Capacity to meet demand

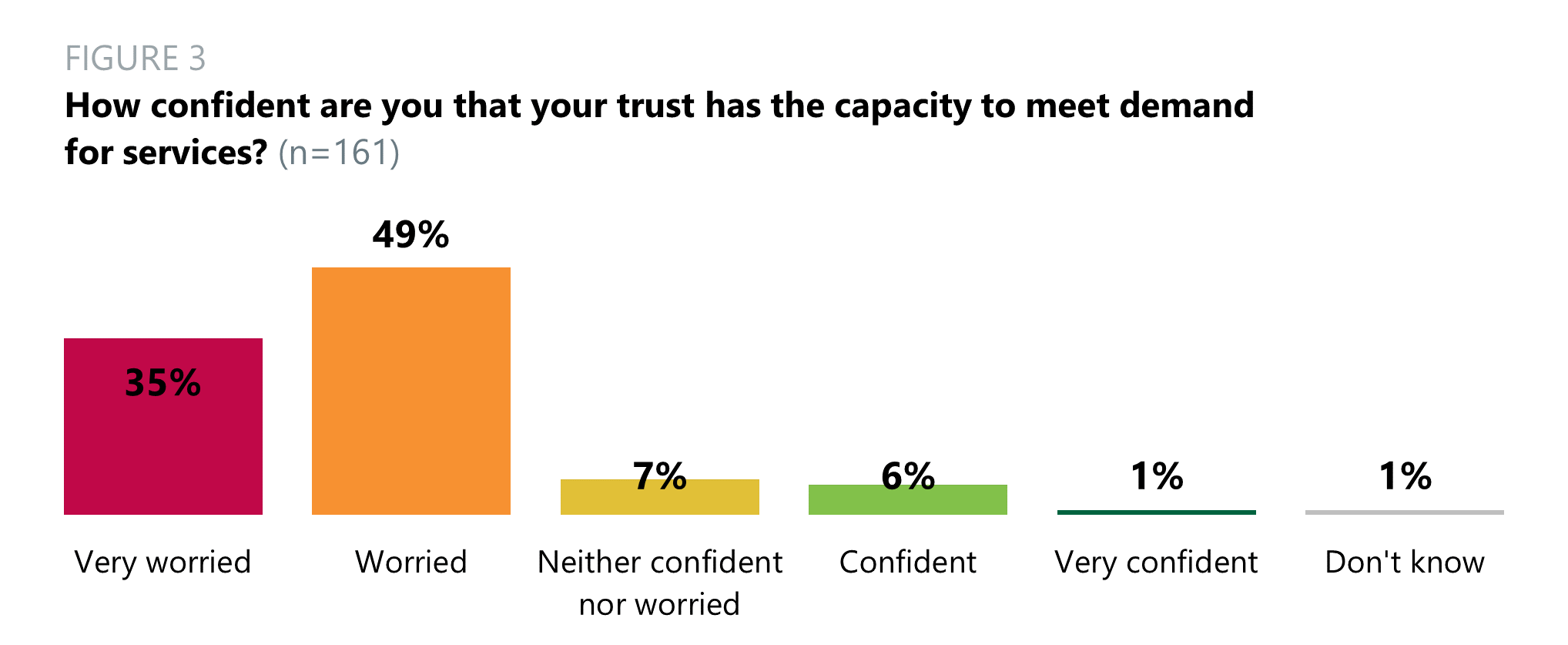
- 84% of trust leaders were very worried (35%) or worried (49%) about their trusts having the capacity to meet demand for services. 7% were neither confident nor worried, 6% were confident, 1% were very confident and 1% did not know. Last year, 64% of trust leaders were very worried (11%) or worried (53%).
- Across different trust types, the two trust leaders from ambulance trusts (100%) were very worried their trust has the capacity to meet demand for services. All (100%) trust leaders from mental health/learning disability trusts were very worried (47%) or worried (53%). The more confident trust type leaders were in acute specialist trusts, of which 58% of their leaders were very worried or worried.
In the comments, trust leaders expressed concerns regarding increasing demand in the urgent and emergency care pathway, staff shortages and the impact of COVID-19 in providing elective care.
“We are experiencing an unprecedented demand in the urgent and emergency care pathway. This is not sustainable with the current staffing model. A revised staffing model is not achievable in the current funding model.”
“Worried about capacity to meet emergency and critical care activity and ongoing impact that has on workforce and ability to deliver elective programme.”
