Why is this important?
NHS England and NHS Improvement set out in its 2021/22 Priorities and operational planning guidance a key ambition on transforming community and UEC to prevent inappropriate ED attendance, improve timely admission to hospital for ED patients and reduce length of stay. This includes ensuring the use of NHS 111 as the primary route to access urgent care (NHS 111 First), safely reducing avoidable attendance at ED and a key focus on same day emergency care (SDEC) programmes. Other ambitions set out in the guidance include accelerating the restoration of elective care, managing increasing demand on mental health services and working collaboratively across systems to deliver on these priorities. Ambulance trusts have a key role to play in working as part of ICSs to deliver on these ambitions.
Prior to the pandemic, the long term plan was clear on its ambition to provide patients with the care they need as close to home as possible and reduce pressure on emergency hospital services through reforming how urgent care is organised and delivered. It states, "By 2023, CAS will typically act as the single point of access for patients, carers and health professionals for integrated urgent care and discharge from hospital care" (NHS England and NHS Improvement, January 2019). The plan also discussed the use of urgent treatment centres to ensure a consistent model of out-of-hospital urgent care and laid the trail for a comprehensive workforce strategy (the People Plan), noting the need for greater workforce flexibility and coordinated national workforce planning.
How does it work?
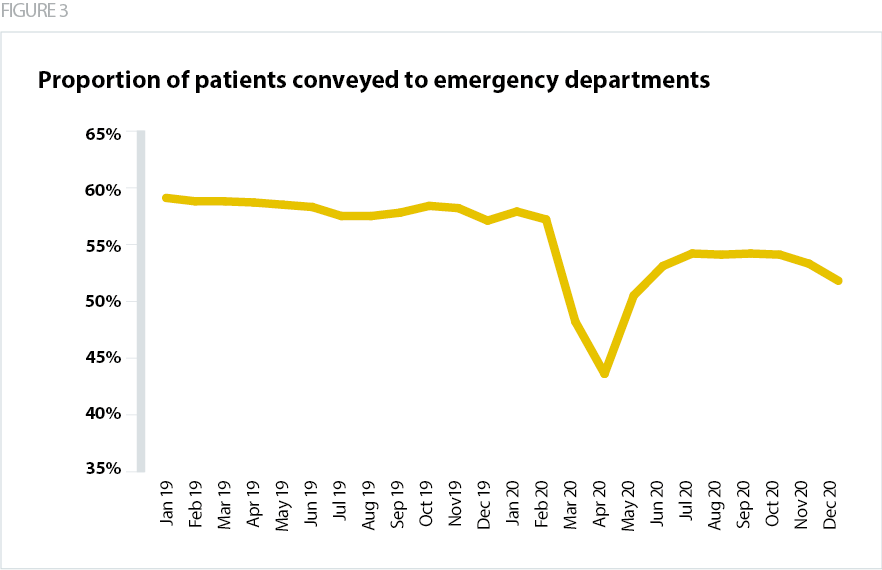
As highlighted in the 2018 Carter review of operational productivity and performance in ambulance trusts (NHS England, September 2018), the sector is instrumental in delivering care closer to home and reducing unnecessary pressures on hospitals. Despite increasing demand, ambulance clinicians are taking fewer patients to ED year on year. Ambulance trusts already deploy 'hear and treat' and 'see and treat' response models, navigating patients through appropriate pathways, and signposting others to relevant services, so keeping people out of hospital wherever possible. Ambulance clinicians only convey to ED when there is no other safe option for the patient and when the patient needs comprehensive assessment, treatment in the ED or admission. Greater access to suitable alternative care pathways, available 24/7, could reduce this still further.
In 2019, the proportion of see and treat cases was 29.8%. This increased to 33.9% in 2020. For hear and treat, there were 6.5% in 2019, rising to 8% in 2020. This is a promising trend as it means the proportion of people being kept out of hospital is rising, suggesting that the shift in approach is leading to positive results. This trend is illustrated below, in relation to the proportion of patients being conveyed to EDs between January 2019 and December 2020.
