

Introduction
Our NHS Winter Watch 2023/24 series concludes today following the release of this week's winter situation report data from NHS England. As always, the data provides valuable insights into the situation across emergency care and hospitals. Today's data cover the period from 26 February to 3 March.
This week's winter data show that the challenges on the ground persist as demand for urgent and emergency care increases and bed occupancy levels remain high. However, the data also shows some more positive trends which continue to highlight the efforts of staff and trust leaders to match the increases in demand and seasonal pressures.
Winter situation report (26 February – 3 March)
A&E closures and diverts: There were no A&E closures again this week. There were 19 A&E diverts this week, nine fewer than the week prior but eight more than the same week last year.
Ambulance arrivals: A total of 92,763 patients arrived by ambulance. An increase of 1.3% since last week and up by 16.3% compared to the same week last year.
Ambulance handovers: 23.7% of ambulance handovers were delayed by 30 minutes or more, down from 27% last week. 7.5% were delayed by 60 minutes or more, down from 9.5% last week. A total of 13,881 hours were lost to ambulance handover delays, a decrease of 26.2% from last week and down by 9.6% compared to the same week last year.
Critical care: Adult critical care bed occupancy is at 78.1% this week, down from 79.7% last week. This is also below levels seen in the same week last year (78.7%).
Diarrhoea and vomiting (D&V): The number of beds closed due to D&V and norovirus has increased by three to 578. This is lower than the same week last year (720).
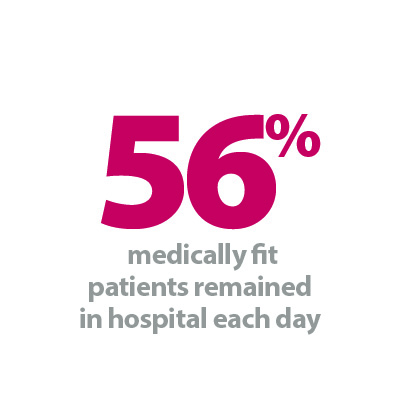
Discharges: There was an average of 23,905 patients each day who no longer met the criteria to reside, 236 fewer than the week prior. Compared to last week, a larger proportion of patients remained in hospital this week, with 56% (or 13,375) staying in hospital.
Flu: This week the average number of general and acute beds occupied by flu patients each day was 1,256. This is 3.1 times greater than the same time last year (398). An average of 77 critical care beds were occupied by flu patients each day this week, 21% fewer than the week before, but 2.4 times greater than the same week last year (32).
General and acute (G&A) beds: There was an average of 102,894 G&A beds open across all acute trusts. On average each day, 49 G&A beds were unavailable and void to non-Covid admissions. The average bed occupancy rate fell by 0.5 percentage points to 93.3%. This is one percentage point lower than same time last year (94.3%).
Long stay: The number of patients staying in hospital longer than seven, 14 and 21 days decreased since last week (down by 1.2%, 1.1%, and 0.5% respectively).
Neonatal intensive care beds: For all trusts, bed occupancy has increased and is now at 69.2%, up from 68% last week. The average number of care beds open remains at 1,724, the same level as the previous week.
Paediatric intensive care beds: For all trusts, bed occupancy has increased to 78.2%, up from 75.4% last week. The average number of care beds open has increased by one bed to 367 since last week.
Respiratory syncytial virus (RSV): An average of nine paediatric beds were closed this week due to RSV symptoms, down from 10 last week and 10 during the same week last year.
Staff absences: There were an average of 45,629 total absences each day this week, of which 2% were Covid-19 related (943). The total number of staff absences decreased from the week before (46,191) but the proportion of Covid-19 related absences remained the same.
Our view
As spring begins, this week's data highlights the sustained pressures felt by seasonal illnesses. The number of patients in hospital with flu fell this week. Although a positive trend, levels remain three times higher than the same week last year showing the prolonged nature of this year's seasonal illnesses.
Demand for urgent and emergency care continues to apply pressure across systems, as the total number of patients arriving by ambulance increases again this week to almost 93,000. However, hours lost to ambulance handover delays has fallen again this week to the lowest level seen so far this winter. This shows the hard work and collaboration between ambulance and hospital staff to tackle delays.
Overall, patient flow continues to be a challenge for trusts as over half of patients (56%) who are medically fit to be discharged remained in hospital. Bed occupancy levels also remain a cause for concern with 93.3% of G&A beds being occupied. Paediatric intensive care and neonatal intensive care bed occupancy has also increased this week to 78.2% and 69.2%, respectively.
