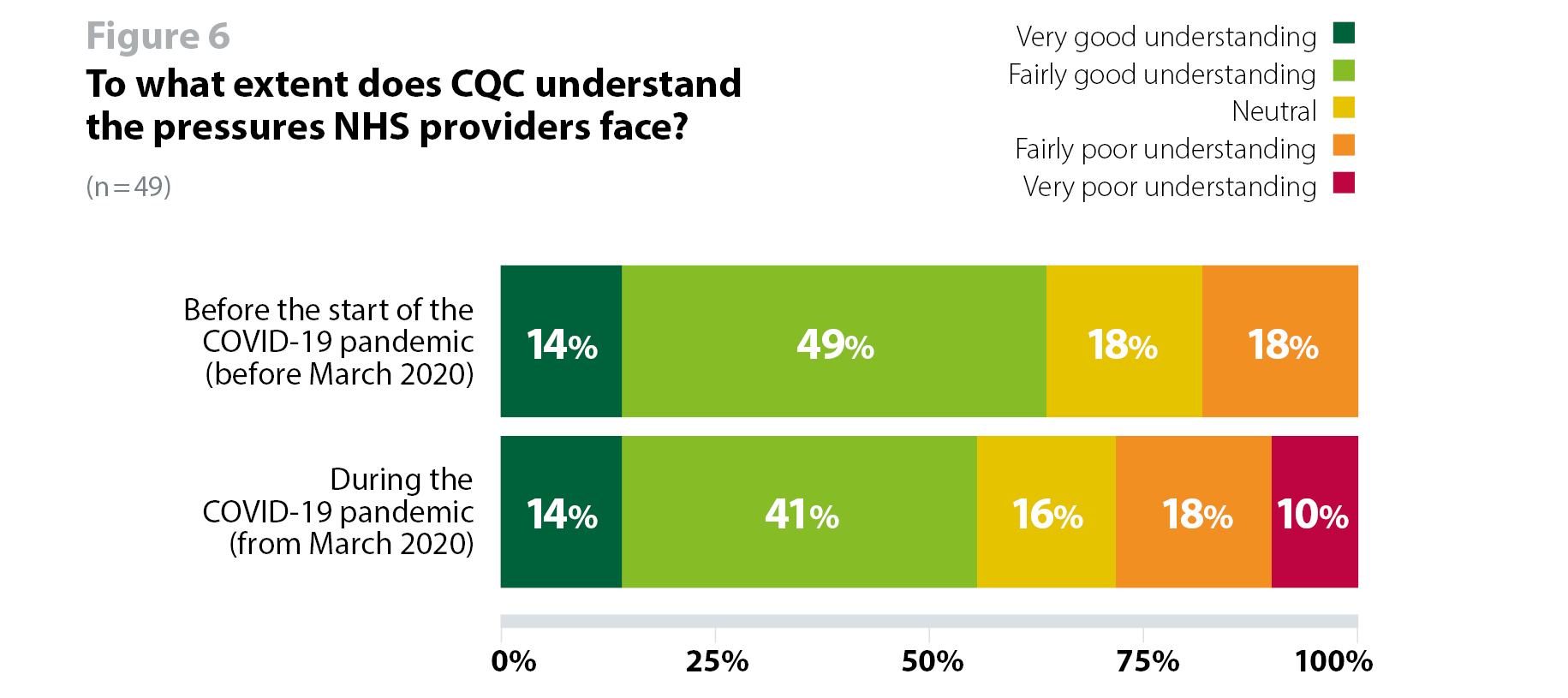
When asked whether CQC understood the pressures providers face before and during the pandemic, almost two thirds (63%, 31 respondents) of respondents said CQC did understand the pressures providers faced before the start of the pandemic, but this decreased to just over half (55%, 27 respondents) during the pandemic. In addition to this, while three in five (60%, 28 respondents) trusts felt that the scaled back approach reduced burden to allow them to focus on managing COVID-19, the comments and other feedback we received on this showed variable views (figure 6).
