The need to deliver efficiency savings
Trusts and systems recognise the importance of an increased focus on efficiency to deliver best value for taxpayers' money.
NHSE sets an annual 'efficiency factor' across the provider sector. This requires trusts to find means of accounting for the disparity between income and expenditure driven by a rise in demand for services and multifactorial cost pressures. Modelling from NHSE suggests that, between 2008/09 and 2017/18, providers became on average 0.9% more efficient, though it noted that the level of efficiency savings had slowed in recent years. The efficiency factor of 1.1% set in 22/23 was considered as 'challenging but achievable' by NHSE.
Cost improvement programmes
Cost improvement programmes (CIPs) are efficiency plans adopted by trusts to use their limited resources in a more efficient way – this can include utilising operating theatres more effectively, treating more patients within the same facilities, reducing waste and improving patient flow.
Once income and expenditure are accounted for, as well as planned service improvements, cost-uplifts and inflationary pressures, the national efficiency factor actually translates into a significantly higher efficiency savings rate for trusts. Therefore, while the national efficiency target has doubled to 2.2%, as we show below, trusts will have to deliver efficiency savings above this figure and exceed the levels they managed to achieve prior to the pandemic.
At this time, it is unclear what proportion of CIP savings will be recurrent. There is a risk that high efficiency savings targets may compel trusts to deliver undesirable, non-recurrent savings: while these may cut costs in the short term, they do not represent permanent savings to providers' cost bases and are not conducive to overall recovery and reducing the care backlog.
The efficiency challenge can also be compounded when capital funding is allocated to trusts to expand services but there is no additional revenue funding for the capital charges in subsequent financial years. The consequential cost pressure must then be met by additional efficiency savings.
The forecast for efficiency savings
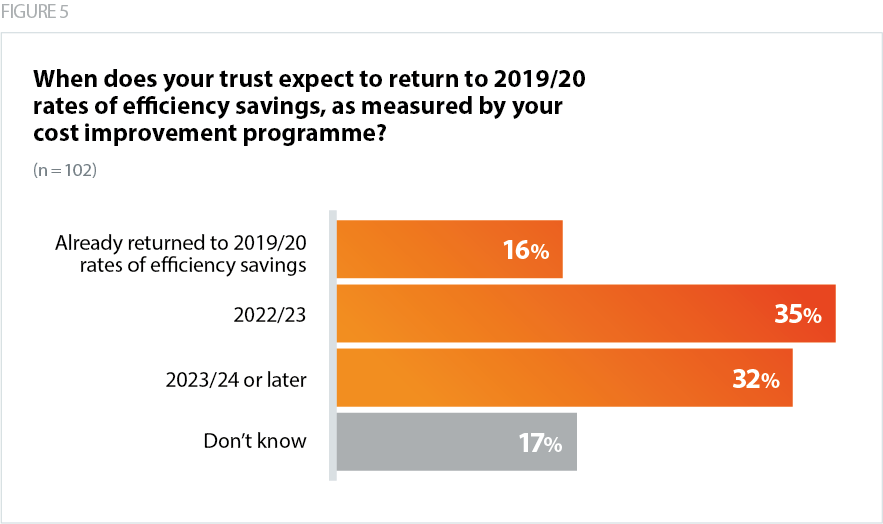
- Just over half (51%) of trusts surveyed expected to return to 2019/20 rates of efficiency savings in 2022/23 as measured by their CIPs.
Our survey results show there is a significant gap between the efficiency ask required by government and NHSE and the level individual trusts consider to be realistic and deliverable in 2022/23. When comparing respondents' realistic efficiency savings target for 2022/23 against their 2019 efficiency savings rate, out of the 91 respondents who provided answers for both questions, almost three out of five respondents (58%) said their realistic efficiency savings target for 2022/23 would be below their 2019/20 efficiency savings rate. 29% said it would be the same and 13% said it would be above.