Although we have technically reached the end of winter, the sustained demand for ambulances and high bed occupancy means nothing has changed for trusts. This winter trusts have had to contend with increasing demand, system wide pressures and industrial action which has led to thousands of appointments being rescheduled. There is no doubt that trusts will continue to experience these challenges beyond the winter period while trying to tackle waiting times and meet key national recovery targets.
Wellbeing and a Listening Leadership: What 'Outstanding' looks like.
For this week's NHS Winter Watch campaign, we take a look at how North Staffordshire Combined Healthcare NHS Trust have 'pursued empowerment of staff at all levels'. In this case study we speak to, Donna Cantrell, associate director acute and urgent care, North Staffordshire Combined Healthcare NHS Trust, a passionate leader and wellbeing ambassador where everyone matters.
We all have our 'go to' mechanisms of support, or that one person who just knows what to say and when to say it, and without much more thought, we get right back to it, onto that hamster wheel called life. We tread through, what feels like the daily treacle of work, home, family, recreation; trying to find that right balance, trying to complete that last report, and send those final emails. Trying to make sure that service delivery is at its optimal while ensuring the whole workforce is ready for any visitors that may come our way wanting to know how well we are performing, or how well we are led, or how well our patients are cared for.
Here at North Staffordshire Combined Healthcare NHS Trust, things may seem just like anywhere else, with the same difficulties, challenges and constraints that are impacting across the NHS, and system partners nationally. Alas, however, we are poles apart from others when tackling those difficulties, challenges and constraints.
In 2019, we were rated 'Outstanding' by the Care Quality Commission, whereby it was noted that leaders were pursuing the "empowerment of staff at all levels". In the 2021 NHS Staff Survey, which measured performance against the seven NHS People Promises, North Staffordshire Combined Healthcare NHS Trust achieved the best results among all 217 English trusts, coming first on three promises and second on two others. We maintained these scores in 2022, leading in four of the seven promises, and in November 2022, we were awarded the HSJ's Trust of the Year Award.
In December 2023, Manager in Partnership quoted: 'North Staffordshire Combined Healthcare NHS Trust has a good claim to be England's best trust. In conversation with Matt Ross, Dr Buki Adeyemo explained the ingredients for the trust's remarkable success against the odds: a stable and happy workforce, a listening leadership, ambitious goals, and an enthusiasm for innovation'.
I am very fortunate to work in an organisation that embraces positive culture, staff development, and staff wellbeing. Senior leaders and executive members are approachable and responsive to creativity and innovation. Through transformational leadership and engagement across the trust, we have seen a significant improvement in staff engagement and workforce health, and a significant improvement in the delivery of safe, responsive, and effective care.
Over the last 12 months, I took the time in the early stages of implementation to engage with staff in a positive, open and motivational way, listening to staff and responding to their ideas, concerns, and compliments. Towards the end of 2022, acute and urgent care directorate responses for the NHS National Staff Survey were the highest ever recorded, and from April 2023 the introduction of various initiatives including the Combined Run Club, the Menopause Café, and Combined Voices (our trust staff choir) have truly put North Staffordshire Combined Healthcare NHS Trust on the map for staff who feel inspired, motivated, and valued.
Over the winter period we have seen the introduction of our first clinical Directorate's Wellbeing Days, with a complete focus on staff wellbeing, and on these days, staff are provided with options of meaningful activities along with full health MOT checks. This has further expanded to include further Health MOT sessions planned for all staff, a Men's Support Group and a Weight Management Group.
From a workforce health perspective, and using comparable data 12 months apart, within the acute and urgent care directorate, we saw a 54% reduction in short term sickness, and a 47% reduction in the rate of stress, anxiety and depression recorded sickness.
Staff engagement, morale and culture has shifted over the last 12 months with more staff completing staff surveys and engaging in their own team development strategies.
For all initiatives, I wanted to bridge the gap between board and ward, and we have achieved this. Executives attend the choir, along with a range of staff across the organisation, but when we all walk into the room, we are all just a group of individuals who have come together to have fun and experience the sense of wellbeing that music brings.
The importance of staff wellbeing is talked about more in meetings, from team to board level. This enables a shift of culture and enables inclusivity and positive focus points.
Over this same period, we have also seen an improvement in performance of key performance indicators for patient care. This is sustained month on month, demonstrating that while staff engagement and wellbeing improve, so does the care to our patients and communities.