It is likely that this variation is due to how CQC adapted its approach between the first and second wave. We received both positive and negative comments about activity undertaken by CQC, and there are indicators that regulatory activity in the second wave created a greater sense of pressure at the frontline than it did during the first wave. For example, trusts have told us that while CQC reduced its regulatory activity quite significantly during the first wave last spring, this was not the case during the second wave, despite the operational pressures being just as intense, and often more intense than in the first wave.
Since the pandemic [the regulators] have largely been less intense and more understanding of operational pressures, certainly in the first phase. Latterly there has been more regulatory demand, particularly from CQC.
...we have had more [meetings] during the time period of COVID from both [regulators], but both are proportionate.
The CQC has been reasonable and supportive in its approach. I commend the plans for the new strategy.
CQC scrutiny has been totally disproportionate, lacking in any sense of empathy for the efforts Trusts have been going through. In my world, most contact has gone online, but has increased (MHA) rather than decreased. Observations about compliance with regards to leave arrangements for inpatients has shown very little understanding of what we have been managing, staffing pressures and the conditions within our communities.
The varied experience of trusts also seems to be the result activity undertaken by local CQC teams, rather than CQC's overall intention set out at a national level. Some have felt that they continued to receive a lot of unnecessary requests from their local team, whereas others felt that their local team could have completed assessments, such as well-led, rather than stopping them midway through the process. This highlights the importance of having strong local relationships between local CQC teams and trusts and echoes previous findings that local relationships and communication is a significant driver of trusts' experience of regulation.
During wave one, NHS England and NHS Improvement provided clarity on expectations from trusts in terms of reducing the bureaucratic burden... This was not replicated by the CQC whose requirements have not changed which inspections being undertaken in a similar format to those pre-pandemic.
CQC has deferred the Trust's well led meetings and interviews,
so we feel part assessed. This was due to COVID-19 so entirely understandable but there did not seem any willingness to undertake Teams interviews with the board, which we found surprising. This has been disjointed and disruptive.
Provider collaboration reviews
Last year, CQC introduced provider collaboration reviews (PCRs) to explore how health and social care providers worked collaboratively in local areas to respond to the pandemic and provide care for particular population groups. The purpose of the reviews was to identify themes and learning that could be used to inform planning over the winter and future waves of the virus, but more broadly to help health and care providers and leaders of local health and care systems plan and work more effectively together.
To date, two phases of the PCRs have been completed. The first review looked to understand how health and social care providers have collaborated to improve care for older people, who are most at risk of COVID-19, while the second looked specifically at how providers are working together to deliver urgent and emergency care services in the context of COVID-19. The remaining three phases of the reviews will focus on cancer services, people with a learning disability and/or autism and mental health services and will take place over spring and summer 2021.
Of the 51 responses to the survey, 11 respondents said their system (i.e. Sustainability and Transformation Partnership or Integrated Care System) took part in a CQC-led PCR since March 2020. Given the low response rate for these questions, the figures in this section should be treated as indicative only.
Of the 11 respondents, two agreed that the review had helped them to understand the effectiveness of their system-wide response to COVID-19, and six (54%) disagreed. Similarly, only two (18%) said they agreed that the review encouraged more collaborative working, and six (54%) disagreed (figure 7).
Only one respondent agreed that the review supported them to improve patient and service user experience, and five disagreed. Similarly, one said they agreed that it supported them to improve patient and service user outcomes in the face of COVID-19, while six (54%) disagreed (figure 7).
Seven respondents disagreed that the review helped them to restore services after the first peak and only one agreed. As for the learning shared from the review, four disagreed that it helped them to respond to winter pressures and further waves of COVID-19, and six disagreed that the review helped them to drive improvement (figure 7).
