The GIRFT programme commenced as a national programme in November 2016, building on the original work of consultant orthopaedic surgeon Professor Tim Briggs who pioneered the programme in orthopaedics.
The GIRFT programme is one element of the government’s response to the recommendations of Lord Carter’s Operational productivity and performance in English NHS acute hospitals: Unwarranted variations report, published in June 2015. In that report, Lord Carter examined data from all acute trusts in England and developed eight headline recommendations across clinical and non-clinical domains designed to reduce unwarranted variation in the delivery of care. The first recommendation was to develop an efficiency metric for NHS providers to use, to review performance against their peers and create a baseline for improvement. The GIRFT programme’s use of benchmarking trusts to identify variance in performance is a practical manifestation of this approach. Whilst the programme is not formally mandatory for trusts to participate in, trusts are strongly encouraged to be involved.
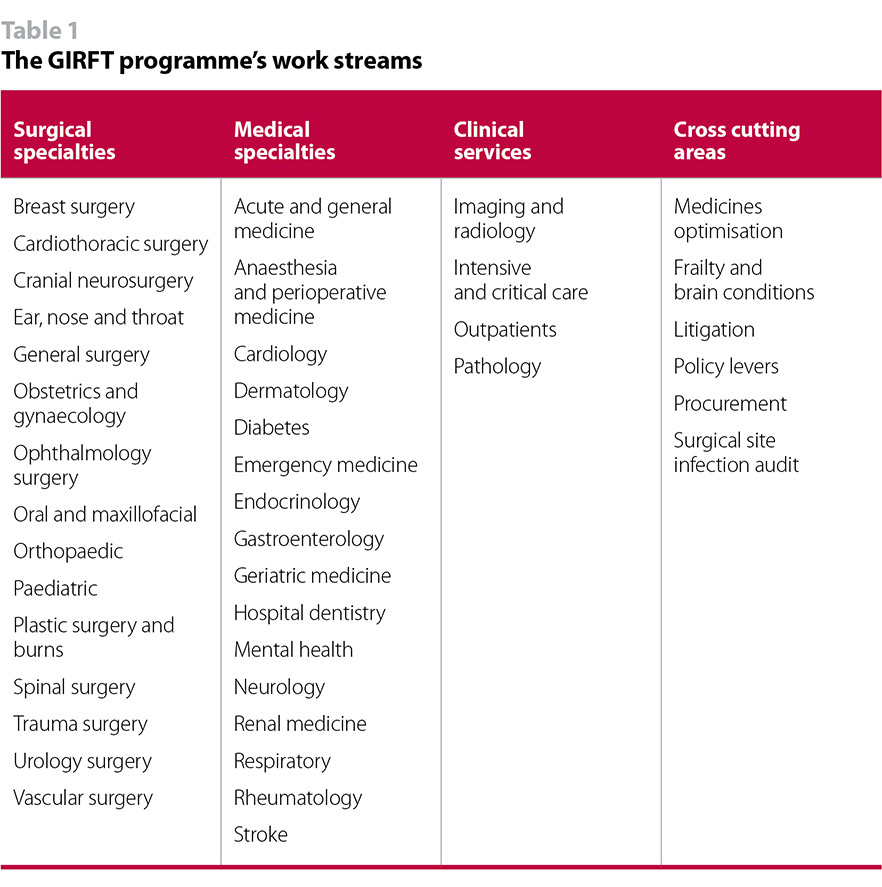
The GIRFT programme’s work covers 35 surgical and medical specialties, of which 25 have commenced, along with six cross cutting work streams (Table 1). The remaining specialties will begin in waves from summer 2018. There are currently 150 trusts participating in the GIRFT reviews, and all hospitals in England will be approached to take part. Following the publication of the GIRFT national general surgery report in August 2017, vascular surgery is the next GIRFT national report, due in February 2018.
The mental health services stream within the medical specialties is in very early development, but the programme will be looking to reduce out of area placements and unwarranted variation in quality in three areas:
- adult mental health acute and crisis care services
- children and young people’s mental health services including Tier 4 CAMHS
- long-term complex care and locked rehabilitation wards.
The programme doesn’t currently apply to community and ambulance trusts.
NHS Improvement aims to generate between £1bn and £1.8bn of productivity gains in 2017/18, with an overall productivity saving target of £6bn by 2020/21.
Funding and projected returns
GIRFT is supported with £60m of funding from the Department of health and social care (the Department) but is part of NHS Improvement’s operational productivity programme, as one of eleven sub-programmes designed to support all NHS Trusts to deliver increased productivity, reduce unwarranted variation and improve quality of services.
A detailed independent review of the original GIRFT orthopaedic programme is also currently underway led by University College London, due to conclude in December 2018.
The GIRFT programme is one of the key pillars of the NHS operational productivity programme. NHS Improvement aims to generate between £1bn and £1.8bn of productivity gains in 2017/18, with an overall productivity saving target of £6bn by 2020/21. Of this, the GIRFT programme is aiming to deliver between £240m to £420m in 2017/18 and £1.4bn per year by 2020/21. Out of the areas currently identified by NHS Improvement, the GIRFT programme has one of the most ambitious savings target attached to it – the proposed savings identified, for example, are larger than identified savings from E-rostering and more effective job planning.
Although the projected GIRFT savings could account for just over a quarter of the financial gap facing the NHS by 2020/21, caution is required when interpreting any headline financial savings taken which have been extrapolated from top-level benchmarking data from trusts. Furthermore, identifying the savings does not automatically incentivise the changes required on the ground to achieve them. There is complex work required to agree how to tackle the underlying factors, deliver the changes to clinical practice required, and release cash savings or, more feasibly, improve the overall productivity of current resource allocations. This work takes time and must be achieved in consideration of matters specific to local contexts, such as the implications of fixed and variable costs.