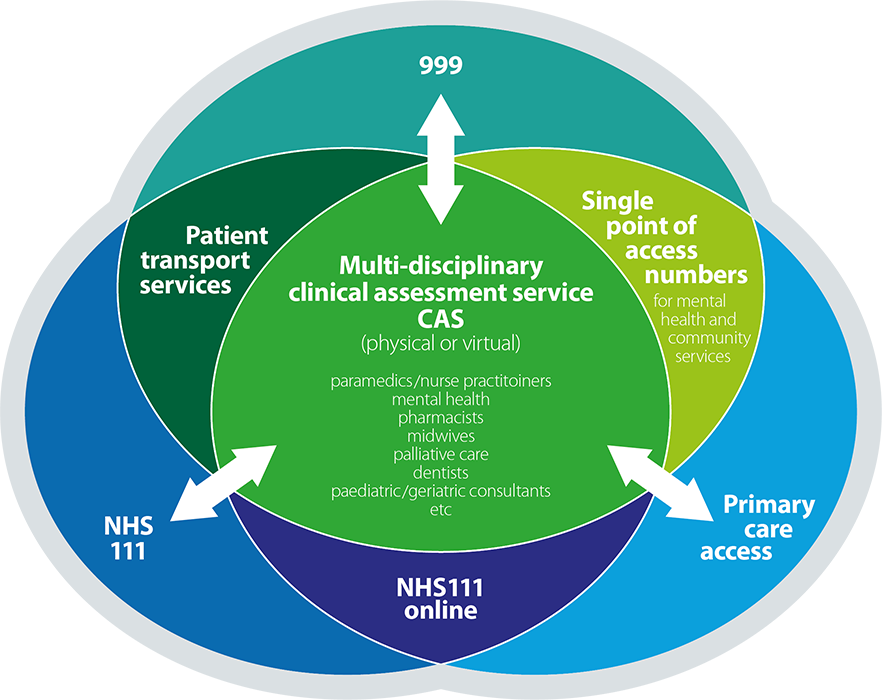
Many ambulance trusts are now working with other providers and commissioners in their region to deliver integrated urgent care services. The multidisciplinary CAS forms a central part of this. The model is designed around having a single point of access for UEC, through which a patient can then access the appropriate service. This means scarce resources are not duplicated in multiple CASs, and patient flow is streamlined, leading to a better patient experience. It also allows for effective strategic commissioning, whereby local needs can be identified and resources matched accordingly, for example ensuring there is additional mental health expertise as part of the CAS in areas of high need. The mental health focus of several trust initiatives is explored further in the Innovative workforce models section of this report and the 111 First model is covered further in the Digital transformation section.
It is also important to realise the ambulance sector’s full potential to support elective recovery and measures to tackle the care backlog. Non-emergency patient transport services (NEPTS), some of which are provided directly or coordinated by ambulance trusts, support the smooth-running of the healthcare system, ensuring that patients arrive on time for their appointments and that, when being discharged, they can return home quickly. The current PTS market is quite fragmented but the move to system-working provides a significant opportunity for larger system-wide PTS contracting or coordination. This will play a key role in tackling the backlog through efficient use of resources across systems and regions and helping to tackle health inequalities by supporting patients who need help to access the care they need.
FIGURE 4
Single point of access model
What needs to happen to make this a success?
True collaboration between different types of providers and wider system partners is fundamental to ensuring the integrated model is a success. Ambulance trusts must be involved in regional, ICS and place-level decision making about service design, including defining what single point of access means in practice and over what size footprint. AACE has developed a blueprint model for joined up access to UEC through 999/111 into CAS and onto the appropriate response model or care pathway or local service. By establishing this model on wider footprints, systems can avoid fragmenting services and duplicating use of scarce clinical resources by having multiple access points and CASs within regions. It also creates a resilient and interoperable infrastructure that can make the most of digital innovations and provide clear oversight of how population health needs can best be met.
FIGURE 5
Right care, first time, every time

It is vital that NHS England and NHS Improvement continues to engage with the sector on evolving ICS guidance to ensure that the guidance reflects the unique nature of the ambulance service and recognises its further potential in supporting system-wide transformation. AACE is currently engaging with NHS England and NHS Improvement and ICS leaders to explore the concept of a single regional commissioning board with oversight for ambulance services working across multiple ICSs. As part of this, there is an opportunity to build on learning from the COVID-19 pandemic in working at scale across regional and ICS footprints.
As explored further in the Digital transformation section of this report, we also need digital platforms that are interoperable and allow ready access to patient information, care plans and referral routes between healthcare providers. This model benefits from economies of scale and is already being implemented in a number of areas.
Where is it happening?
CASE STUDY
South Central Ambulance Service NHS Foundation Trust
Provider collaboration to deliver NHS 111 and integrated urgent care service
South Central Ambulance Service NHS Foundation Trust (SCAS) provides integrated urgent care services through collaborative models across Thames Valley, Hampshire and Surrey Heath, covering three ICSs. This case study focuses on the provider partnership in Hampshire and Surrey Heath.
The service’s ambition is that anyone contacting the NHS via 999, 111 or online will be offered the right care, at the right time, in the right place in response to their enquiry, needs and circumstances. The aim is to connect callers to the most relevant specialist, either on the telephone or digitally when appropriate, so that neither the patients nor the clinicians have to travel to see each other unless this is necessary for someone’s clinical assessment or treatment. When further assessment or treatment is required in a face to face setting, the aim is to conclude the telephone assessment with a booked appointment.
Over the years, the partnership model has strengthened and broadened, and there are now a wide range of primary, urgent, emergency, mental health and specialist care partners working together. By leading the collaborative work, through a variety of contractual and partnership arrangements, SCAS is hosting multi-agency teams on a shared technical platform and the public is benefiting from a 24/7 multi-disciplinary CAS.
The benefits of the scheme have included patient access to a virtual CAS via the NHS 111 service, increasing the rates for self-care and reducing the rates for 999 and ED referrals. The new multidisciplinary approach has also brought benefits to staff, who are able to learn from each other in a more diverse clinical team with greater breadth of expertise.
