

Introduction
Today NHS England published another release of its weekly winter situation reports, providing a snapshot of activity and demand in trusts across England for the period 22 – 28 January.
This week's figures remind us of the challenges that the NHS faces throughout winter, as we see a surge in seasonal illnesses, contributing to a further increase to already exceptionally high bed occupancy levels. There remains sustained demand for urgent and emergency care, with large numbers of patients arriving by ambulance compared to last year, which is impacting performance as we also observe increases in handover delays.
This week saw fewer medically fit patients remaining in hospital, demonstrating the efforts of staff working across the health and care sector to discharge these patients in a timely manner.
Winter situation report (22 – 28 January)
A&E closures and diverts: There were no A&E closures this week. There were 28 A&E diverts, the same as the week prior but 18 more than the previous year, an increase of 180%.
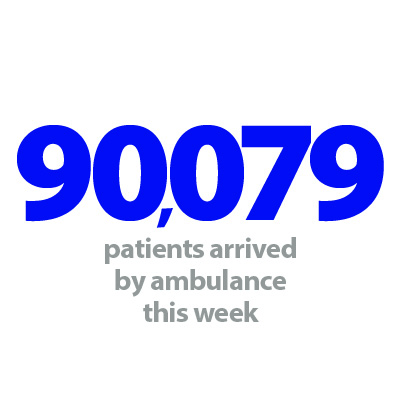
Ambulance arrivals: A total of 90,079 patients arrived by ambulance. A slight decrease of 36 arrivals since last week, but up by 15% compared to the same week last year.
Ambulance handovers: 33.9% of ambulance handovers were delayed by 30 minutes or more, a small increase from last week. At the same time last year this figure was 18.2%. 15.4% of handovers were delayed by 60 minutes or more, compared to 5.6% for the same week last year. The total number of hours lost to handover delays has increased by 16.6% to 33,480 since last week – 3.8 times higher than last year.
Critical care: Adult critical care bed occupancy is at 82.6% this week, up from 80.3% last week and the highest it has been all winter.
Diarrhoea and vomiting (D&V): The number of beds closed due to D&V and norovirus has increased this week, with an average of 798 closed per day. This is up from 549 last week and is the highest it has been so far this winter. Compared to the same week last year, this has increased by 61%.
Discharges: There were an average of 24,281 patients each day who no longer met the criteria to reside, a decrease of 3% (723 less). Of these, over half (56.1%, 13,620) remained in hospital, a smaller proportion than the week prior (57.7%) and also down from this time last year (59.5%).
Flu: This week the average number of general and acute beds occupied by flu patients each day increased by 41% to 2,142, a 78% increase from the same week last year. An average of 84 critical care beds were occupied by flu patients each day this week (29% more than the week before).
General and acute (G&A) beds: There were an average of 103,688 G&A beds open each day across all acute trusts, 2,640 more beds than the same time last year. On average each day, 92 G&A beds were unavailable and void to non-Covid admissions. Total average bed occupancy was at 94.8% this week, the second highest rate for any week this winter, 0.8 percentage points greater than the same week last year.
Long stay: The number of patients staying in hospital longer than seven days has increased since last week (up by 1.2%), but those staying longer than 14 and 21 days has decreased by 0.2% and 1.6% respectively.
Neonatal intensive care beds: For all trusts, bed occupancy has decreased from last week and is at 66.8%; this is down from 68.3% last week. The average number of care beds open is at 1,711, the same level as last week.
Paediatric intensive care beds: For all trusts, bed occupancy has increased this week to 80.8%, up from 77.7% last week. The average number of care beds open has risen this week to 371, up by 1.2%. The average number of care beds available has fallen to 71 (11 fewer than last week).
Respiratory syncytial virus (RSV): An average of 21 beds were closed this week due to RSV symptoms, up from 17 last week but down from 30 last year.
Staff absences: There were an average of 49,212 total absences each day this week, of which 4% were Covid-19 related (2,007). The total number of staff absences has increased from the week before, but the proportion of Covid-19 related absences has remained the same.
Our view
The figures from this week reflect the stark impact of seasonal viruses on the healthcare system. Last winter saw the return of normal flu transmission post-Covid, resulting in an extremely high prevalence compared to the years preceding. However, in the latest week we have seen a spike in the number of beds occupied by flu patients with this figure up 78% from last year – a concerning jump given levels last year. This week's flu report shows the influenza-like illness (ILI) GP consultation rate increased to 9.8 per 100,000 registered population, up from 5.5 last year and also just above levels seen in January 2020 before the pandemic (9). Today's weekly NHS data also demonstrate high levels of D&V and norovirus which have risen considerably from this time last year. Covid-19 figures also remain a cause for concern.