Quality of healthcare provided by your local area now and in the future
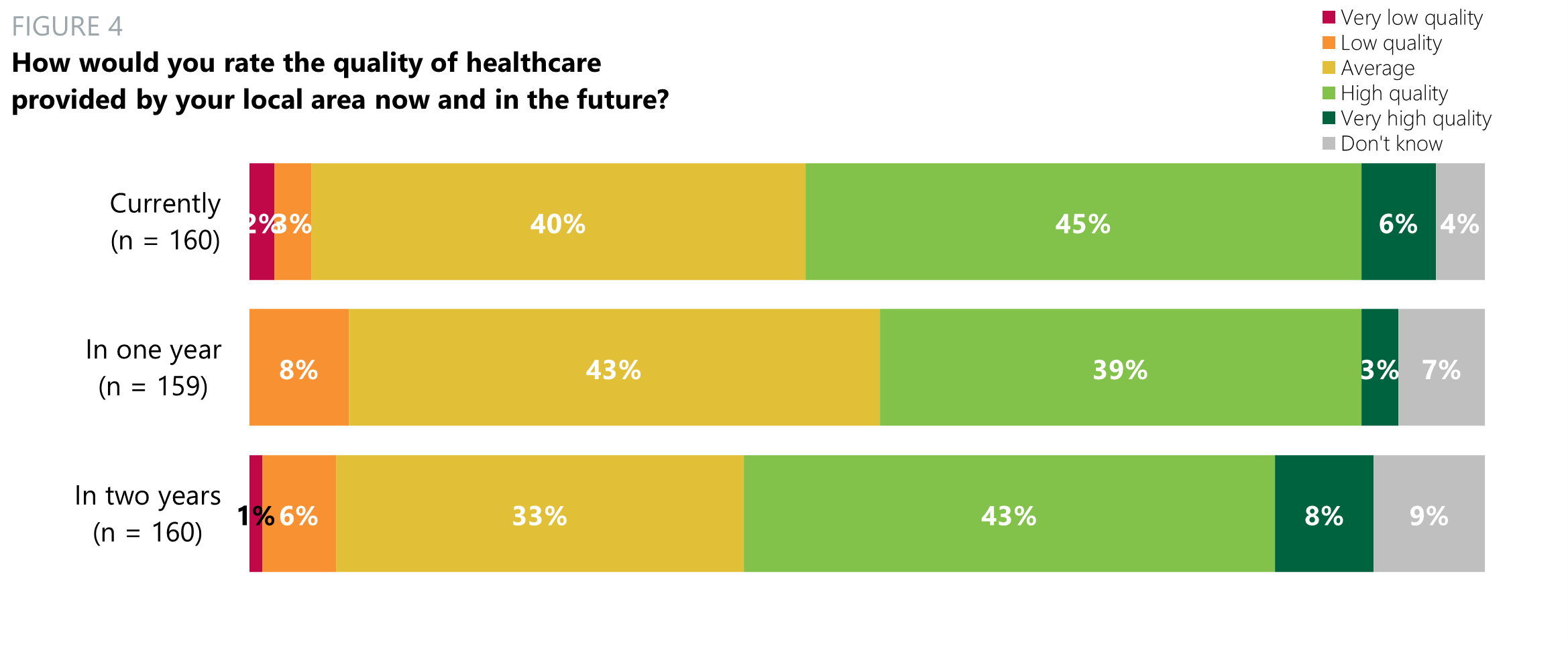
- Just over half (51%) of trust leaders rated the current quality of healthcare provided by their local area as very high (6%) or high (45%). 40% rated it as average, 3% as low quality and 2% as very low quality. 4% did not know.
- Under half (42%) of trust leaders predicted that the quality of healthcare provided by their local area in the coming year would be very high (3%) or high (39%). 43% said it would be average and 8% low quality. 7% did not know.
- Just over half (51%) of trust leaders predicted that the quality of healthcare provided by their local area in the coming two years would be very high (8%) or high (43%). 33% rated it as average, 6% as low and 1% as very low. 9% did not know.
In the comments, trust leaders had mixed views when rating the quality of healthcare provided in their local area now and in the future. Some were unsure, stating it was dependent on the type of service and that too many variables were involved. Respondents who believed the quality of healthcare would decline raised concerns around staffing issues. Those who believed it would remain the same highlighted how they were striving to deliver high quality care, and issues with capacity rather than quality. Respondents also relayed concerns over the high waiting lists for elective care.
“We will continue to deliver high quality care. We know that the quality isn't currently as good as we would like it to be and we are working hard to improve this. The capacity is the issue, not the quality.”
