

The data in the second week of the winter sitreps paints a slightly more positive picture than expected. Despite showing high demand and sustained high occupancy levels which are a continued concern, there are some positive nuggets compared to performance at the same time last year.
- 93.4% of general and acute beds were occupied, a fall from last week.
- There were 30 A&E diverts this week – exactly the same number as last year.
- A reduction in ambulance handover delays compared to last year.
- Compared to last year there has been a 65% reduction in the number of beds closed as a result of diarrhoea and vomiting or norovirus.
- Length of stay as fallen from last week and in comparison to last year there has been a 13% reduction in the number of patients staying over 21 days.
- The number of patients waiting over seven days has also reduced by 8% compared to the same week last year.
- Trusts have 23% fewer escalation beds open than last year and fewer beds than last week.
However, the key measure that really indicates local systems are in a slightly stronger position than we may have expected are the improvements in handover delays. This time last year 15% of patients that were delayed when being handed over to a hospital had to wait for 30 minutes or more. This has fallen to 9.7% - and is also lower than last week which is a positive trend. This metric, along with the improvements in length of stay and bed occupancy, indicates that systems are working together to unblock the barriers that often stop patients being discharged home or to the right setting.
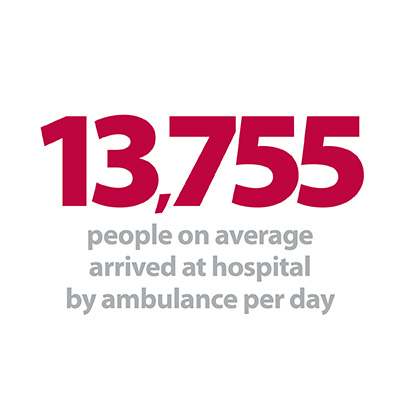
We know that demand for urgent and emergency care remains very high. In particular the data shows that ambulance services are experiencing an increase in activity. This week, 13,755 people on average arrived at hospital by ambulance each day – an additional 170 patients a day compared to last year when we know it was colder and the flu season had begun to put more pressure on services.
This week our contribution from South Central Ambulance Service shows exactly how systems are working together to ensure frail and older people avoid being admitted into hospital and are treated in the most appropriate setting.
So far, the flu season and norovirus outbreaks are having considerably less impact than this time last year. The ability, capacity and resilience of systems to respond to any further surges in demand will remain the worry for both system leaders and frontline staff alike over the Christmas period.
Length of stay as fallen from last week and in comparison to last year there has been a 13% reduction in the number of patients staying over 21 days.
Frailty support team transforms elderly patient care
A partnership between South Central Ambulance Service NHS Foundation Trust (SCAS), Southern Health NHS Foundation Trust, West Hampshire CCG, Hampshire County Council, New Forest GP practices and the Milford-on-Sea and Totton League of Friends is helping ensure more elderly patients can be provided with treatment and care in their own homes.
It’s great that we are living longer but the bad news is that many of us spend our latter years coping with ill-health and associated care needs. We also have increasing numbers of people living with long term conditions and frailty, putting them at risk of repeated hospital admissions which can undermine their capacity to live independently and well. Time and time again studies have shown that most people want to live well at home, on their own terms, for as long as possible, so what can we do to make that the reality for more of us?
Charity Director, Age UK
Since launching in late August, the frailty support service has already helped healthcare professionals to treat on average 80-90 patients a month (approx. 1,300 referrals from primary care and SCAS since the service launched). Ensuring that more frail elderly patients do not need to be taken into hospital reduces pressure on other parts of the NHS, particularly acute hospitals, all year round and is particularly important at a time of peak winter demand.
Sometimes, hospital admission is unavoidable particularly if there are suspected fractures following a fall or a suspected severe underlying illness. But any attempts to keep this group of patients out of hospital are valuable as their admission can lead to risks of muscle wastage from lack of movement and developing hospital acquired infections. These are all factors that increase the chances of frail elderly patients being readmitted to hospital either from falling again, or falling ill, shortly after having been discharged.
The frailty support scheme is a really positive example of how NHS organisations can work together to improve the patient experience through supporting them with the appropriate treatment at source.
Demand Practitioner, South Central Ambulance Service
Specially commissioned cars are used by the frailty support team, with each car staffed by an experienced SCAS ambulance technician, contracted to work in partnership with Southern Health. The cars have diagnostic equipment as well as cardiac monitoring, defibrillator, lifting cushions and other emergency response equipment to enable responders to perform a thorough triage assessment.
When visiting a patient at home, the frailty support team can spend more one-to-one time capturing a holistic view of the person’s health and social care needs. With more personal and dedicated time for each patient, it is possible to diagnose any potentially acutely unwell patients, provide medical intervention if needed and also undertake further assessments and recommendations, such as creating or revising a personal care plan. These visits also reduce the need for the patient to visit their own GP or request help from the ambulance service.
The frailty support scheme is a really positive example of how NHS organisations can work together to improve the patient experience through supporting them with the appropriate treatment at source. The service combines the right clinicians and resources to better manage patients in the community or direct them to the appropriate pathway of care.
Winter preparations by trusts having positive impact but pressure points remain
Responding to the latest weekly winter performance data from NHS England, NHS Providers director of policy and strategy, Miriam Deakin, said:
"Record levels of demand for urgent and emergency care going into December have already put trusts under tremendous pressure so it is a testament to the hard work and preparations of trusts and staff that pressures at the frontline have levelled off from last week.
"Although bed occupancy levels remain very high the number of escalation beds opened and the number of beds filled has fallen from last week and is better than this time last year. The work trusts have undertaken to reduce the number of patients staying in hospital longer than 21 days has also really paid off.
"Despite this trusts are still experiencing real pressure points. Demand for ambulance services remains very high with over 1,000 more arrivals by ambulance in one week than the same point last December.
"As many people head into a Christmas break, we must thank the thousands of NHS staff who will be working extremely hard around the clock over the festive period to provide quality care to those that need it."