

This week marks the end of our Winter watch series with this being the last week that the winter daily sitreps are published. The week 14 data covers 25 February - 4 March and reflects NHS performance over one of the coldest and the most snowy week of winter. Today also sees the publication of some February performance figures.
Following Simon Stevens announcement that February was the most pressured month ever for the NHS it is no surprise to see that the A&E 4-hour waiting-time target for February is at a record low of 85%. The 4-hour target for type 1 attendances has fallen to an all time low of 76.9%. Despite the performance against the target the NHS managed to see over 1.5 million people from arrival to admission/transfer or discharge within 4 hours, an increase of 2% from February 2017.
But what does the rest of the data tell us?
- general and acute bed occupancy holds at the high of this winter at 95.2%, well above the recommended level of 85%
- the average number of beds occupied for more than seven days is at the highest it has been all winter at 46,311
- there are still 23% more escalation beds open than this time last year; although the number has fallen since last week
- the impact of norovirus has fallen significantly since last week with an average of 751 beds being closed each day but this is also 23% higher than this time last year
- the number of A&E diverts rose to 33 from 13 last week but is still less than this time last year
- ambulance handover delays are down when compared to last week, with 12.7% being delayed over 30 minutes and 2.8% being delayed over 60 minutes
- the number of ambulance arrivals was the lowest it has been all winter but this will be , in part, due to the weather conditions last week.
You can find out more about what the data means in our new explainer and download our winter sitrep dashboard to see the figures in more detail.
The 4-hour waiting-time target for February is at a record low of 85%. The 4-hour target for type 1 attendances has fallen to an all time low of 76.9%.
The story of winter
This week Adam Brimelow, NHS Providers deputy director of communications, wraps up our Winter watch series with his reflections on how the story of the winter unfolded for the NHS this year.
This winter large parts of the NHS have been in survival-mode. Our Winter watch series has highlighted the planning, innovation, teamwork and commitment that helped the health service through. It’s revealed the dogged determination and – at times – heroic devotion to duty required to keep the show on the road.
This was - above all - a test of resilience. Despite a late dollop of extra cash in the budget, there was plenty to worry about last November, heading into winter. The main concern was capacity – would there be sufficient beds and staff to cope with ever-growing demand, including increasing numbers of very frail, sick patients requiring complex care?
In week 1 we heard about the key steps in place in hospitals, mental health and community trusts and ambulance services to ensure that with the limited resources at its disposal, the NHS was battle-ready.
Our Winter watch series has highlighted the planning, innovation, teamwork and commitment that helped the health service through. It’s revealed the dogged determination and – at times – heroic devotion to duty required to keep the show on the road.
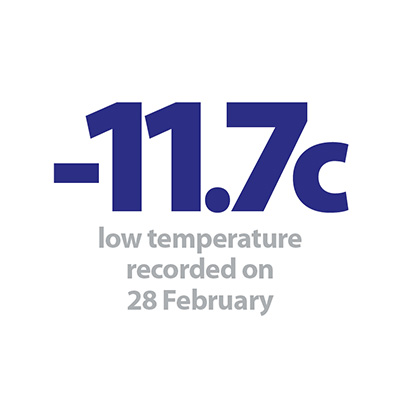
And what a battle. Pressures grew right on cue in weeks 2, 3 and 4 with rising rates of norovirus symptoms and flu. These posed difficulties right through the winter, aggravated by the impact of freezing temperatures, causing falls, fractures and respiratory problems. And finally, a late mauling by the Beast from the East.
These pressures were reflected in the weekly "situation reports" and monthly combined performance summaries published by NHS England that informed our analysis. Emergency admissions rose relentlessly. Bed occupancy rates remained at or around 95% - well above recommended safe levels. These pressures fed back through the system, adding to delays in A & E and for patients being handed over to hospital from ambulances.
Our blogs from NHS frontline leaders provided a real-time commentary on these pressures and some of the solutions that helped the NHS win through. Simon Sethi from Yeovil Hospital NHS Foundation Trust explained how working with partners had helped to reduce patients’ length of stay and meet the four hour standard in A & E.
In her video contribution on Provider Bites, Carolyn Regan from West London Mental Health NHS Trust highlighted the value of planning: putting in extra beds to deal with winter pressures, alongside support to help people stay in their own homes. As a result nearly 80% of people they have worked with in the community have not needed an admission.
Emergency admissions rose relentlessly. Bed occupancy rates remained at or around 95% - well above recommended safe levels. These pressures fed back through the system, adding to delays in A & E and for patients being handed over to hospital from ambulances.
Sonia Swart from Northampton General Hospital NHS Trust gave a compelling account of how staff ensured patient safety for those waiting on trolleys in corridors:
Every single patient that weekend and every set of relatives felt that the care had been good and safe. They were full of praise for hospital and ambulance services alike – with the waiting regarded as an inevitable consequence of NHS pressures.
Chief executive, Northampton General Hospital NHS Trust
Wayne Bartlett-Syree from East of England Ambulance Service NHS Trust explained how these pressures – felt right across the urgent and emergency care system - are impacting on the safety of patients in the community:
It is now commonplace over the winter period for A and E corridors to become full of patients and ambulances to queue outside emergency departments. It means that patients in the community could be having heart attacks and strokes when there are no ambulances available to provide an emergency response. The risk of harm is now transferring from those in corridors to patients in the community needing an ambulance.
Director of strategy and sustainability - East Of England Ambulance NHS Trust
That stark warning contains an important message for rest of this year and next winter. We can not, must not allow people to be put at risk in this way.
But for me the most powerful frontline accounts in Winter watch described acts of kindness and compassion by staff giving their all to make life better for people in their care. They included the paramedic who camped out in the snow close to work to make sure he could be in for his shift the next day, the midwife on leave who skipped a Christmas party to help a mother have her planned home birth, and the staff who brought forward Christmas day on the ward, so a dying patient could share a special final celebration with her family.
Yes, winter tested the resilience of the NHS to the limits and most likely will again next year. But with that kind of spirit and commitment, there is always hope it can continue to rise to the challenges ahead.
NHS trusts in survival-mode pulled out all the stops this winter
Responding to the latest sets of performance data from NHS England, NHS Providers deputy chief executive, Saffron Cordery, said:
"These figures encapsulate the story of this winter for the health service.
"NHS trusts and frontline staff pulled out all the stops to keep services running, and managed to treat more patients than ever – a really significant achievement.
"But the reality is that large parts of the health service have been in survival-mode for much of the winter
"The NHS was unable to match the relentless rise in demand for care. Consequently, too many patients suffered delays, distress and inconvenience while staff were put under intolerable pressure.
"Of course the cold weather combined with high rates of flu and norovirus symptoms were major factors.
"But the prolonged financial squeeze and workforce shortages have compromised the ability of the NHS to respond in a safe and timely way to spikes in demand.
"We need to see urgent steps put in place to ensure sustainable long term funding for health and social care."