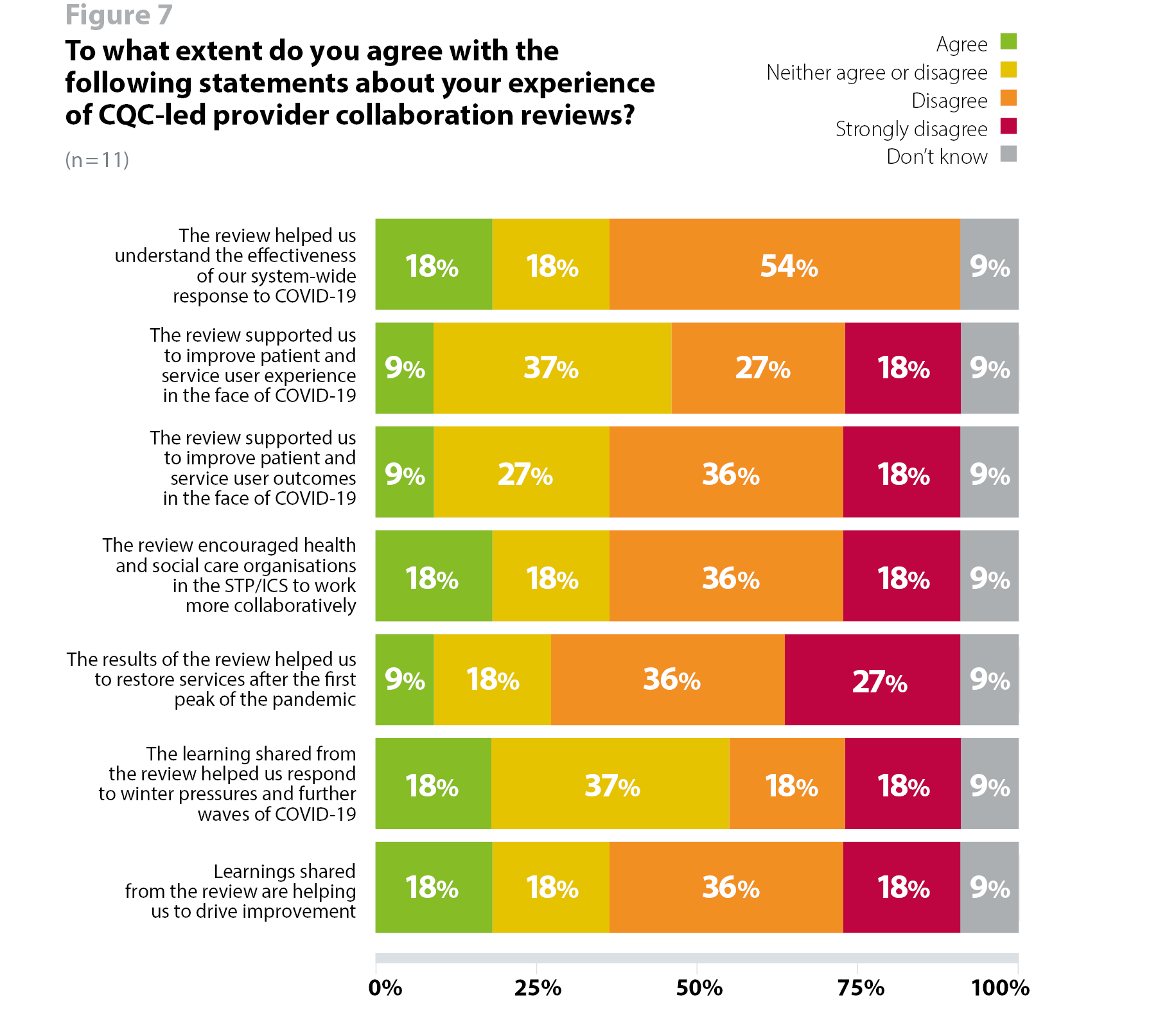
While some trusts felt that the review preparation itself was helpful, other trusts said the review did not necessarily add value or improve their understanding of how to approach collaborative working across systems. Despite these mixed views, the aggregate findings may still be helpful in highlighting learning and systemic barriers to collaboration at a national level.
While this is a small sample of respondents, the findings highlight the importance of using the insight gathered by these reviews to add value and supports trusts and their partners to work collaboratively across systems, drive improvement and restore services from COVID-19. This will be important if CQC are to use PCRs as a tool to review how well health and social care services work together to reduce inequalities, as outlined in its new strategy. We would encourage CQC to consider how it uses the insights of these reviews to develop a more system-focused methodology in the future.
We did not need these reviews to understand our local systems, both issues and what works well, and both before and during
the pandemic.
It may be that in my role I simply don't have the awareness of any benefits deriving from this work.
Preparation across system partners for the PCR was instructive, but there was little to no local benefit. There was no learning shared locally or specifically published by CQC that could help us reflect and improve local system resilience and outcomes for patients.
