
With bright sunshine, warmer temperatures and daffodils appearing - it’d be fair to assume that we might be over the hump of winter. So does the NHS England winter sitrep data this week show any signs of reprieve for NHS staff?
Despite a much milder winter and flu not being a feature in the way it was last year, demand for NHS services continues to increase yet again this year.
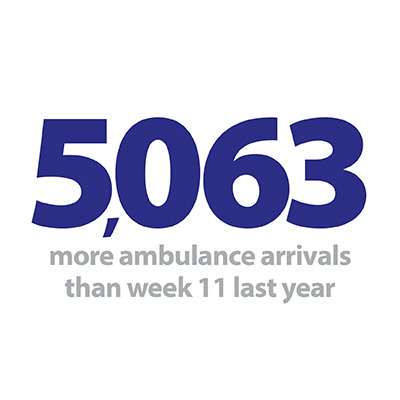
This week, 5,063 more ambulances arrived at A&E departments across the country than over the same week last year. On average, this equates to an additional 38 ambulances a week arriving at each of the 134 trusts with a type 1 A&E department – not an insignificant amount of additional work when bed occupancy is so high and when we know there are staffing challenges.
Bed occupancy has fallen slightly from last week but holding at 94.5%. Acute hospitals are running very hot – meaning sites are extremely full with little available capacity for new patients to be admitted.
Despite a much milder winter and flu not being a feature in the way it was last year, demand for NHS services continues to increase yet again this year.
But despite these indicators of pressure across systems there have been a number of areas where performance has improved compared to last year:
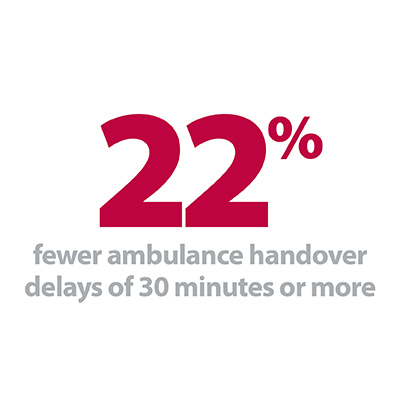
- Despite the increase in demand for ambulances handover delays are better than last week and significantly better than last year. The proportion of ambulance handover delays of 30 minutes or more was 22% lower than the same week last year. The number of delays of 60 mins or more is down 13% on last year.
- Drives to reduce length of stay remains positive, with the number of patients staying longer than seven and 21 days down compared to the same time last year. The number of patients staying longer than 7 days has fallen by 6% and those staying 21 days or more has decreased by 13%.
- There were 17 A&E diverts this week, down by a third compared to last week and 26% lower than the same week last year.
All these indicators point to the service making improvements in areas such as increasing morning discharges, reducing length of stay, providing assisted discharge services and working better with partners in social care to avoid delayed transfers of care. These improvements are the result of the hard work trusts put in to prepare for winter, the changes they have made to implement new processes and the relationships they have built within systems and across sectors to manage patient flow.
These improvements are the result of the hard work trusts put in to prepare for winter, the changes they have made to implement new processes and the relationships they have built within systems and across sectors to manage patient flow.
For example, this week our feature blog highlights the key role that voluntary and third sector organisations can play in working with the NHS and helping improve patient experience. The British Red Cross offers a range of services for the NHS, and below, Mike Adamson, British Red Cross chief executive explains why it is so important to get the discharge process right for patients to ensure they do not become unwell again and prevent readmission to hospital.
Overall, the data this week shows the NHS running at nearly full capacity but indicates that the service is able to run more efficiently than it was able to last year. Without a late surge in flu or another ‘beast from the east’ weather moment it is unlikely that NHS England will continue to publish the sitreps into March as they did last year. But NHS staff will still be taking things day by day and hoping that the seasonal spike may start to ease as spring begins.
For a more detailed breakdown of this week’s winter sitrep data please see our summary dashboard.
Care beyond the hospital doors
Your patient has left hospital – what next?
By Mike Adamson, British Red Cross chief executive
For hospital staff, sending someone home is usually viewed positively. The patient has been successfully treated, and now their bed is free for the next patient who needs it.