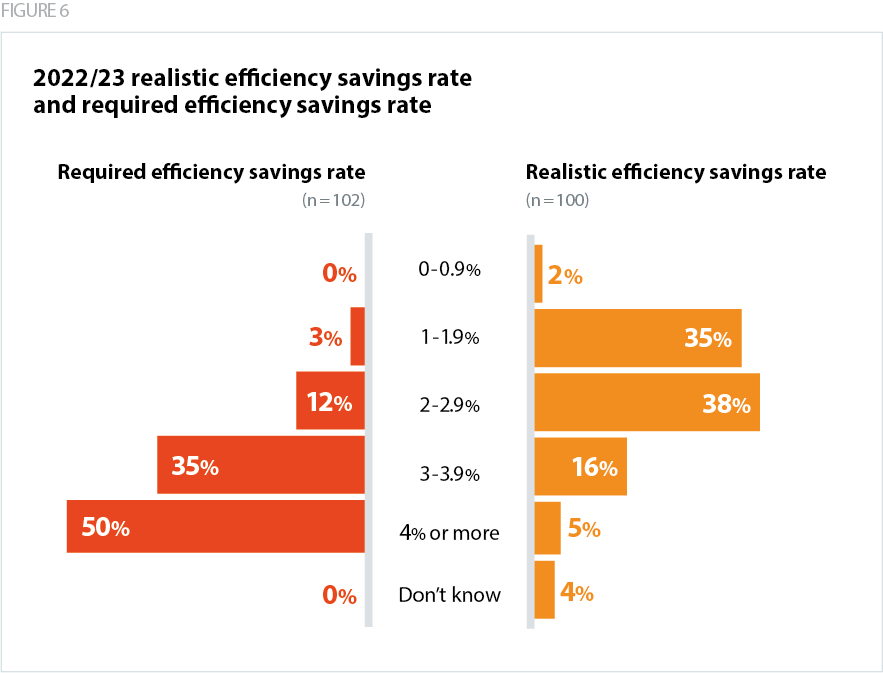
- The average 2019/20 efficiency savings rate of trusts surveyed was 2.81%. However, the average estimated required efficiency savings rate for 2022/23 is 4.04%, whereas 73% of respondents told us that a realistic and achievable efficiency savings target – as measured by cost improvement programmes – would be between 1% and 2.5%.
Barriers to delivering efficiency savings
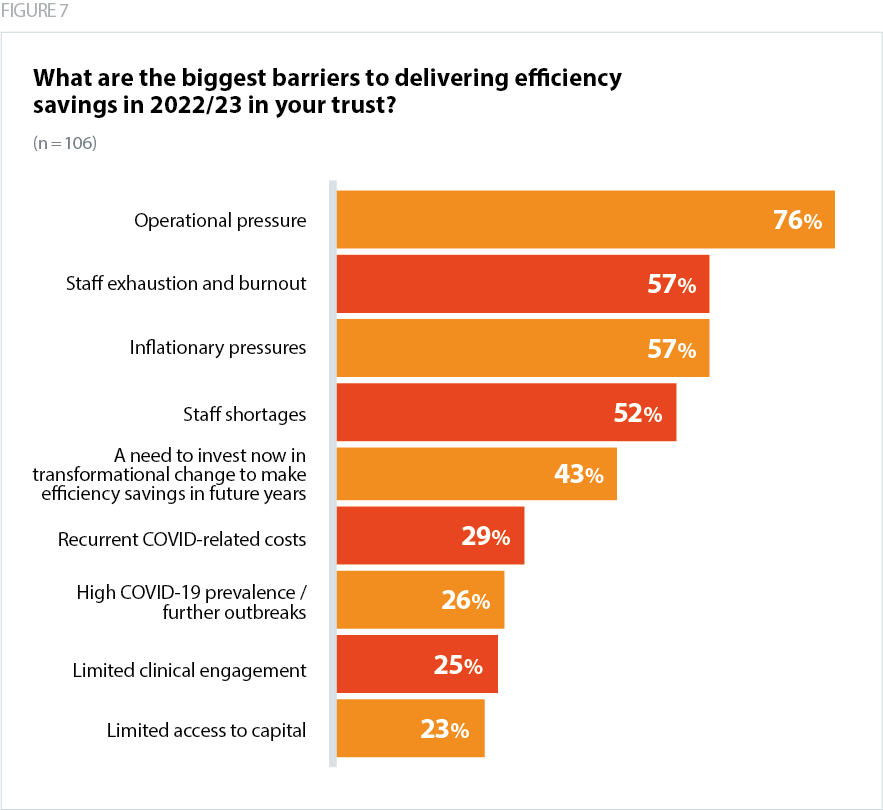
In addition to the cost pressures eroding the value of the cash settlement – including the withdrawal of COVID-19 funding and significant inflationary pressures – survey responses indicated a number of limitations on trusts' capacity to realise efficiency savings at the level expected by government and NHSE.
Operational pressures and COVID activity
- Just over three out of four respondents (76%) said that operational pressures are the largest barrier to delivering efficiency savings in 2022/23 in their trust.