Right numbers, quality and mix of staff
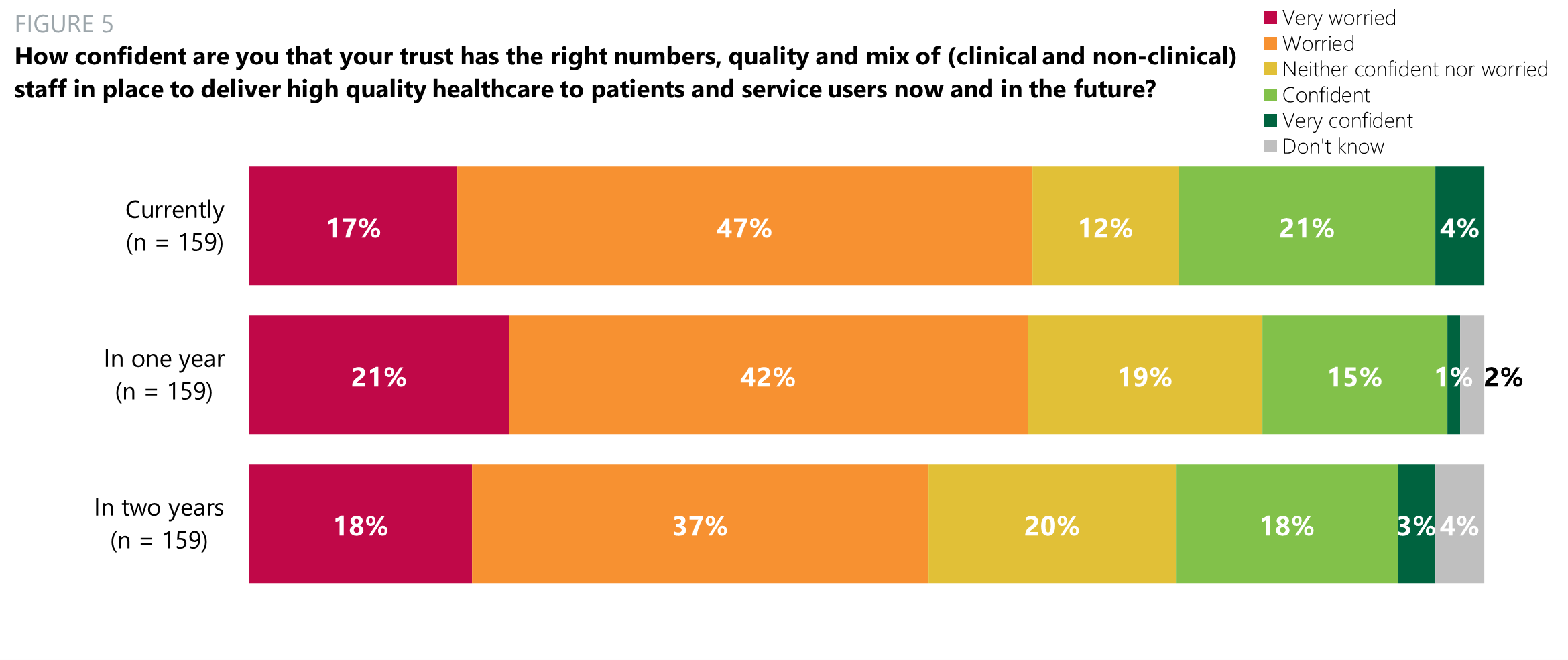
- 64% of trust leaders were very worried (17%) or worried (47%) regarding their trust having the right numbers, quality and mix of staff to deliver high quality healthcare currently. 12% were neither confident nor worried, 21% were confident and 4% were very confident.
- 63% of trust leaders were very worried (21%) or worried (42%) regarding their trust having the right numbers, quality and mix of staff to deliver high quality healthcare in the coming year. 19% were neither confident nor worried, 15% were confident, 1% were very confident and 2% did not know.
- 55% of trust leaders were very worried (18%) or worried (37%) regarding their trust having the right numbers, quality and mix of staff to delivery high quality healthcare in the coming two years. 20% were neither confident nor worried, 18% were confident, 3% were very confident and 4% did not know.
Burnout across workforce
- Almost all (94%) trust leaders were extremely (56%) or moderately (38%) concerned about the current level of burnout across their workforce. 6% were slightly concerned.
- Across different trust types, most trust leaders were extremely or moderately concerned, particularly in the one ambulance trust which responded (100% extremely concerned), mental health trusts (73% extremely concerned and 27% moderately concerned) and acute trusts (61% extremely concerned and 32% moderately concerned).
The biggest concern among trust leaders was the low level of staff morale, this was reported across respondents who were both extremely and moderately concerned. Respondents also highlighted the concern of workforce shortages.