Although the lead-provider contract only started in June 2021, most of the planned developments were fast-tracked during 2020, in order to support the wider system response to the pandemic pressures. This helped to assess more people clinically on the telephone, to resolve enquiries remotely whenever appropriate, and to book people into other services if needed.
Partners are engaging in work to review the assessment and care pathways available in each local care system after people contact the NHS via 999, 111 or online. These reviews involve both providers and commissioners, and provide a foundation for ongoing work to identify any inequities in access, service gaps or scope for further improvement. They also help to share learning and best practice across local care systems.
CASE STUDY
South Central Ambulance Service NHS Foundation Trust
Paramedic on-scene referrals support tool
SCAS identified that there were key areas for improvement in its service, including non-conveyance rates, managing patients out of hospital and improving tools for referral. SCAS recognised that sometimes the wrong patients were being conveyed to hospital and, although there was a clinical requirement for additional investigation and/or intervention, it was clear that the ED was not the right care environment.
Taking a system-wide approach and focusing on same day emergency care (SDEC), a model of care aimed to minimise and remove delays in the emergency patient pathway, the trust has enabled on-scene referral into SDEC and other secondary care services for paramedics and clinical staff. A key aim of this model is that patients receive care in the right place, first time, helping to improve patient flow.
SCAS has utilised a system called ‘SCAS Connect’, an app-based tool for effective referral, as an enabler for this work. 63% of clinicians now access the system and 69% of patients have received a more appropriate primary or secondary care service referral as a result. The work is ongoing as part of the SCAS urgent care pathway improvement programme with the aim to build up confidence and utilisation of the tool to 100%.
The main criteria for referral is reliant on not only the system to guide paramedics but also the clinical conversation with the service that’s being referred to. This supportive measure to encourage referrals allows SCAS clinicians to understand that no decision needs to be made in isolation. To highlight this the team have been utilising the strapline, 'Click before you call; call before you convey'.
The trust has had to navigate a number of challenges with developing this way of working, including the culture shift needed for frontline paramedics in considering different referral routes, ensuring consistent SDEC provision across the region, data extraction, and effective utilisation of the SCAS Connect system. To help overcome these challenges, SCAS acknowledged the best approach was to collaborate and ensure teams felt ownership of the new model.
The benefits of the model have included having more options for paramedics on-scene, including a number of 24/7 services, a continuing downward trend of non-conveyances and enhanced patient experience. In total, 9,422 patients have been directly referred to either medical or surgical SDEC from SCAS paramedics, meaning they have not been conveyed to an ED. This is a huge step in the right direction for improving patient experience, using clinical time effectively and avoiding unheralded demand in ED. SCAS is continuing to expand the model within the region with the aim of ensuring that 100% of patients experience care in the right place, first time.
CASE STUDY
Yorkshire Ambulance Service NHS Trust
Regional coordination of non-emergency patient transport services
Yorkshire Ambulance Service NHS Trust (YAS) is taking on board learning from its role in regionally coordinating NEPTS during the COVID-19 pandemic. National guidance in response to the pandemic meant NHS ambulance trusts were mandated to coordinate and support all regional NEPTS contracts. This was to ensure sufficient oversight and support for patients requiring transport to and from NHS services. It also meant that an accurate assessment of the situation in each region could be established for national decision-makers.
At the start of the pandemic, YAS engaged with transport providers throughout the region, including local authorities, community and voluntary organisations, taxi companies and private ambulance services to coordinate resources. While there were far fewer patients attending outpatient appointments or being taken into hospital for elective procedures, the focus was to support discharge from hospitals to ensure there was sufficient capacity for incoming COVID-19 patients and to continue supporting patients for urgent treatment and diagnostics.
YAS provided a single point of access for teams across primary, acute and community care services to escalate PTS needs, including supporting providers, for example around PPE supply and ensuring the right vehicles and mitigations were provided for safe patient journeys. The trust also provided NHS England and NHS Improvement with daily PTS activity data, to ensure oversight of transport capacity and to escalate any regional concerns. As well as developing existing trust volunteers, YAS launched a campaign to recruit more members of the public and now has almost 300 volunteers supporting PTS.
The trust had to navigate challenges in coordinating NEPTS providers, including:
- information sharing
- access to personal protective equipment (PPE) for non-NHS providers
- high staff absences due to COVID-19 related sickness or isolation
- a 40% vehicle capacity reduction due to social distancing, which led to the need for increased funding support from commissioners.
The main benefits of regional coordination were that patient journeys continued in a timely manner, waiting times in hospitals were kept to a minimum and, in turn, the infection risk to patients, staff and members of the public was reduced. By coordinating resources at a regional level, YAS was able to manage capacity fluctuations in other parts of the system. Staff both within YAS and other PTS providers benefitted from increased confidence as a result of being supported in an uncertain environment.
The trust intends to build on the relationships established during the pandemic to respond to the increased demand for planned care and backlog recovery over the coming months. An important part of this relates to tackling health inequalities by ensuring people are able to access healthcare. Ensuring that non-emergency patient transport continues to be part of the conversation with ICSs is just one of the many steps that ambulance trusts can take to help prioritise patients who need healthcare services the most.
