Strong clinical leadership at all levels is a feature of high-performing healthcare organisations. For NHS foundation trusts, recent independent research has found it to be a critical factor of successful board leadership to improve the safety and quality of care. However, the relatively low number of clinically-trained individuals on NHS boards and in particular taking up chief executive positions, provides compelling evidence that there are cultural and practical challenges for this group of leaders, that make the leap into executive management seem risky and unappealing.
Our recent leadership report with The King’s Fund reflected the impact that financial and operational challenges, regulatory burden, the risk of organisational failure and rapid staff turnover have had in contributing to perceptions of how difficult the role can be. In addition to constraining the autonomy of leaders within board level roles, these conditions now seem to be discouraging talented, qualified candidates with clinical backgrounds from coming forward to take on chief executive positions.
We also know there are other barriers to progressing into senior NHS leadership positions. Inequalities across gender and ethnicity persist, and the sheer complexity of the operational pressures mean there are very few opportunities for newly appointed chief executives to follow a supported path into the role.
Strong clinical leadership at all levels is a feature of high-performing healthcare organisations. For NHS foundation trusts, recent independent research has found it to be a critical factor of successful board leadership to improve the safety and quality of care.
However, encouragingly, we also know from this research and our previous work, that trust chief executives view their jobs as immensely rewarding: a vocation and a privilege. It is clear from their responses that making a positive impact for large patient populations and for staff within a complex and financially constrained environment provides the biggest personal reward, and biggest challenge, they face in their careers.
This research is based on the NHS Leadership Academy’s response to recommendations made in 2017 by the Faculty of Medical Leadership and Management to the secretary of state for health and social care, to address the barriers and enablers that influence whether clinicians perceive senior executive healthcare management opportunities to be viable and appealing.
This report outlines the results of a survey which NHS Providers conducted in June 2018, to better understand what current trust chief executives see as the main attraction and barriers for clinicians seeking to progress into chief executive roles. The second section provides 13 short case studies from trust chief executives, many of whom hold clinical qualifications themselves, offering insight and advice for clinicians considering whether to follow in their path.
We know from this research and our previous work, that trust chief executives view their jobs as immensely rewarding: a vocation and a privilege.
The professional backgrounds of NHS provider chief executives
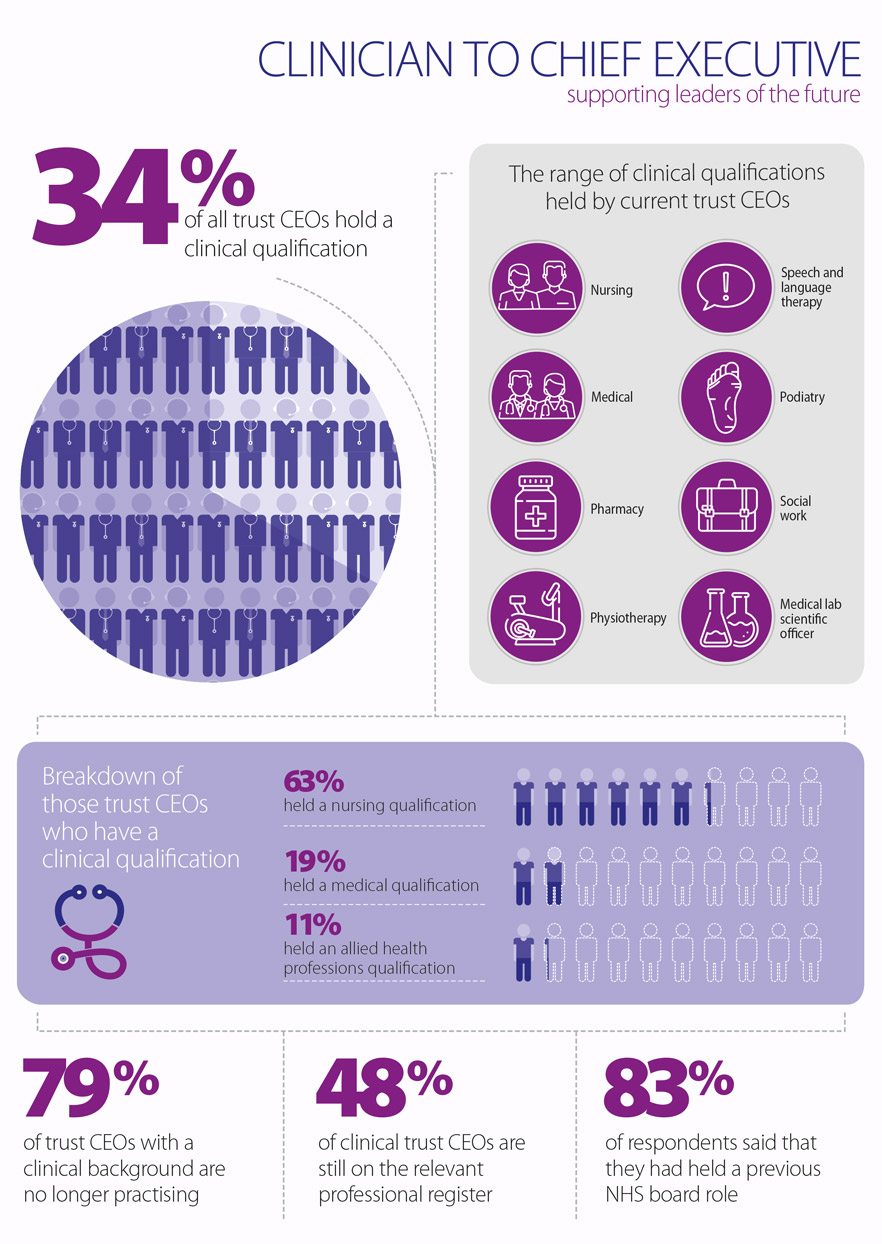
We surveyed all NHS provider chief executives about their professional background and qualifications, and supplemented the findings with desktop based research. The combined results established that a third of chief executives (CEOs) hold a clinical qualification. Of these 78 CEOs, 63% trained as nurses, 19% trained as medical doctors, 4% trained as pharmacists and 11% as allied health professionals (AHPs).