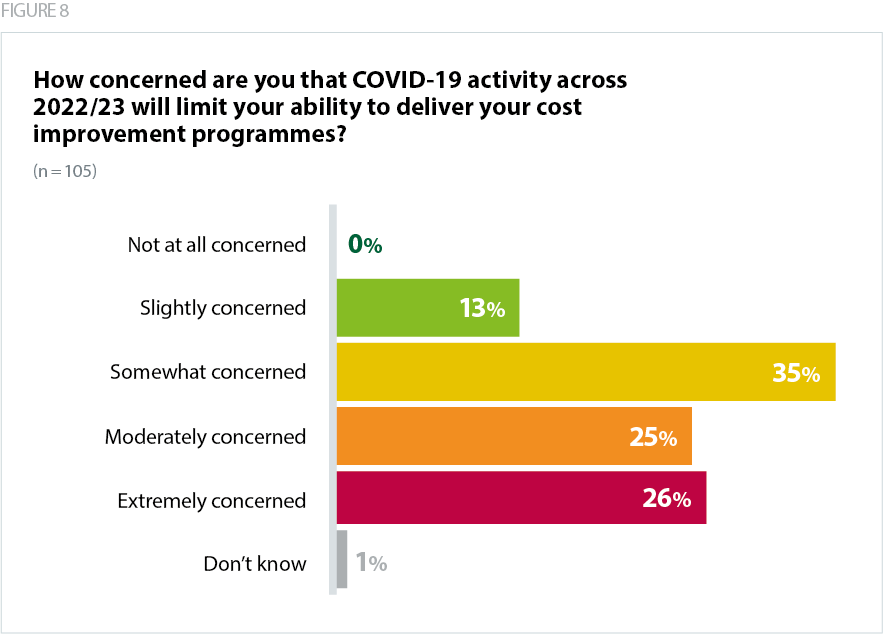
- Just over half of respondents (51%) are moderately or extremely concerned that their COVID-19 activity across 2022/23 will limit their ability to deliver cost improvement programmes.
While vaccination and new treatments mean morbidity and the clinical impact of COVID-19 has become less severe for the general population, the need to deliver care to patients presenting with COVID-19 throughout 2022/23 will still impact operational efficiencies, even with the update to the infection prevention and control (IPC) guidance. COVID-19 is disruptive as trusts make clinical and operational decisions to separate patients, often impacting their ability to sustain elective activity or recover care backlogs.
Workforce
Survey respondents noted how increased levels of staff absence on wards limits the capacity for trusts to deliver recurrent cost savings by reducing agency spend (which for some is a key element of their CIPs). Consequently, they are often forced to resort to paying a premium for outsourcing recruitment and hiring agency staff at a cost above the pay scales of the Agenda for Change (AfC).
Limited leadership bandwidth to engage with CIPs
To successfully deliver sustainable efficiency savings, trusts must have the buy-in and focus of clinical staff. Usually, trusts would start seeking out opportunities for programmes that can deliver recurrent savings well in advance of the previous financial year.
However, since the pandemic started, staff have been focused on the immediate operational pressures. There is now some concern about getting sufficient levels of engagement from staff to deliver CIPs at the speed and scale expected given there was limited bandwidth in Q3 and Q4 of 2021/22 to engage in the usual planning process.
Drivers for efficiency savings
Respondents to the survey identified a number of potential drivers for efficiency savings:
Workforce recruitment / retention and reducing staff absences – A number of trusts said that sufficient staffing levels and supporting the wellbeing of the workforce is essential in enabling staff to work productively, reducing sickness absence and limiting agency and bank spend. Trust leaders are already implementing a range of initiatives to expand staff capacity, including enabling those nearing retirement, or who have recently retired, to stay on in the NHS and offering staff greater flexibility over their working hours.
Improving flow into social care and domiciliary care – Respondents told us that difficulty discharging medically fit patients in a safe and timely manner is a key barrier to making productivity gains. If systems can improve patient flow and effective discharge into social care, this will be better for patients and increase productivity.
Data and digital transformation –In its broadest sense, the use of digital solutions eliminates duplication and automates processes, therefore freeing up staff time and NHS resources. Digital initiatives such as electronic prescribing or electronic patient records can reduce human errors and improve safety, preventing avoidable complications in patient care.
Updated IPC guidance – It is unclear precisely what the productivity implications of IPC measures have been over the course of the pandemic. We do know, however, that while essential for patient and staff safety, IPC measures, and the need for social distancing have had a material impact on trusts' ability to deliver efficiency gains.* Since the guidance has been updated, trusts have been positive about the relaxation of measures at this point in the pandemic.
*[Our survey was carried out before the IPC guidance was updated.]
System efficiencies – With the statutory establishment of ICBs approaching, there is real potential to deliver system wide efficiencies. Many respondents highlighted collaborative approaches in schemes across ICSs to make best use of collective resource for patients. However, the capacity for systems to implement cash-releasing productivity growth across the system will be dependent on a number of factors including the maturity of relationships.