

Unfortunately the data in this week's sitreps seems to be heading in the wrong direction. At the same point last year we began to see cases of diarrhoea and vomiting (D&V) and norovirus fall and the number of escalation beds reduce. But this year many key indicators that monitor capacity in the system are on the up again as we head into the end of February.
Whilst the number of A&E diverts has fallen, the actual number of ambulance arrivals has increased since last week. The waits on the forecourts at emergency departments, seem to be increasing again with 14.3% of ambulance handovers being delayed by 30 minutes or more - an increase of nearly 3% on last week.
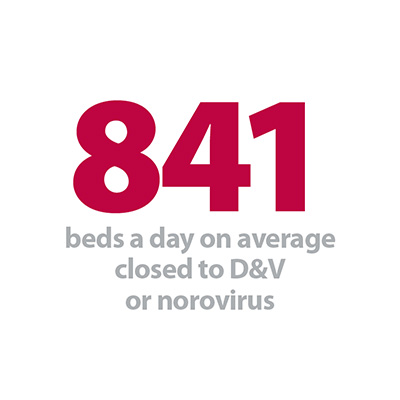
The number of beds a day on average closed to D&V and norovirus has shot up by a third in just two weeks meaning that norovirus continues to place a strain on bed availability. To cope with this and the impact flu has had this winter, trusts across England have again increased the number of escalation beds they have - this currently stands 24% higher than at this time last year.
At the same point last year we began to see cases of diarrhoea and vomiting (D&V) and norovirus fall and the number of escalation beds reduce. But this year many key indicators that monitor capacity in the system are on the up again as we head into the end of February.
Long hospitals stays are also on the up again - with nearly 18,000 beds being filled by people who have been in hospital for 21 days or more.
Bed occupancy is holding firmly at 95% and has been for seven weeks. From the figures published this week, coupled with continuing cold weather, it is difficult to imagine the figures improving by the last week in our winter watch series - but certainly not the last week of 'winter pressures' for NHS staff.
You can find out more about what the data means in our new explainer and download our winter sitrep dashboard to see the figures in more detail.
Insight from the frontline
This week Phil Luke, deputy chief operating officer of Royal Devon and Exeter Trust explains how despite a difficult winter, local collaboration and the strengthening of local partnerships has been a positive development that will have a lasting impact and result in East Devon being better prepared next year.
"It is true that this winter has been one of the toughest for many years, putting intense pressure on hard working staff right across the system in eastern Devon:
- Levels of flu are more than double the level experienced last year, triggering a rise in admissions for patients over 75, as well as impacting on staffing levels
- Flu affected all our community hospitals and 25 of our local care homes closed at some point this winter
- Although not as high profile this year, norovirus has also been a big challenge shutting down ward space when we most needed it
- Recruiting and retaining enough staff to deal with increasing demand has also been difficult
From GPs and primary care professionals to acute sector staff, colleagues in social and domiciliary care provision and carers at home, many of them elderly themselves; the pressure has been real and has tested us all. However, amidst this pressure, we’ve seen lots of examples of great leadership and innovation from staff across all parts of the system.
The close working with partners in primary care, 111, the Ambulance Trust, Social Services, mental health, regulators and leading domiciliary care providers enabled us to refine and strengthen our winter plans.
Deputy chief operating officer of Royal Devon and Exeter Trust
If there is one take home message from the eastern Devon system this winter, it would be that the deepening collaboration that comes from organisations coming together during difficult times is the only way through.
We have made huge strides in forging open, trusting relationships with partners from across health and social care as we all grapple with complex issues in a constrained financial environment. The close working with partners in primary care, 111, the ambulance trust, social services, mental health, regulators and leading domiciliary care providers enabled us to refine and strengthen our winter plans.
More locally, having welcomed community services into the trust around 18 months ago, we’re still learning about the complex risk management undertaken by community staff on a daily basis and this is helping the system think differently about what is in the best interests of patients.
We’re proud of what our teams have achieved this year, but we’re already focused on working with partners from across health and social care to improve things for winter 2018/19.
Deputy chief operating officer of Royal Devon and Exeter Trust
In advance of next winter, as a system, we will be in a stronger position to co-create system-wide plans, which will increase the resilience of services and support staff in all organisations in caring for patients and we are already working together on what we need to do differently to prepare for the winter ahead.
Defining the story of this winter only by its challenges is tempting, as this year has certainly been one to remember. But the tendency to describe performance by the number of failures in the system, however, cannot be right.
While every cancellation is a matter of regret and impacts on individual patients, it remains important to step back and reflect on what we have achieved. In January, for example, whilst 11.7% of patients were not admitted or discharged from ED within 4 hours, 88.3% out of 8839 people were successfully treated in less than 4 hours - including patients whose lives will have been saved by the combined hard work, expertise and professionalism of staff from all disciplines.
We’re proud of what our teams have achieved this year, but we’re already focused on working with partners from across health and social care to improve things for winter 2018/19."
Defining the story of this winter only by its challenges is tempting, as this year has certainly been one to remember. But the tendency to describe performance by the number of failures in the system, however, cannot be right.
Deputy chief operating officer of Royal Devon and Exeter Trust
Responding to the winter operational update from NHS England, NHS Providers director of policy and strategy, Saffron Cordery, said:
"These figures show that far from easing as we start to head towards spring, the pressures on the NHS are intensifying.
"Trusts and frontline staff are doing all they can to provide safe, timely, high quality care for patients.
"But the increase in ambulance handover delays reflects the difficulties they face in ensuring there is enough capacity, including beds and staff, so that patients get the standard of care they have a right to expect.
"That is despite having nearly 25% more escalation beds in place than last year – to deal with exceptional winter pressures – and the number is still rising.
"Even so, bed occupancy – at 95% – remained well above recommended safe levels.
"These figures provide a further snapshot of the unsustainable pressures that were presented in yesterday’s Q3 data published by NHS Improvement.
"They showed in stark detail how demand is rising much faster than funding. Trusts are not only having to treat larger numbers of patients but more of those patients have serious, complex, illnesses.
"Trust leaders increasingly are telling us 'we cannot carry on like this'.
"The warning signs are clear and in plain sight.”