“Staff in our organisation are at their lowest point through the pandemic. Increased demands from COVID-19, alongside pressure to increase activity and reduce waiting lists, means we lack the ability to transfer staff to support most pressurised areas (as we try to do everything), meaning it is harder now than at any time during the COVID-19 waves. Staff are suffering burnout and morale is extremely low.” Acute trust, South East
ICS(s) management of the allocation and distribution of funds to providers in 2022/23
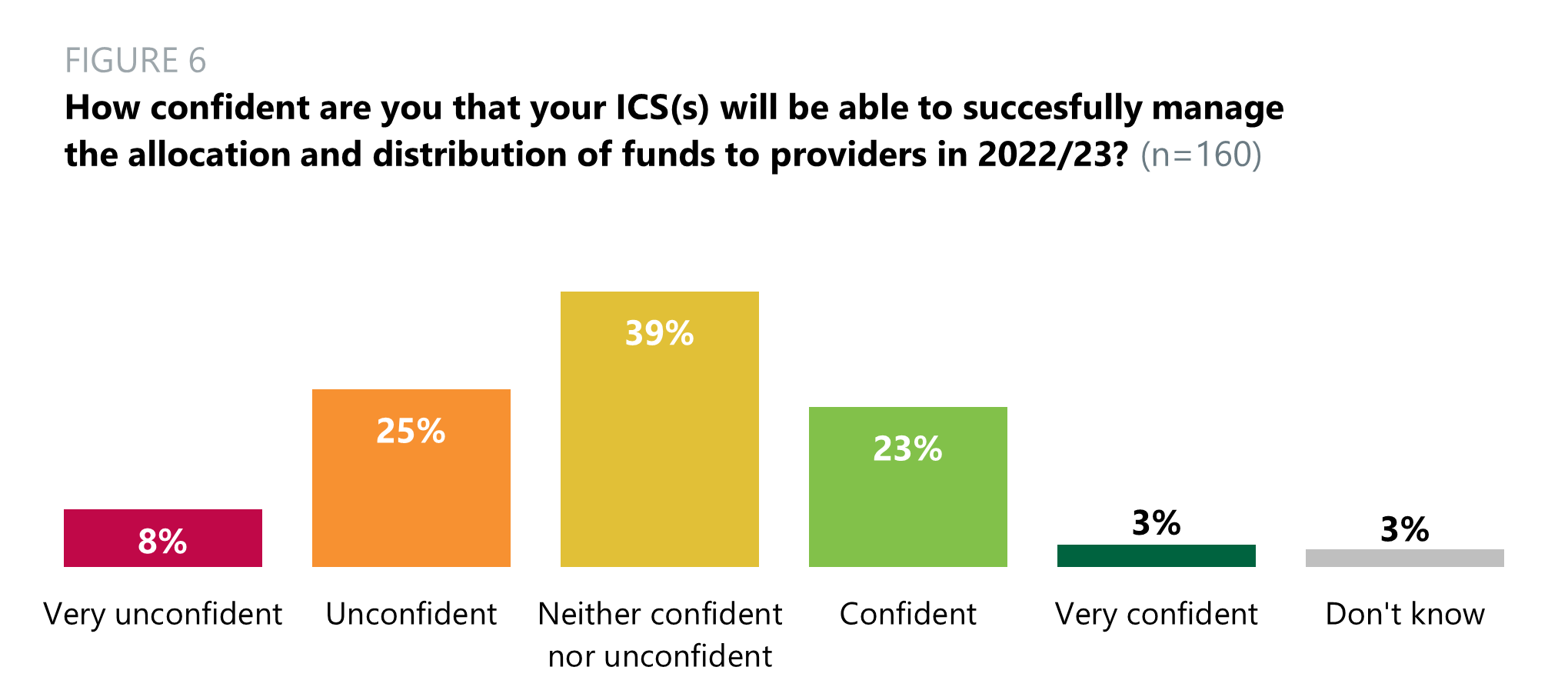
- There was a mix of confidence levels regarding the ability of ICS(s) to successfully manage the allocation and distribution of funds to providers in 2022/23. A third (33%) of trust leaders were very unconfident (8%) or unconfident (25%) their ICS will be able to successfully manage the allocation and distribution of funds. 29% were neither confident nor unconfident, 23% felt confident, 3% felt very confident and 3% did not know.
Thinking about the funding available to the NHS in 2022/23 and the continued move to ICS-led financial management, what is your biggest concern in relation to your trust's finances over the next 12 months?
- Trust leaders reported their greatest concern in relation to their trust’s finances over the next year is insufficient funds. It should be noted that this piece of work took place prior to the comprehensive spending review. Other respondents highlighted the uncertainty around the budget, which hinders their ability to plan accordingly.
Investment in social care in your local area
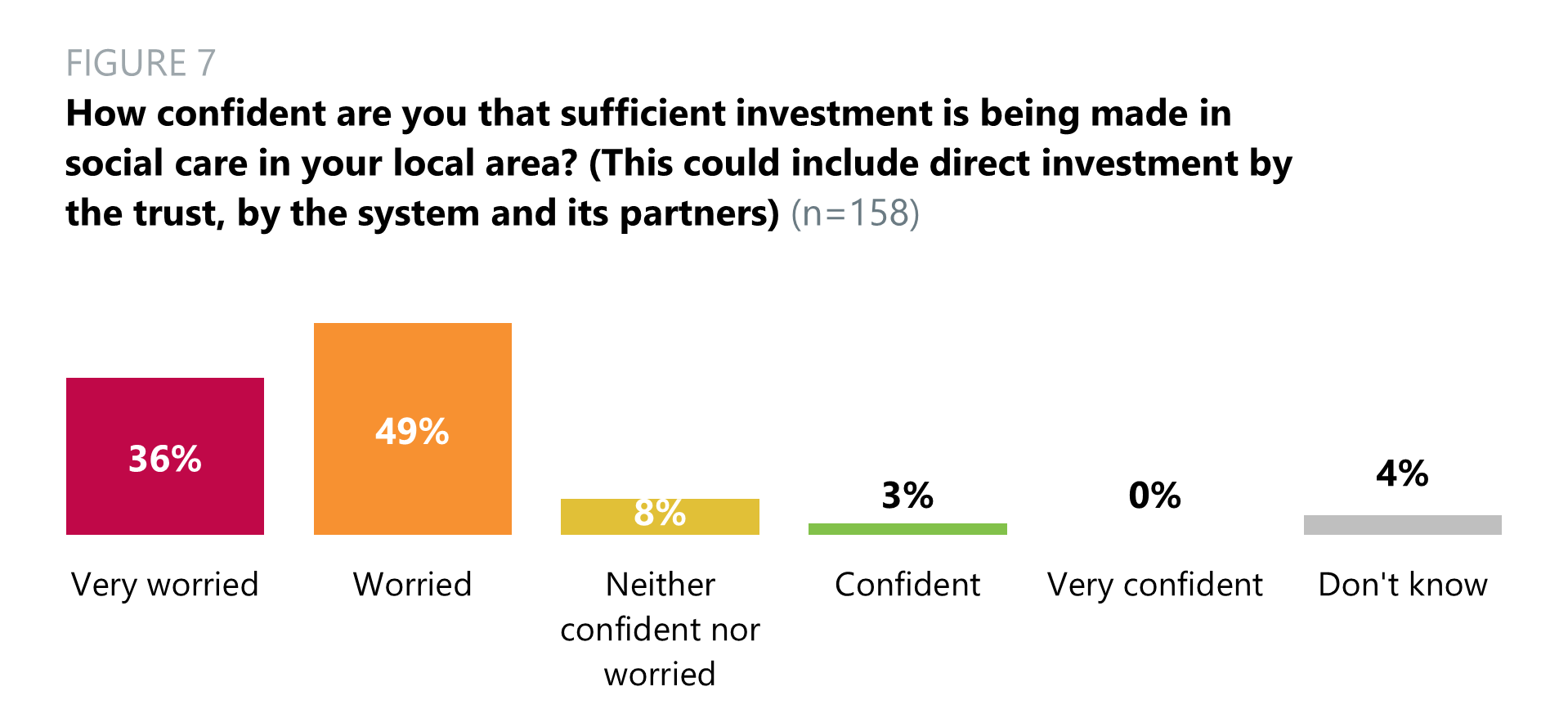
- A large number (85%) of trust leaders were very worried (36%) or worried (49%) that sufficient investment is being made in social care in their local area. 8% were neither confident nor worried, 3% felt confident and 4% did not know.