New strategic approach to regulation
CQC has recently set out plans to change its regulatory approach under four key themes. These themes include regulation that is driven by what people expect and need from services; a smarter approach to regulation that is more flexible and dynamic; regulation that enables stronger safety and learning cultures; and accelerating improvement. Throughout the four themes, a common thread focuses on their ambition to understand how health and care systems are working together to reduce inequalities.
We asked providers to share their views on each of the four themes outlined in CQC's draft strategy prior to the launch of its formal consultation in January 2021. Respondents expressed very strong support for the direction of travel but raised questions about what the new approach will look like in practice.
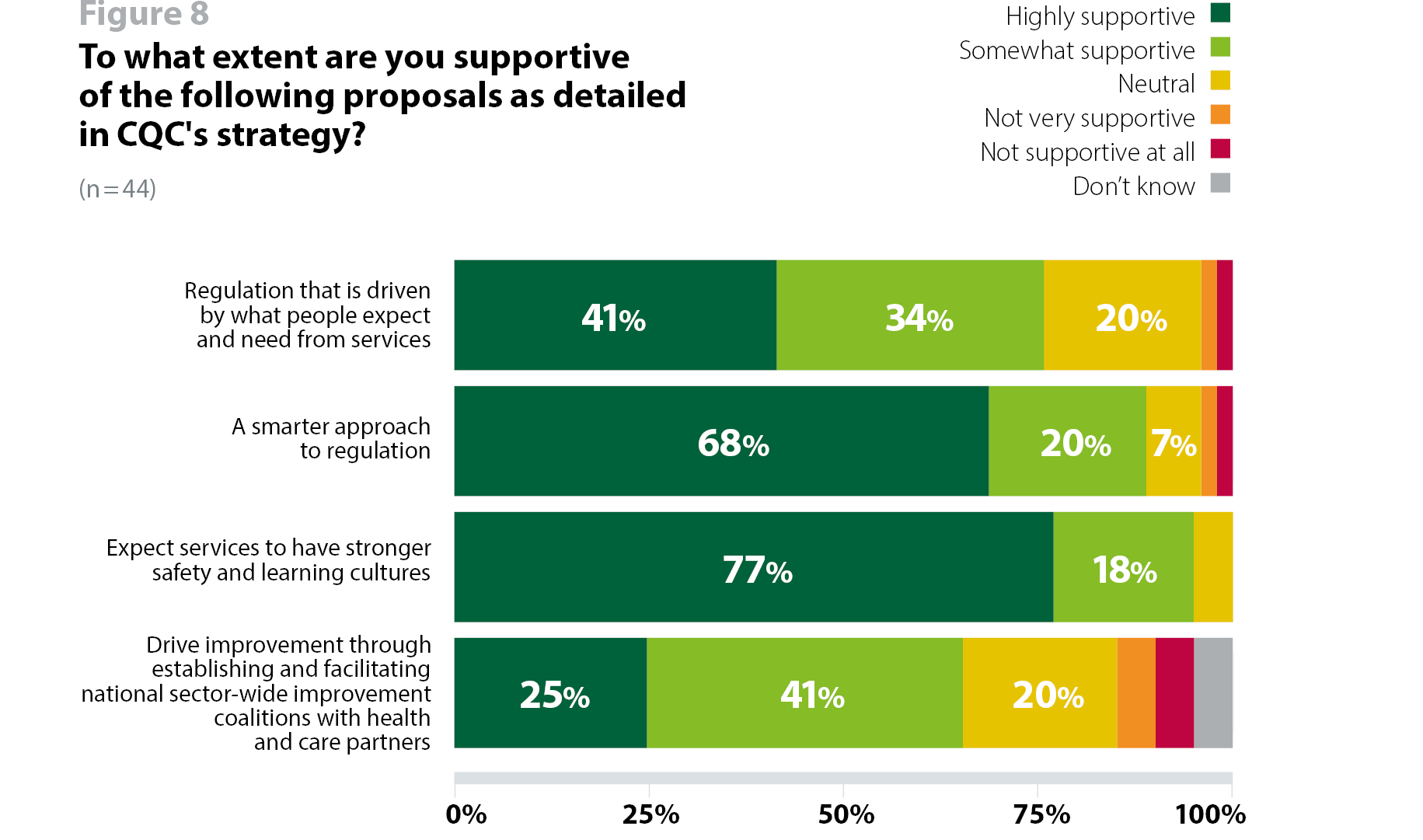
Three quarters (75%, 33 respondents) of respondents to our survey said they are supportive of the proposal to ensure regulation is "driven by what people expect and need from services, rather than how providers want to deliver them" (figure 8). Evidently, trust leaders support the principle of planning and delivering care to meet the needs of people using services. The main consideration will be to ensure sufficient flexibility to allow trusts and their partners to determine the most appropriate way of meeting local population health needs while meeting the requirements of a nationally defined framework for performance and quality.
