
Introduction
Today NHS England published another release of its winter situation reports, offering valuable insight into the activity and performance of trusts across the country during a remarkably cold week.
This week's data (8-14 January) show that seasonal illnesses continue to put pressure on the NHS. The number of patients in hospital with norovirus, flu and Covid-19 remains high, adding to a system challenged by ongoing patient flow issues, and together contributing to high bed occupancy levels.
However, this week's figures again demonstrate the enormous efforts of NHS staff as time lost due to handover delays continues to improve, despite extremely high numbers of patients arriving by ambulance.
Winter situation report (8 – 14 January)
A&E closures & diverts: There were no A&E closures this week. There were 24 A&E diverts this week, four fewer than the week prior but six more than the same week last year.
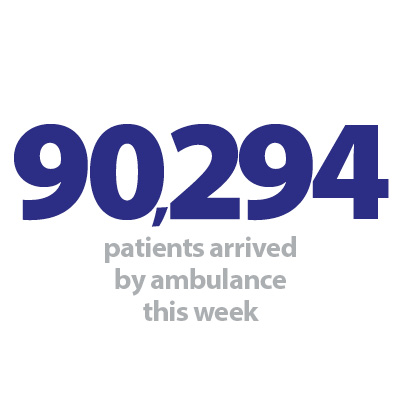
Ambulance arrivals: A total of 90,294 patients arrived by ambulance. A decrease of 1% since last week but up by 25% compared to the same week last year.
Ambulance handovers: 25.7% of ambulance handovers were delayed by 30 minutes or more, down from 30.9% last week but up from 23.4% at the same point last year. 9.1% were delayed by 60 minutes or more. This is down from 13.4% last week but up from 8.9% since the same week last year.
Critical care: Adult critical care bed occupancy is at 79% this week; this is 0.6 percentage points lower than last week (79.6%), and down from 82.6% in the same week last year.
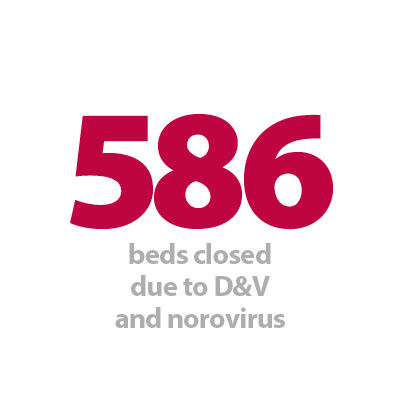
Diarrhoea and vomiting (D&V): The number of beds closed due to D&V and norovirus has increased this week, with an average of 586 closed per day. This is up from 540 last week.
Discharges: There were an average of 23,645 patients each day who no longer met the criteria to reside, an increase of 8.7% (1,897 more). Of these, over half (57.7%, or 13,637) remained in hospital, a slightly larger proportion than the week prior (57.3%) but smaller than the same week last year (59.3%).
Flu: This week the average number of general and acute beds occupied by flu patients each day decreased by 7.3% to 1,335. An average of 81 critical care beds were occupied by flu patients each day this week (24.7% fewer than the week before).
General and acute (G&A) beds: There were an average of 102,784 G&A beds open each day across all acute trusts. On average each day, 75 G&A beds were unavailable and void to non-Covid admissions. Average bed occupancy remains high at 93.3%.
Long stay: The number of patients staying in hospital longer than seven days has decreased since last week (down by 0.8%), but those staying longer than 14 and 21 days has risen by 0.4% and 2% respectively.
Neonatal intensive care beds: For all trusts, bed occupancy has decreased from last week and is at 67.6%; this is down from 68.2% last week. The average number of care beds open is at 1,712, 0.5% lower than last week.
Paediatric intensive care beds: For all trusts, bed occupancy has decreased this week to 72.5%, down from 76.9% last week. The average number of care beds open has remained at a similar level this week at 366, up by 0.1%. The average number of care beds available has risen to 101 (16 more than last week).
Respiratory syncytial virus (RSV): An average of 30 beds were closed this week due to RSV symptoms, down from 54 last week and down by 37% from last year.
Staff absences: There were an average of 49,039 total absences each day this week, of which 5% were Covid-19 related (2,318). The total number of staff absences has decreased slightly from the week before, but the proportion of Covid-19 related absences has remained the same.