Support and infrastructure
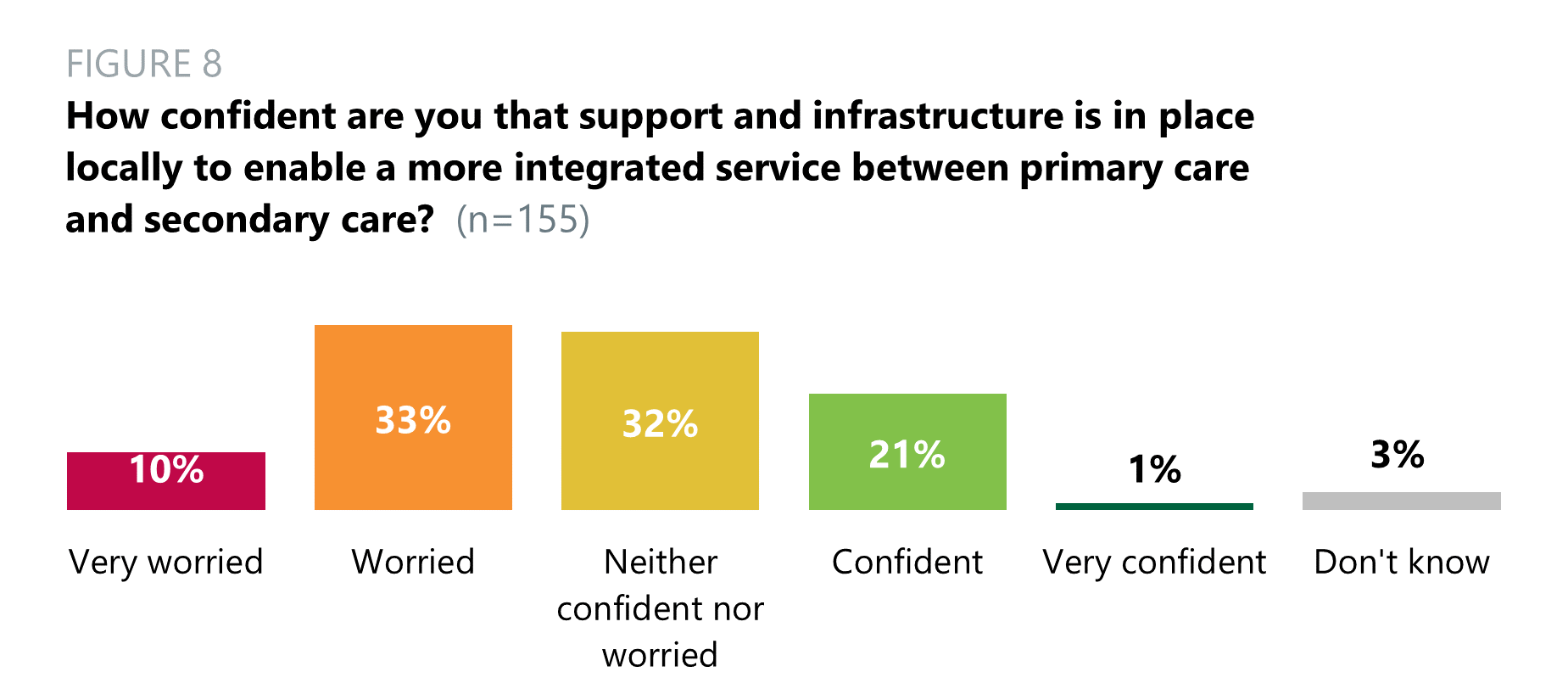
- 43% of trust leaders were very worried (10%) or worried (33%) about the support and infrastructure in place locally to enable a more integrated service between primary and secondary care. 32% were neither confident nor worried, 21% were confident and 1% were very confident. 3% did not know.
Some respondents felt confident about the support and infrastructure in place to enable a more integrated service between primary care and secondary care. The most common theme among these respondents was that they can see the effects starting to work.
