

The winter reporting period closes this week with the final sitreps data showing continued high levels of demand across the system. A theme throughout the winter has been the ability of trusts to meet these challenges, and this remains the case as we enter spring in a stronger position than last year.
Key indicators in week 13 include:
- Bed occupancy fell slightly by 0.1% this week to 93.8%, which is 1.4% lower than the same point last year.
- There were an average of 3,374 escalation beds open each day this week, 6.3% fewer than last week and 26% fewer than the same point last year.
- Total beds open fell by 0.2% since last week and is 0.5% lower than the same point last year.
- Beds closed with diarrhoea and vomiting and norovirus has increased by 23% since last week to 684. This is 9% lower than at the same point last year.
- There were 18 A&E diverts this week, one more than last week – but nearly half the number at the same point last year.
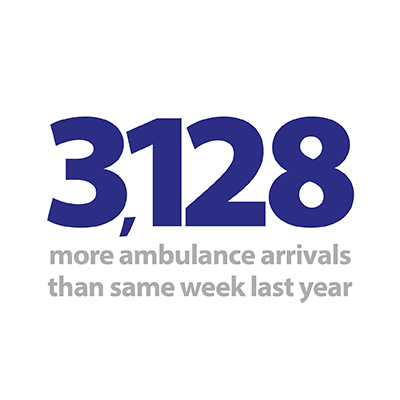
- The number of ambulance arrivals decreased by 1.4% this week to 95,289 (1,362 fewer than last week). The number of arrivals remains 3.4% higher than the same point last year.
- The proportion of ambulance arrivals waiting more than 30 minutes and more than 60 minutes decreased very slightly this week to 10.6% and 1.8% respectively. Compared to the same point last year, 1.1% fewer people waited longer than 30 minutes and 1% fewer waited longer than 60 minutes.
- A&E closures – zero.
- Adult critical care bed occupancy has decreased by 0.9% to 82.5%. Paediatric intensive care bed occupancy decreased by 2.1% this week to 75.2%. Neonatal intensive care occupancy has decreased this week by 0.7% to 67.7%.
While bed occupancy has fallen to the lowest rate since the start of the year, hospitals will still feel very busy despite the changing seasons. Staff will remember the pressures brought on by the cold conditions and outbreaks of flu and norovirus last winter, and while conditions have been milder this winter, demand has remained extremely high.
A theme throughout the winter has been the ability of trusts to meet these challenges, and this remains the case as we enter spring in a stronger position than last year.
However, the plans trusts have put in place are having a positive effect, reflected in the fact the number of escalation beds open fell by a significant amount this week, and now sits 26% lower than the same point last year. There have been fewer patients staying longer than 7 and 21 days every week this winter compared to the equivalent point last year, and this week the pattern continues with 8.7% and 10.2% fewer patients staying longer than 7 and 21 days respectively.
High numbers of ambulance arrivals have been seen throughout the winter, and while this week sees a small drop from the previous week, the total remains 3.4% above the number of arrivals at the same point last year. This works out to be almost 450 additional arrivals per day, so it is a credit to trusts that the proportion of arrivals experiencing handover delays sits considerably lower than a year ago.
This week our feature blog is written by Lisa Ward, head of communications at NHS Providers, giving reflections of the winter campaign and highlighting key contributions from staff on the ground over the previous 13 weeks. While the improvements trusts have made to prepare for winter and meet the challenges on a daily basis are nothing short of remarkable, the real story of winter is that services remain incredibly stretched, and NHS staff face comparable pressure throughout the year to meet high levels of demand.
For a more detailed breakdown of this week’s winter sitrep data please see our summary dashboard.
To the outside world it may feel like the NHS has avoided a winter crisis this year, but is that really the case?
For the last 13 weeks we have been analysing and reporting on the weekly winter sit-rep statistics through our NHS winter watch series. Here, we set out the story of winter from our members’ perspective.