I am strongly in favour of user-driven changes but there does need to be some consideration for providers to be able to deliver services as they feel appropriate for their organisation as a whole... For example, you can't place a burden such as Cost improvement programmes on trusts and then say they must deliver services as dictated by patients - there needs to be a balance of input and control. And of course, you can't be everything to everyone, and providers need to be able to have some autonomy in this decision making/ planning.
Nine in 10 respondents (89%, 39 respondents) are supportive of CQC's proposal for a smarter approach to regulation, with an ambition to provide an up-to-date, consistent, and accurate picture of the quality of care in a service and in a local area (figure 8). Again, trusts welcome this proposed shift towards regulating more dynamically and proportionately. However, getting the implementation of this ambition right will be crucial to ensuring it has the intended impact.
The devil is in the detail. On paper, the current approach by the CQC seems proportionate. However, in practice the framework is not applied consistently and there is a varied level of quality of regulatory service offered.
Almost everyone who responded to this survey (95%, 42 respondents) said they are supportive of the proposal for CQC to focus more on safety and learning cultures, making it the most highly supported of the ambitions on which we sought trusts' views (figure 8). We know that NHS staff and organisations treat safety as a top priority, so this is expected. Similarly to the smarter regulation proposal, comments from trusts centred on successful implementation.
[CQC] needs to ensure inspectors and assessment tools have the maturity to measure the important elements like culture and emotional intelligence not just weighting inspections to what’s easiest to measure.
Others highlighted the need for CQC to ensure it avoids duplication with other national bodies and questioned what role CQC might play in the safety landscape given the work other bodies are doing in this space – a stronger emphasis on safety without adequate coordination with these partners could not only confuse the landscape but also add burden to trusts.
I do not think a stronger approach to safety is applicable to CQC as this cuts across HSIB - only one of these should do this. Focusing more on improvement does not sit well with the current ethos and culture of CQC - to change to this would require a change of direction for the leadership team and new inspectors.
I'd like to see a robust and consistent methodology for quality assurance used.
Two thirds (66%, 29 respondents) of respondents said they are supportive of the proposal to establish and facilitate national sector-wide improvement coalitions to improve the availability of direct, tailored, hands-on support (figure 8). Of the four themes outlined in CQC's strategy, this had lower levels of support from respondents, raising questions about avoiding duplication and ensuring CQC focuses on its core regulatory role.
It is important that work to develop improvement coalitions does not duplicate arrangements that already exist and therefore not see as the CQC looking to expand their remit.
I am not sure establish/facilitate nationwide improvement coalitions is consistent with the CQC regulator role and this is already a crowded area. Better for a focus on improving the current approach rather than adding another body. Also, with the increase in the number of prosecutions, can you really expect staff to be open in a learning environment with the CQC present?
I do not see this as a role which sits with a regulation of quality as this is about service improvement - please encourage CQC to stay away from this as this is all about development not regulation - much better for say King's Fund, NHS Providers and NHS Confederation to support this.
Regulation of systems
The COVID-19 pandemic has accelerated the shift towards health and care services working more collaboratively as a system to deliver care. As such, CQC has identified that its 'single provider service model' is no longer fit for purpose in the current and evolving landscape. It has therefore outlined its intention to review how well health and care systems are working together.