Trust leaders who felt worried, extremely worried, or neither worried nor confident, highlighted the extreme pressures which primary care services are under. Another common theme was that integration takes time and therefore the effects are not evident yet.
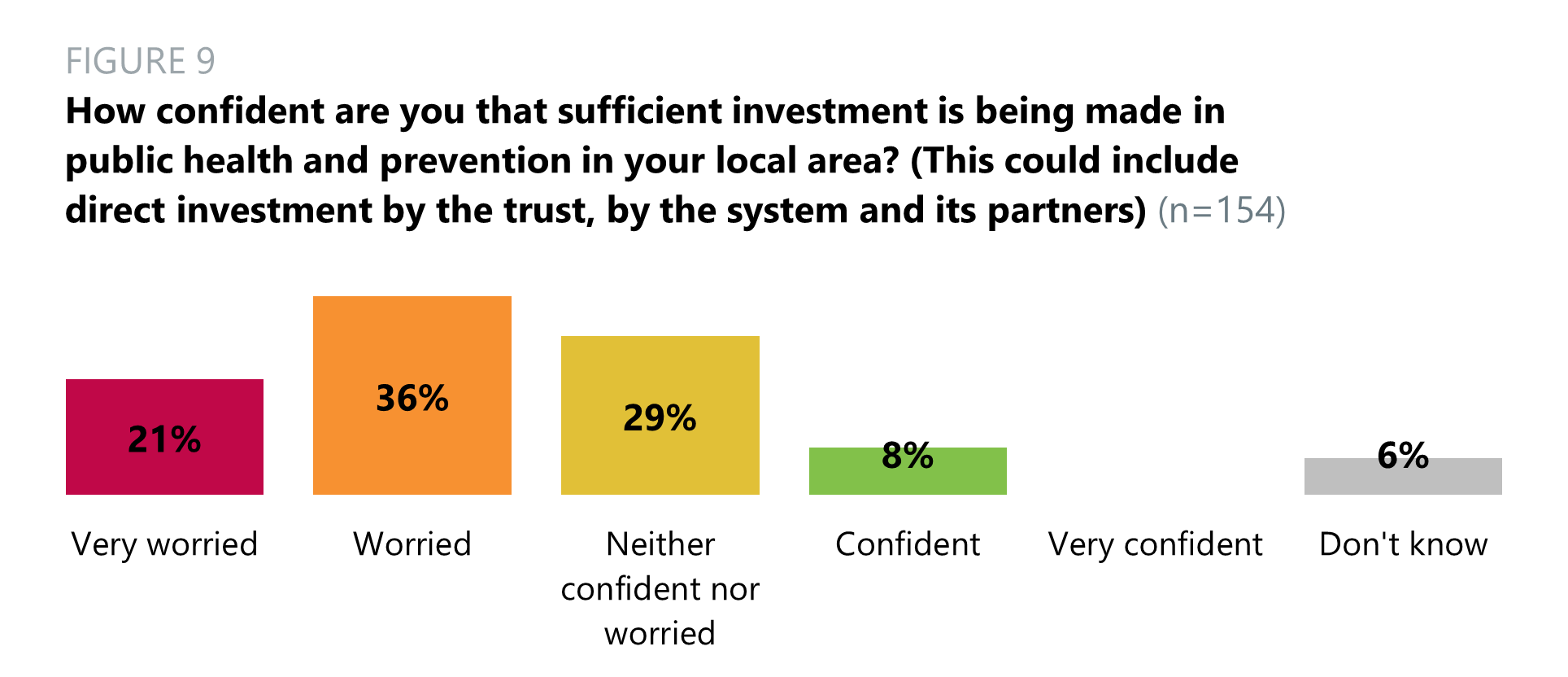
Investment in public health
Plans to embed system working
Better collaboration
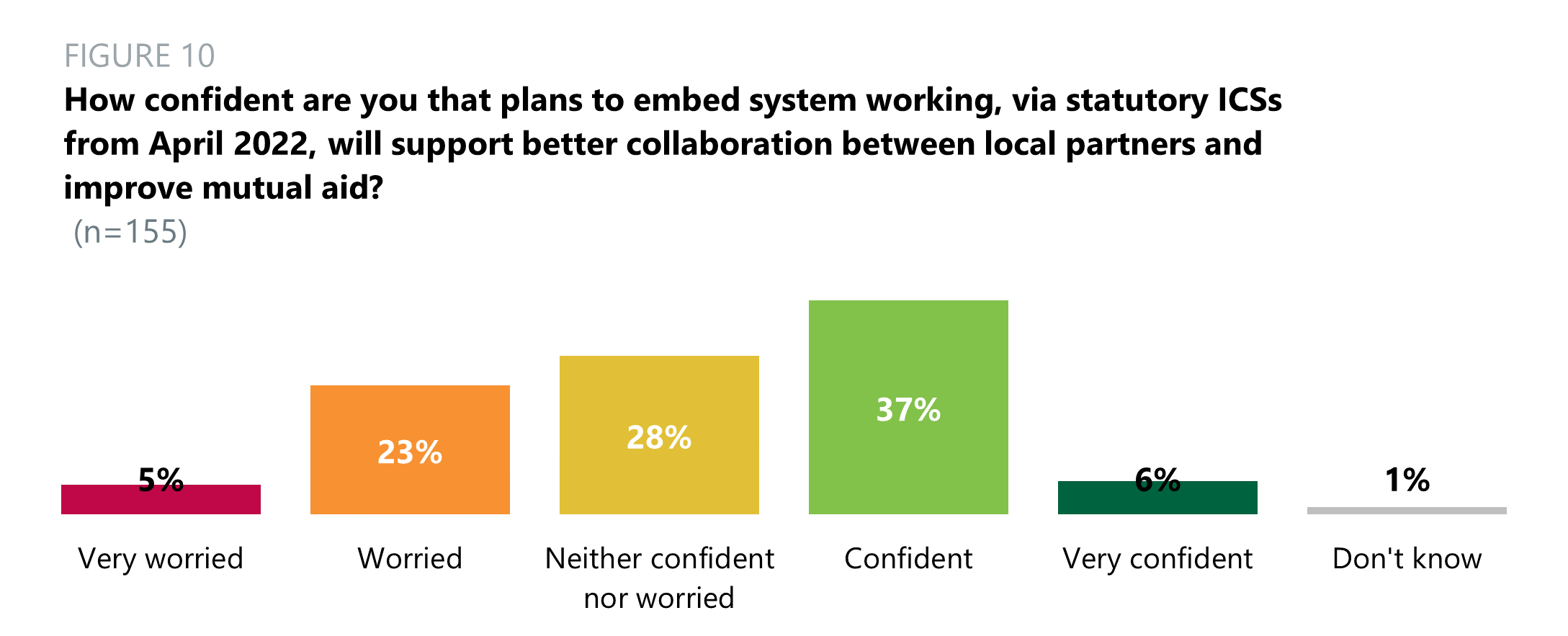
- When asked about how confident trust leaders were that plans to embed system working, via statutory ICSs from April 2022, will support better collaboration