Our view
This week saw temperatures plummet across the country, adding further pressure to an already stretched healthcare service. The data depict trends similar to those observed in previous weeks, however we are seeing some improvements, particularly for ambulance crews handing over patients to hospital.
Bed occupancy continues to remain too high at 93% and system wide challenges persist. This week an average of 13,600 patients remained in hospital each day when medically fit to be discharged – the highest figure observed so far this winter – equating to 57.7% of all medically fit patients.
Although this week saw a reduction in the number of patients in hospital with flu for the first time this winter, this is still worryingly high at 1,335, with 81 being in critical care. Furthermore, the number of beds closed due to D&V and norovirus rose again this week and remains above levels seen last year.
More positively, this week saw a considerable reduction in the number of hours lost to ambulance handover delays which were down by over two fifths from the week before. As well as this, there were smaller proportions of handovers delayed by over 30 and 60 minutes compared to last week. The reductions in handover delays were achieved despite over 90,000 patients arriving to hospital by ambulance this week. The demand for ambulances remains high, with arrivals up by a quarter compared to the same time last year: a testament to the incredible efforts of staff working under intense pressure.
Artificial intelligence at the heart of determining care for stroke patients
Jenny Vernel, senior radiographer at Wye Valley NHS Trust, discusses how artificial intelligence (AI) is being used to determine care for stroke patients.
The new RapidAI software which analyses brain images of stroke patients to help determine whether a patient is a suitable candidate for either an operation or drugs to remove a blood clot went live at Hereford County Hospital last month.
The new software does this by automatically identifying the presence of large vessel occlusions – a blockage in one of the main arteries in the brain – to a high accuracy, as well as highlighting any possible intracranial haemorrhages – areas of bleeding – and giving a rating which is used to determine critical changes in the level of blood flow on CT brain scans in acute strokes.
The results and images are immediately available to us within the trust, on our existing Picture Archiving Computer System (PACS) as well as the stroke team and neuroradiologists in Birmingham to assist in rapid assessment of the imaging to decide on the best treatment for the patient in the shortest time possible to maximise the reversal of stroke symptoms and vastly improve patient recovery.
The software assists clinicians to make a quick decision as to whether a patient requires either a thrombectomy (to remove the clot through an operation) or thrombolysis (using drugs to remove the clot).
AI will never replace the clinical expertise that our doctors and consultants have, but harnessing this latest technology is allowing us to make very quick decisions based on the experiences of thousands of other stroke patients.
The system is linked to the Comprehensive Stroke Centre at University Hospitals Birmingham NHS Foundation Trust (University Hospitals Birmingham), meaning that clinical teams and experts at both sites can make faster and more informed clinical decisions – this is essential when treating stroke patients.
Wye Valley NHS Trust is the first trust in the area to roll out RapidAI as a satellite hospital to University Hospitals Birmingham which is acting as the hub for the region.
Niki Williamson, clinical nurse specialist in the trust's stroke services, explains the process of using RapidAI to save vital minutes.
"Patients who present with stroke symptoms and who may be potential candidates for a thrombectomy (mechanical clot removal) have both a plain CT head scan and an angiogram.
"The plain scans look for bleeding, structural and ischaemic changes. The angiogram looks at the blood vessels to see if there are clots present.
"Large clots can potentially be removed by the interventional radiology team at the Queen Elizabeth Hospital Birmingham (QEHB) and at present we wait for a formal report from our radiology team before contacting the stroke team at the QEHB.
"RapidAI indicates possible large clots within 1-2 minutes which means we can contact the team at the QEHB straight away. This means that the appropriate images are reviewed, alongside all the appropriate patient information, medication history etc more quickly.
"If after the review the patient is a candidate for a thrombectomy, we can then transfer the patient to the QEHB for the procedure.
"RapidAI speeds this overall process up – saving at least 60 to 90 vital minutes. Removing a large clot has the potential to vastly reduce disability and is the gold standard treatment for patients who meet the criteria for the procedure.
"We are also very lucky to have support from the air ambulance during daylight hours, this massively reduces transfer time.
"Every minute is important so time saving throughout the pathway is vital in improving patient outcomes."