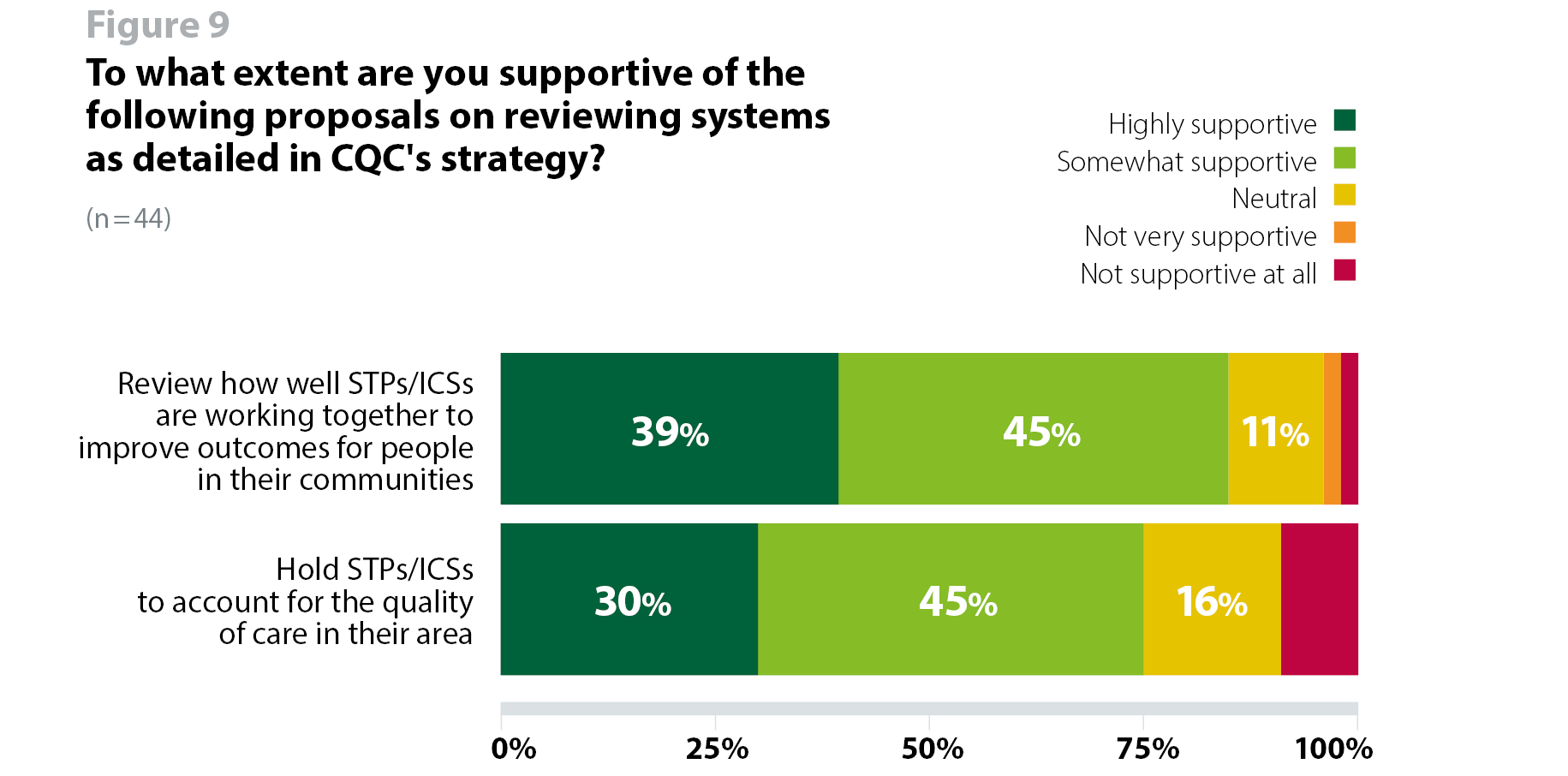
Trusts are broadly supportive of CQC's intention to take the system-wide context into consideration when reviewing services. More than four in five (84%, 37 respondents) respondents expressed their support for CQC's ambition to review how well Sustainability and Transformation Partnerships (STPs) and Integrated Care Systems (ICSs) are working together to improve outcomes for people in their communities. Additionally, three quarters (75%, 33 respondents) said they would be supportive of its proposal to hold STPs/ICSs to account for the quality of care in their area (figure 9).