This higher than usual prevalence of seasonal illnesses over winter sits within the wider context of the increased cost of living, which is causing additional challenges. Data published by the Office for National Statistics this week revealed that between 18 October and 1 January, 19% of adults reported being occasionally, hardly ever, or never, able to keep comfortably warm in their home, and a high proportion of these adults also experienced difficulties with paying their energy bills (76%), affording food (14%) or affording housing payments (59%). The rising demand for NHS services is undoubtedly impacted by these issues.
Inside hospitals, bed occupancy levels continue to be worryingly high. Adult critical care bed occupancy reached the highest level so far this winter at 82.6% and is higher than last year. Total general and acute bed occupancy reached the second highest level so far this winter at 94.8%, also up from last week and last year. This is despite the NHS expanding the available capacity by opening 2,640 more beds than last year.
In addition, there are challenges across the urgent care pathway, with demand for ambulances remaining high, and the proportion of handover delays and time lost due to handover delays both greater than this time last year.
Although not covered in this week's data, trust leaders from mental health and community services are also experiencing sector specific challenges. One area of concern for these leaders in particular are the delays facing children and young people in accessing the services they need.
These wide-ranging pressures are compounded by staffing challenges; in the latest week there were over 49,000 staffing absences – an increase from the week before – perhaps not a surprise as community prevalence of flu and other seasonal illness has increased. This is against the backdrop of over 121,000 staff vacancies across the NHS.
South Yorkshire Orthopaedic Surgery Hub to shorten waiting lists for local patients
Richard Parker OBE, chief executive at Doncaster and Bassetlaw Teaching Hospitals NHS Foundation Trust discusses how their new orthopaedic surgery hub is helping to reduce waiting lists and waiting times.
A new service has opened its doors to residents from around South Yorkshire, giving them additional choice in receiving their orthopaedic surgery.
The Dearne Valley-based orthopaedic centre specialises in hip and knee replacement and other similar surgeries, including hand and foot and knee and elbow procedures, for residents within the Bassetlaw, Barnsley, Doncaster and Rotherham areas. Patients can choose to be treated at the specialist centre following consultation with a clinician or choose their usual acute hospital setting.
The Mexborough Elective Orthopaedic Centre of Excellence (MEOC) plays a significant role in reducing orthopaedic waiting lists and waiting times for local people. The service commenced mid-January this year and within the first weeks of operation, 24 patients attended for surgery. In the first year of operation, the centre is expected to undertake around 2,200 orthopaedic procedures, equating to about 40% of the current orthopaedic waiting list.
Currently, the service can treat up to 52 patients a week, operating over a five day a week service. It is anticipated that this number will increase as the service expands to six days a week by mid-2024.
The MEOC, being located within the Montagu Hospital at Mexborough, benefits from the hospital's 'cold site' status, meaning it is not impacted by emergency service provision and the peaks in activity that affect wider acute hospitals. This ensures that the MEOC is ringfenced and protected against the usual cancellations and postponements caused by emergency pressures, particularly in the winter period.
Utilising best practices, the MEOC aims to minimise on-the-day cancellations through consistent and coordinated pre-assessment processes, eliminating all preventable cancellations and has also implemented the Getting it Right First Time care pathways with standardised peri-operative care and pre-assessment co-designed with clinicians to reflect management of care between hosts sites and MEOC.
Gavin Boyle, chief executive of the South Yorkshire Integrated Care Board, said: "The MEOC is a great example of partnership working between hospitals in South Yorkshire.
"By working together and working differently, we can better meet the orthopaedic healthcare needs of our community. This centre will play an important part in helping us to reduce waiting times for surgery and we know how important this is for local people.
"We are committed to providing the best possible care for our communities, and the MEOC is a practical example of how we work together as an integrated care system to do this."
The MEOC is operated between Doncaster and Bassetlaw Teaching Hospitals, Barnsley Hospital NHS Foundation Trust and The Rotherham NHS Foundation Trust, costing £14.9m. The project started its planning phase in 2021, completed in December 2023, with the first patients admitted for surgery on 15 January 2024.
For more information about the MEOC, including a tour of the centre, please visit: www.dbth.nhs.uk/meoc/