But there’s a lot more behind each patient’s situation. Some patients may be medically fit, but have other needs that either prevent them from going home, or mean they struggle when they get there. Others are initially eager to leave hospital but find they feel differently once they get through their front door.
The pressure to manage patient flow is real, and complicated by both systemic and human factors. Teams struggle to communicate effectively. Patients keen to get home may over-estimate their ability to cope, or not want to be a burden.
Navigating hospital discharge for vulnerable patients is tricky. It’s something British Red Cross knows about – we work in over 100 hospitals providing assisted discharge services from wards and around twenty emergency departments too. This winter we’ve provided 40 extra or scaled-up projects to take some pressure off hospitals. Our winter pressures work has expanded to include mobility aids pop-up services with several Trusts, and pilot projects to help ‘longer length of stay’ patients. We hear from ward staff and OTs these services give them peace of mind – we are their eyes and ears beyond the hospital doors, able to check people’s home environments and make sure they get the extra help they need to adjust and recover.
The pressure to manage patient flow is real, and complicated by both systemic and human factors. Teams struggle to communicate effectively. Patients keen to get home may over-estimate their ability to cope, or not want to be a burden. Patients often want to recover at home and evidence shows it can be better than a stay in hospital. But when the transition from hospital to home doesn’t work, it can affect recovery, wellbeing and the person's ability to live independently.
Patients often want to recover at home and evidence shows it can be better than a stay in hospital. But when the transition from hospital to home doesn’t work, it can affect recovery, wellbeing and the person's ability to live independently.
Last week, I was joined by leaders in the sector at our first Health and Social Care Leaders' Summit, to discuss how we best support patients through the discharge process. We launched our new report Home to the Unknown: Getting hospital discharge right. This research looks at discharge processes, the views of staff and policy experts, and the experiences of patients themselves back in their home environment. You can hear some of those patient reflections in this powerful video, which illustrates a range of issues, from people not understanding their diagnosis or paperwork, through to isolation, loss of confidence, and challenges of the physical environment they’re returning home to.
Kev, now back at home after four weeks in hospital after a stroke, explains how the transition affected him:

“When you come out of hospital, you get back to your flat, and you’re different. Mentally you’re different because your life is different, your life has changed. So you’ve got to do things in a different way.”
‘Doing things in a different way’ is a good way to address this issue. When discharge and the transition process works well, it can make all the difference to a patient’s recovery. But where it doesn’t, we need to do things differently. There are good initiatives out there already. Sometimes it’s hard to make that culture change happen and follow through with good ideas. The voluntary sector could take on more of this non-clinical work to smooth patients’ journey through the system.
“When you come out of hospital, you get back to your flat, and you’re different. Mentally you’re different because your life is different, your life has changed. So you’ve got to do things in a different way.”
Health and social care staff do an incredible job in difficult circumstances. Our report suggests some simple, low-cost improvements that pay attention to the joins in the system:
- ensuring clinical accountability for transitions between teams, so patient care doesn't fall through the gaps
- supporting patients and clinical teams by having a named non-clinical person supporting patients through hospital and first days at home
- building in a 5-part independence check to all discharge processes.
Working together, with some small changes, we can make all the difference to the wellbeing and recovery of patients – both during the winter, and all year round.
Health and care system running hot but trusts managing relentless pressure
Responding to the latest weekly winter performance data from NHS England, the head of policy at NHS Providers, Amber Jabbal said:
“This week’s figures show that the health and care system is still running hot with very high demand for emergency and urgent care, but trusts are continuing to manage the relentless pressure.
“The number of beds in use across the health and care system remains very high. We shouldn’t underestimate how busy it currently is on the frontline and the dedication of NHS staff.
“The number of beds in use across the health and care system remains very high. We shouldn’t underestimate how busy it currently is on the frontline and the dedication of NHS staff.
“Ambulance services are bringing more people requiring treatment to hospitals this winter, but staff are working hard to reduce the time it takes to handover patients to hospitals with success in reducing delays.”
“The reduction in the length of time a patient stays in hospital is a result of partners across the health and care system working closer together to treat patients in the most appropriate setting possible.”