Culture and morale
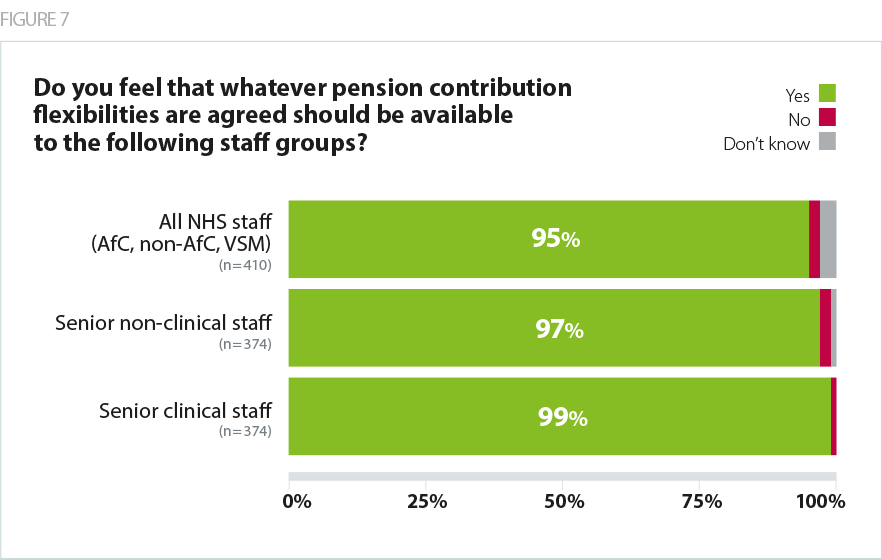
Respondents were almost unanimous in the view that senior non-clinical staff should be eligible for pension contribution flexibilities (97%). Almost as many (95%) felt that the flexibilities should be available to all NHS staff including AfC, VSM and other non-AfC staff groups.
Respondents were also unequivocal in their concern at the equity implications of offering pensions flexibilities only to clinicians in active clinical roles, particularly for its impact on culture and morale across the workforce. Nine in ten respondents (91%) said that they or their boards are concerned about the impact on culture and morale of offering differential arrangements to different groups of staff.
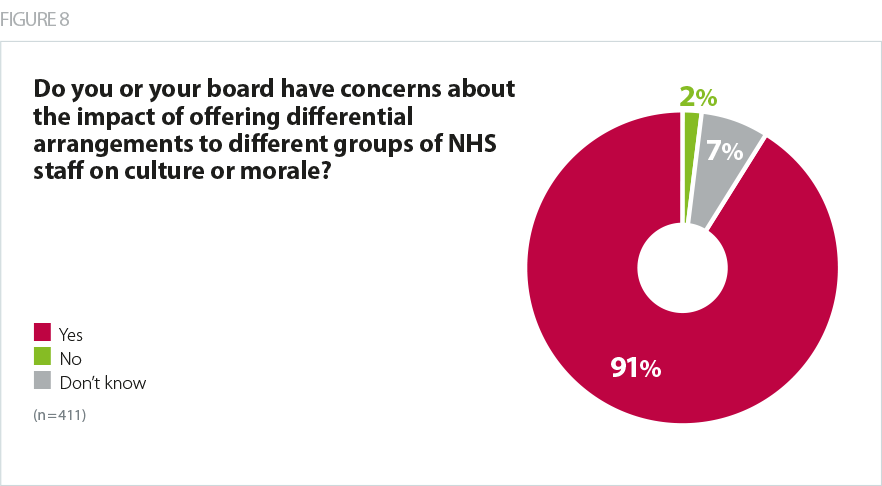
Trust leaders are responsible for instilling the core NHS values of equality and fairness within their organisations, while playing a critical role in the development of system working. Respondents felt strongly that offering differential arrangements to groups of staff based on their specific role runs counter to these efforts.
Trust leaders also expressed concern that a loss of morale may diminish the willingness of staff across the sector to offer up additional discretionary effort to sustain stretched services, while a divisive policy which favours one group over another may undermine individual relationships and general cohesion within teams, with a knock-on impact on the effective delivery of services.
Impact on frontline services
Respondents strongly expressed the view that the expertise of senior leaders enables clinicians to deliver high quality care in well designed services, in well supported teams, and with the right facilities they need to do their jobs well.
Non-clinical managers provide a hugely valuable service in the day to day operation of patient services – whether corporate services like HR or finance, or operational managers who directly support clinical activities. Hospitals and community services can't function without non-clinical managers and staff working as part of a single team with clinical colleagues. This solution creates a dividing line in that team that does not fairly recognise the 24/7 contribution of those non-clinical staff.
Combined acute and community trust
While the link between consultants' working hours and clinical capacity is more overt and has been widely reported, there is also a link between the roles of other directors and managers and team productivity, quality of care and the effectiveness of the leadership. The leadership and governance at trust board and executive level plays a central role in setting an organisation's culture, vision and strategy, approach to management at all levels, recruitment and staff wellbeing. All of these factors underpin the provision of high quality frontline care with substantial implications for patient outcomes.
It is the efficiency and affordability of [frontline] services that suffers as the work done to make sure they are being managed effectively is compromised.
Combined acute and community trust
Positive work atmosphere and visible leadership are key ingredients for staff recruitment and retention. All leaders face being penalised if they take on more senior roles, or responsibilities. This leads to more vacancies, interim/agency working etc, which is corrosive for well led organisations. Poorly led organisations have higher mortality rates. Senior managers do on-call, and work seven days a week. Vacancies lead to operational decisions, especially around emergency care, becoming ever more difficult.
Acute trust
Not only is there potential for attrition of senior leaders in the provider sector if these roles continue to carry a risk of incurring large and unpredictable tax bills, but there is also evidence that difficulties are beginning to emerge in encouraging new staff to take up these challenging and important roles where vacancies do arise. Trust leaders raised concerns that this is leading to difficulties filling managerial on-call rotas, driving up agency costs and destabilising transformation efforts.
Others noted that, as additional hours worked among managers are more likely to be unpaid, a loss of discretionary effort would, while not measurable in a number of additional sessions or 'programmed activities', equate to a loss of management capacity across services which rely on leadership to run smoothly. Some have already seen this in the form of managers asking for time off in lieu for additional hours worked, where previously they did not.
My concern is that if we don't make the pension flexibilities applicable to all, we run the risk of a very unequal set of arrangements within the workforce which could give rise to tensions and feelings of resentment between clinicians and non-clinicians which in turn could impact on the delivery of front line services. For example, there may be some non-clinical posts that can't be filled as they are unattractive to those who have the skills and experience but a large pension pot. In turn, these posts may be filled by less experienced candidates who perform less effectively and therefore the delivery of services is affected.
Acute specialist trust
Many senior trust leaders have decades of experience of working in the NHS. Recruiting to vacant posts on a 'like for like' basis if they leave for the private sector or retire early is challenging, particularly in light of the evidence that fewer staff are willing to accept promotions into these challenging roles due to the risk of receiving large tax bills. It also costs the NHS many years of investment in their skills and expertise during long periods of NHS service, and increased board turnover leads to a loss of organisational memory.
Stability of leadership is essential to the efforts of trusts to deliver high quality care in a challenging environment, and there is a clear link between the quality of leadership in a trust and the quality of the care that trust provides.