between local partners and improve mutual aid, 43% were confident (37%) or very confident (6%). 28% were neither confident nor worried, 23% were worried and 5% were very worried. 1% did not know.
Better outcomes for patients
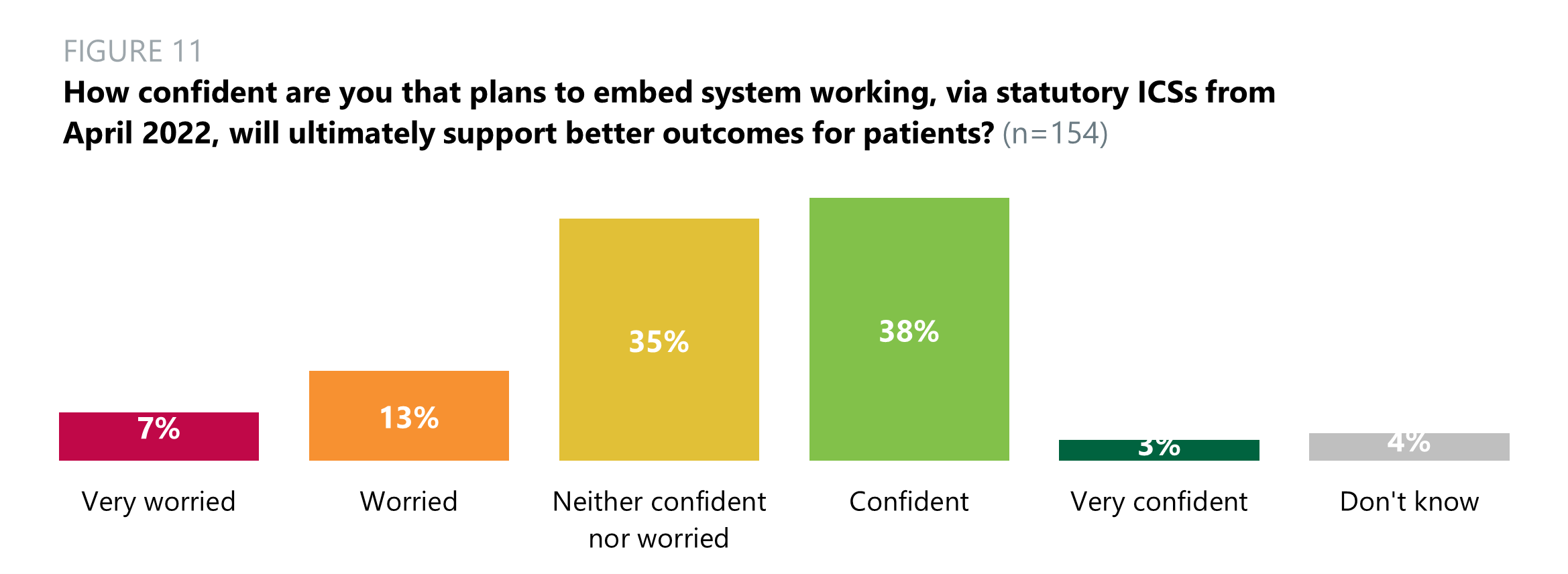
- When asked about how confident trust leaders were that plans to embed system working, via statutory ICSs from April 2022, will support better outcomes for patients, 41% were confident (38%) or very confident (3%). 35% were neither confident nor worried, 13% were worried and 7% were very worried. 4% did not know.