...Re STP/ICS holding to account, once legislation is approved then the CQC should focus on system but also review work with individual providers so as to avoid duplication."
The main concerns trust leaders have noted, including through our broader engagement with them outside of this survey, are around the context of planned legislation to support the shift towards system working. While trusts support this direction of travel, their comments highlight a need to ensure changes to regulating systems are not made too hastily before the full impact of legislative proposals is seen.
Without primary legislation to enable proper governance of any new bodies created by ICPs/ICSs then holding to account these non-legal entities becomes problematic for everyone, time consuming and confusing.
In our last regulation survey report, we noted that this shift in the operating environment "serves to highlight that providers, their local partners, and the national bodies are continuing to navigate a complex environment and developing new regulatory models to reflect the changes taking place locally will only grow as a priority." Trusts have again echoed the complexity of the environment they are operating in and highlight the need for any changes to be flexible, adaptable, and responsive to a changing health and care architecture.
We also asked trusts what changes they felt could be made to CQC's existing regulatory framework to support the further development of system working and integrated care. Our findings highlight a need to ensure new capabilities and infrastructure are developed to support this shift, as well a focus on ensuring the approach is data driven.
To make the change successfully it's critical the CQC undertake more robust training and induction of staff so they can understand the complexity of systems without extensive experience of working in systems inspectors will struggle to review meaningfully and it will become a checklist/tick box approach, missing the point.
Much more data driven in terms of overall outcomes for patients and health and wellbeing measures across pathways.
Trusts also commented on the need for CQC to determine what specific role it will have in regulating and reviewing quality care across systems, but also more widely in assisting in the development of supporting systems to build their own quality management systems.
... The CQC need to determine whether it is replicating audit functions or whether it is trying to take a more strategic critical friend approach to assist the development of new systems/
ICS, which is the space it should inhabit so it can share other good practice from around the country.
ICSs have no quality management systems, no quality assurance, and no quality manual or procedures. CQC should assist the new organisations to build a quality management system and a health and safety system and an environmental management system to bring NHS management up-to-date with all other major enterprises globally.
On the whole, it is clear that trust leaders experience organisationally-focused regulation as a potential barrier to a more collaborative way of working across a system, and are keen for regulation to support collaboration and take wider system issues into consideration.
To review services from a whole system perspective rather than just individual organisations. Sometimes there are important inter-dependencies which need to be part of an overall assessment of services that meet the needs of the population in the broadest sense.
They need to link in with the wider system and not just providers.
An emphasis on partnership for the benefit of patients and system learning.
CQC's success in effectively reviewing health and care systems will depend in part on the relationships developed between trusts, clinical commissioning groups (CCGs), STP/ ICS leaders and other system leaders. As well as working with NHS England and NHS Improvement to design a system level regulatory model that does not duplicate or create additional burdens and where accountabilities are clear. However, if CQC does not take on additional responsibilities for regulating systems it will be imperative that it provides clarity over how it intends to take system issues into account that are outside of a trust's direct control.
Coordination with other national bodies
As in previous surveys, this year we asked trusts to describe how well they thought CQC had coordinated its activity with NHS England and NHS Improvement , other regulators, and national bodies over the last 12 months.
Trusts' opinion was divided as to whether CQC had coordinated its activity effectively at a national level, although more agreed than disagreed (22%/9 fairly effective, 36%/15 neutral, 21%/6 not very effective, 7%/3 not effective at all, 21%/9 don't know), which is similar to responses received in our previous survey (30% agree, 26% disagree, 35% neutral, 9% don't know) (figure 10).
Trusts' opinion in this survey were also largely split as to whether CQC had coordinated its activity effectively at a national level, although more agreed than disagreed (22%/9 fairly effectively, 34%/14 neutral, 12%/5 not very effectively, 5%/2 not effectively at all, 27%/11 don't know). This is better than the previous survey where more respondents felt CQC had not coordinated effectively than those that did (18% agree, 43% neutral, 23% disagree, 15% do not know).