The story so far
There is no doubt from what we have heard from trusts that the NHS has worked incredibly hard to plan for and deliver care for patients over traditionally the busiest period for the NHS. But demand for urgent and emergency care is as high as its ever been and, in particular, the number of ambulances conveying patients to A&E has dramatically increased. The media, politicians and the public have been distracted by the countdown to Brexit, but frontline staff working in our member trusts have pulled out all the stops and yet again cared for increasing numbers of patients.
Demand for urgent and emergency care is as high as its ever been and, in particular, the number of ambulances conveying patients to A&E has dramatically increased.
Weekly sitrep reporting began in the first week of December, but the NHS entered winter in a challenging position after a busy summer contending with an unexpected heat wave. In November attendances increased and performance against the A&E four hour waiting time target fell to 87.6% - the lowest for that month since the data collection began. But trusts saw 1,000 additional patients within four hours every day in November compared to 2017 and emergency admissions in October and November were at record levels. By the second week of January (normally when the post festive period pressure hits), bed occupancy had crept up to 94.7% and the number of escalation beds open increased by 18% from the previous week, although this was still 22% lower than the level seen in the same week last year suggesting trusts were coping better and managing flow through hospitals effectively.
By the first week of February, it was clear that some of the most acute pressure was being felt by the ambulance service. 7,056 more ambulances arrived at A&E departments across the country than over the same week last year, which on average equates to an additional 53 ambulances a week arriving at each of the 134 trusts with a type 1 A&E department – not an insignificant amount of additional work when bed occupancy is so high and there are staffing challenges.
This trend of high numbers of ambulance arrivals continued to the end of February but again trusts and the ambulance service and hospitals demonstrated how they have risen to the challenge of improving patient flow with fewer handover delays across the vast majority of winter when compared to last year.
Trusts saw 1,000 additional patients within four hours every day in November compared to 2017 and emergency admissions in October and November were at record levels.
Working in partnership to deliver for patients
This year trusts have been keen to share more examples of their work within health and social care to breakdown some of the longstanding barriers to integration and tackle winter pressures.
One key example from our winter blog series was the Royal Bournemouth and Christchurch Hospitals (RBCH) and Dorset Healthcare University NHS Foundation Trusts successfully collaborating as part of system working under the banner of ‘One Dorset’. The two trusts are working closely to ensure that patients can be discharged when they are medically fit with the right support in place in the community. RBCH has a community ward on site to provide rehabilitation before being discharged home or to another community facility. Preventing hospital admissions is also a priority and senior clinicians triage patients quickly and, if possible, refer them to facilities in the community. Dorset Healthcare has community matrons and intermediate care therapists based in the emergency department to manage patients who can be cared for by the integrated hub in Bournemouth or co-located teams in Christchurch.
Preventing hospital admissions is also a priority and senior clinicians triage patients quickly and, if possible, refer them to facilities in the community.
Richard Jenkins chief executive at Barnsley Hospital NHS Foundation Trust described how they had spent a year working with staff and redesigning their whole approach to the emergency care pathway and winter preparedness.
"The improvement work was extensive and our drive to do better this year came from the poor experience our patients and staff had in December and January last winter and a sense of 'never again'.
"An important part of the work was 'hearts and minds' – we held lots of open meetings with staff to talk through some of the key proposed work and why we were doing it. We were supported in the work by our partners in Barnsley (South West Yorkshire Partnership NHS Foundation Trust, Barnsley Metropolitan Borough Council, the local GP federation and Barnsley Clinical Commissioning Group) and the Improvement Academy."
This year trusts have been keen to share more examples of their work within health and social care to breakdown some of the longstanding barriers to integration and tackle winter pressures.
The trust saw a progressive improvement in four-hour performance through the first half of 2018 and achieved the best performance in the country for September. They went into winter consistently meeting the standard and continued through to Christmas.
Planning was also key for Sherwood Forest Hospitals NHS Foundation Trust. Chief operating officer Simon Barton led a process he described as "preparing, enacting, reacting".