What key challenges and opportunities do you feel provider collaboration presents?
Opportunities highlighted by trust leaders focused on the chance to share resources, systems, and workforce, leading to increased productivity and a higher quality of care.
“We have already embarked on a provider collaboration which is working well and has certainly enhanced the patient experience and improved communication and understanding between partners.”
“We have already embarked on a provider collaboration which is working well and has certainly enhanced the patient experience and improved communication and understanding between partners.”
“An opportunity to reimagine the approach to healthcare is an exciting and invigorating one, but the context of continued pressure and limited capacity in the workforce and management of services makes the likelihood of successful transformation a real concern.”
“Opportunities for addressing health inequalities and access, and for developing more joint working between teams across different sectors. Challenges that central NHS bureaucracy will get in the way of local decision making/implementation.”
Respondents also provided a range of challenges that provider collaboration presents, including disputes over fundings, conflicting personalities, and a concern it could lead to bureaucracy.
What key challenges and opportunities do you feel the development of place based working arrangements present?
- The most prevalent opportunity that trust leaders raised regarding the development of place-based working was the ability to focus on and improve healthcare in local areas.
“Working with a focus on place will hopefully allow a greater level of detail to be given to local measures that will improve health outcomes for people close to their homes, reducing dependency on healthcare.”
- The challenges that concerned respondents varied greatly, the most common ones relating to financial issues, a lack of resources, working across different systems, and the potential for added bureaucracy.
Plans and activities from the national NHS leadership to effectively support the delivery of a sustainable service
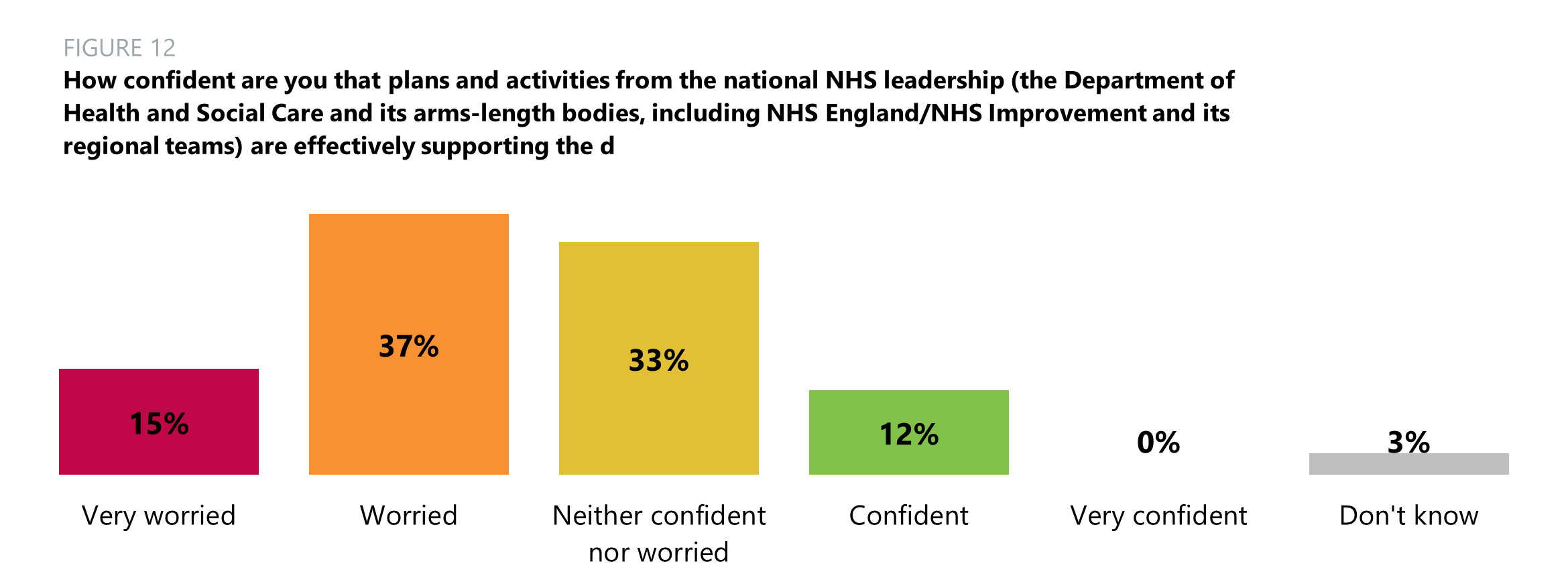
- Over half (52%) of trust leaders were very worried (15%) or worried (27%) about the national NHS leadership’s (the Department of Health and Social Care and its arms-length bodies, including NHS England and NHS Improvement and its regional teams) support for the delivery of a sustainable service in their area. 33% were neither confident nor worried, 12% were confident and 3% did not know.
Trust leaders identified various concerns with how national leaders in the Department of Health and Social Care, NHS England and NHS Improvement and regulators are effectively supporting the delivery of a sustainable service in their area. Their reasons tended to focus around finance – not enough funding, how funding will be allocated, and leadership being driven by financial targets. Other respondents were concerned that command and control is no longer needed at a local level, that the workforce shortages present a large uncertainty and questioned the Care Quality Commission’s approach during the pandemic.