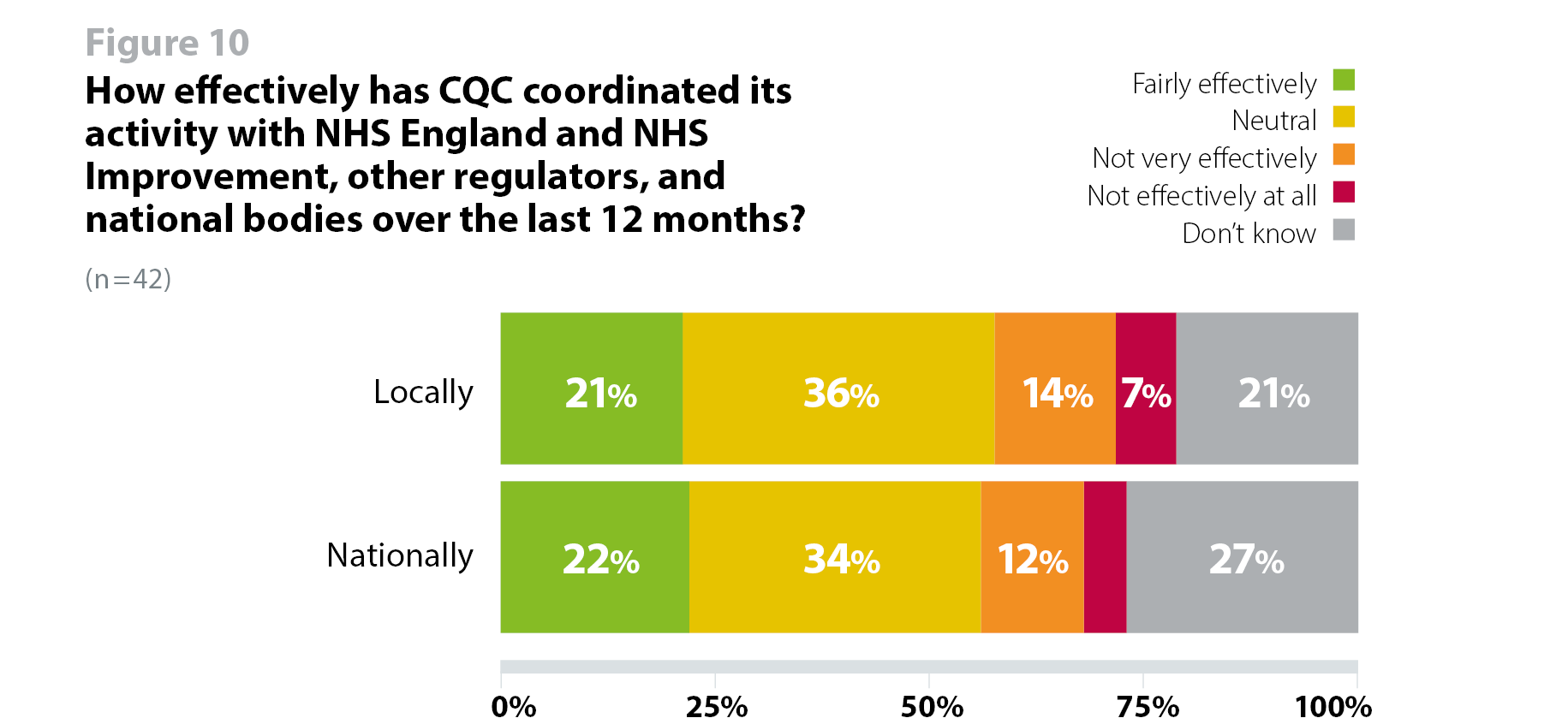
Given the impact of trusts' resource and staff time to respond to regulatory requests, particularly during the COVID-19 pandemic, it is important to coordinate activity effectively to reduce, prioritise and streamline these requests. As most trusts are either uncertain or neutral about the level of coordination CQC has with other regulators and national bodies, this suggests a need for greater alignment.
Both regulation and oversight are out of step and confused. There is, for example, no use of the FT Code of Governance whatsoever since the CQC magicked up the well-led framework.
There needs to be a more streamlined and joined-up process so providers are not being asked for the same things (but often in different formats) from different bodies e.g. commissioners, ICS, NHS England and NHS Improvement and CQC.