The diversity of professional and education backgrounds among them – while welcome given the breadth of perspective and experience it offers – reinforces the absence of a well-worn path into NHS executive management roles. Clinical CEOs come from varied clinical backgrounds, with 42% from mental health (including psychiatry) and 12% trained in paediatrics. The majority of clinical chief executives also work in the same sector as their clinical specialty.
Of the clinical CEOs who responded to our survey, 77% were appointed in the last five years, and 93% had held a previous NHS board role, most likely to have been medical or nursing director, deputy chief executive, chief operating officer, or manager of an NHS regional organisation. They have, as a group, slightly longer tenure than the 28 chief executives without clinical backgrounds who also responded to the survey, of which 85% were appointed in the last 5 years.
Of the clinical CEOs who responded to our survey, 77% were appointed in the last five years, and 93% had held a previous NHS board role, most likely to have been medical or nursing director, deputy chief executive, chief operating officer, or manager of an NHS regional organisation.
The challenges of maintaining professional practice are well recognised as a particular concern for clinicians considering management roles. Of our survey respondents, 79% of the clinician chief executives are no longer practising. The reasons for this primarily included a lack of time due to the busy nature of their role, and not being able to fulfil clinical requirements as they had limited exposure to patients or clinical practice.
However, 48% of clinical CEOs had maintained their professional registration. Those who were still registered were mostly specialised in nursing (59%), followed by medicine (36%), and pharmacy (5%). The different professional requirements around revalidation may, in part, explain why a higher number of nurses remain on the register compared to doctors. Chief executives who are still practising cited the opportunity to undertake regular shifts which they can schedule effectively with their CEO duties, or have opportunities to shadow their full-time clinical staff and visit wards where they can be involved in directly delivering care to patients in their professional speciality.
Our survey respondents felt strongly that it is necessary to attract more clinicians into the role of NHS chief executive, as part of the broader focus on building up the pipeline of future NHS leaders with the necessary skills and experience to lead in such a complex environment. They also suggested that prospective applicants will benefit by gaining real on-the-job experience by spending time with a range of CEOs leading NHS provider organisations, and that there is a need to start encouraging clinicians to consider a future in management much earlier in their career. They also felt the NHS needs to do more to directly tackle the practical barriers and risks relating to senior management for clinicians and to consider the post-CEO pathway for clinicians who desire to return to practice after their tenure as a CEO.
Encouragingly, the majority of our survey respondents indicated they are willing to offer their experience as mentors or advisors to aspiring clinical chief executives. NHS Providers and the NHS Leadership Academy and are currently exploring now how best to deliver this opportunity to grow our future NHS leaders.