"This has meant that for December we were at 94.9% (and year to date we are still above 95%). While not meeting the target, it was an improvement on our performance in December 2017 (86.4%). Our admissions via ED have been high compared to last year – 86 compared to 83 per day in December 2017. However, length of stay has been lower which has enabled us to cope better. We feel we are working better with partner organisations and all this means a better experience for some of the sickest patients we see."
Another of our contributors to winter watch was Sam Allen chief executive of Sussex Partnership NHS Foundation Trust. She highlighted that there is always more focus on performance during winter and the effort that goes into planning for it across community and mental health services, but the big challenge is to make sure this degree of system-wide focus exists all year round.
"This is crucial given the sustained demand upon mental health services we’re starting to see all year round. We’re moving in the right direction on this in my local area, and I value the shared commitment to mental health from our partners.
"The work we have to do includes determining if we have the right level of capacity, in the right place, in our mental health hospitals as well as our acute hospitals. Bed occupancy across many mental health services runs close to, or at, 100%. This means it can be challenging to arrange timely access to hospital care for people as close as home to possible.”
Real story of winter shows that health and care services remain at full stretch
Responding to the final winter sitrep figures from NHS England, the director of policy and strategy at NHS Providers, Miriam Deakin said:
"Health and care services have coped well compared to last winter, but we must not fall into the trap of normalising the extreme pressures facing the service.
"Due to sustained high levels of demand bed occupancy for this final week of winter performance data is at 93.8%. This is still higher than trusts would like and only just under the levels we saw last year during much colder weather and challenging conditions.
"Improvements to winter preparations and the plans put in place by trusts including the use of walk-in centres and efforts to reduce the length of stay have played a key part in providing the right level of care to patients as quickly as possible."
Health and care services have coped well compared to last winter, but we must not fall into the trap of normalising the extreme pressures facing the service.
Director of policy and strategy
"It has also been striking how many more patients have been arriving at hospital by ambulance this winter. These consistently high numbers are a sign of growing care needs resulting in the need for emergency care.
"Improvements in how health and care systems have helped patients to return home more promptly when they are well enough is shown by the significant drop in the number of people staying in hospital for over three weeks.
"But despite the efforts trusts and their staff have made, and the improvements they have delivered, the real story of winter is that health and care services remain stretched and NHS staff are now working incredibly hard throughout the year to meet high levels of demand."
There is still time for additional pressure to hit, and in the last week the number of beds closed due to D&V and norovirus increased by 23%.
Where do we go from here?
These are obviously fantastic examples of planning ahead and working across boundaries and are clearly better for patients, but it still doesn’t get away from the fact that the NHS is under more pressure than it’s ever been. Performance against the four-hour A&E standard hit a record low in January 2019 at 84.4% and the lowest individual trust performance was down to 62.7%. But to put this in context, this is just 0.9% worse than last year and with a 6% increase in A&E attendances. Trusts have seen 111,549 more patients come through A&E and 37,719 more emergency admissions compared to January 2018.
This is largely down to hardworking frontline staff who have focused on keeping patients safe and looking for ways they can ensure they can rise to the challenge of ever increasing demand.
The weekly reporting may have ended, but this does not mean that the ‘difficult’ winter period has ended for the NHS. Demand is still high with nearly 3,500 escalation beds still open and ambulance arrivals remaining high compared to last year. But despite months and months of continued pressure, trusts are continuing to rise to the challenge with 8.7% fewer patients staying over 7 days and 10.2% fewer patients staying over 21 days compared to the same time last year.
There is still time for additional pressure to hit, and in the last week the number of beds closed due to D&V and norovirus increased by 23%.
It is clear from what we have heard anecdotally from our members that the feeling is that on the whole services have coped better and planning, partnership and system working have been key to that. What we need to see in the year ahead is more recognition of what trusts and partners have done to prepare and, through the work to deliver the long term plan, sustainable solutions to rising levels of demand across community, mental health and hospital services.