It is also important to recognise that trusts are already actively engaged in efforts to reduce unwarranted variation, drive out wasteful spending and deliver savings. NHS trusts already achieved £3.1bn of savings through cost improvement programmes (CIPs) in 2016/17, £200m more than in 2015/16. The NHS is also outperforming its historic productivity, as well as recent UK economy productivity. The University of York calculated that productivity increased across the NHS by an average of 1.7% a year between 2009/10 and 2014/15, above the long-run average for the NHS of 0.9% and above recent whole economy productivity of 0.4% a year.
The NHS has a strong track record of delivering savings and efficiencies, as evidenced by work over the past seven years since the NHS budget has been under substantial pressure. In this way, the GIRFT programme should be seen as building on existing initiatives and efforts across the sector to unlock efficiency savings, with the key difference being the type of national support and focus put into the programme and the primacy of clinical engagement.
NHS trusts already achieved £3.1bn of savings through cost improvement programmes (CIPs) in 2016/17, £200m more than in 2015/16. The NHS is also outperforming its historic productivity, as well as recent UK economy productivity.
Leadership and structure
Delivery of the GIRFT programme is a partnership approach between the Royal National Orthopaedic Hospital NHS Trust and NHS Improvement. An executive team is jointly led by Professor Tim Briggs, as chair of GIRFT and NHS Improvement’s national director of clinical quality and efficiency, Dr Jeremy Marlow, executive director of operational productivity, NHS Improvement, and Rob Hurd, chief executive of the Royal National Orthopaedic Hospital NHS Trust, as joint senior responsible officers of the programme.
Each clinical specialty has a national lead with responsibility for managing a national review of their specialty, visiting every trust that undertake that service. There are currently 41 appointed clinical leads and advisors. The majority of clinical leads have been recruited with assistance from their specialty’s Royal College or professional society.
Seven GIRFT regional hubs headed by implementation managers will function as centres from which clinical and project delivery leads can support and advise on delivering recommendations emerging from the clinical lead visits. In addition, the GIRFT regional hubs will support the implementation of the national report recommendations into local practice.
Operation
We outline below the main processes that take place when a clinical specialty is reviewed as part of the GIRFT Programme.
Methodology and six-phase implementation process at trust level
Phase 1 – preparation: GIRFT specialty clinical leads examine trust data looking for unwarranted variations; differences between trusts in areas such as effective procedures, length of hospital stay, infection rates and costs. The GIRFT team analyses data from multiple data sources, including hospital episode statistics, NHS Litigation Authority, and relevant data streams for each clinical area including registry and professional body data.
Phase 2 – data pack distribution: A bespoke data pack is produced for each trust delivering the specialty under review. This helps clinicians and managers understand what the variations are, what needs to be done to address them and explore the challenges they face.
Phase 3 – clinical lead visits: The GIRFT clinical lead undertakes a number of ‘deep dive’ visits to present the trust report and discuss the data with the hospital team. GIRFT regional hubs aid trusts with interpreting their datasets, building and delivering the implementation plans.
Phase 4 – national report publication: After at least 40 trust reviews have been completed for a clinical specialty, the emerging trends from the visits to trusts and analysis of datasets enable the lead clinician to write a national report. The national report presents the original benchmark data, GIRFT’s findings, examples of best practice, and an action plan of proposed changes and improvements, supported by an implementation programme. Where appropriate, these national recommendations are added to trust implementation plans.
Phase 5 – data refresh: Core GIRFT data will be updated on an annual basis to enable trusts to monitor progress and, where necessary, reprioritise implementation efforts. The GIRFT analytics team refreshes and re-issues the trust data packs, and the specialty clinical leads revisit trusts.
Phase 6 – transition to business as usual: Regional hub teams support trusts to complete actions in the implementation plans and transition improvements into business as usual. Across the programme, more than 1,000 ‘deep dive’ visits to around 150 trusts have taken place so far.
The first specialty report of the new programme, covering general surgery, was published in August 2017, with the vascular surgery report due in February 2018. Of the GIRFT reviews currently underway, cranial neurosurgery, cardiothoracic surgery and urology are the most advanced and therefore closest to the publication of their respective national reports.
As noted earlier, each trust will work with regional GIRFT teams to develop an implementation plan in a given specialty. This will be informed by the relevant national specialty report as well as the local GIRFT review. The implementation plan will be updated on a rolling basis by the GIRFT regional team to ensure alignment with relevant national initiatives including NHS Right Care (NHS England’s national programme for reducing unwarranted variation in commissioning) and sustainability and transformation partnerships (STPs). The model hospital portal – an NHS Improvement tool that allows users to compare productivity, quality and responsiveness data, an approach which emerged from the Carter review – will act as the gateway for accessing GIRFT information for all providers and commissioners.
The NHS has a strong track record of delivering savings and efficiencies, as evidenced by work over the past seven years since the NHS budget has been under substantial pressure.
Timescales
NHS Improvement expect that clinical specialty reviews take between 6-24 months depending on size of the workstream. It is anticipated that the average workstream will take 36 months from initiation to 'business as usual' activity at the trust. If the final wave of specialty reviews start in March 2018, all workstreams are projected to be 'business as usual' across all trusts by March 2021, though it is recognised that formal support for GIRFT may need to extend longer than this timeframe if roll-out takes longer than planned.