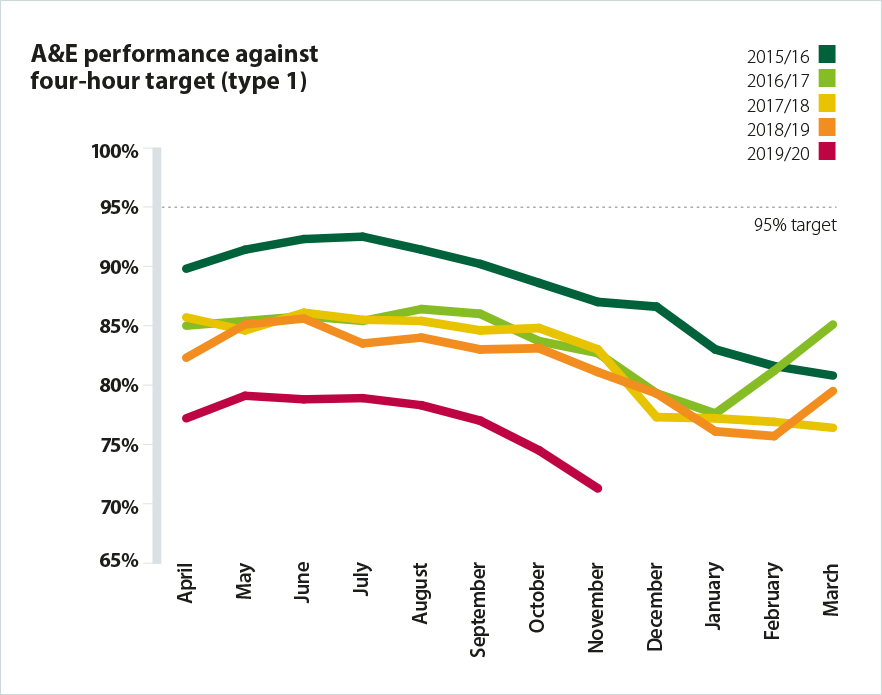
NHS urgent and emergency care performance is traditionally measured against the four-hour acute hospital standard – 95% of patients being treated, discharged or admitted with four hours. Performance against this target is already at the lowest levels ever recorded, before the winter period even starts. The latest statistics show that no providers with a major A&E department met the 95% standard in November, either for all attendances or type 1 only. Instead, the average percentage of patients seen within four hours for all types was 78.6% for all providers with a major A&E department.
Performance against the standard has continuously declined for each of the last five years and as the chart below shows, it seems almost inevitable there will be another sharp decline this year.
Trust leaders report that they are seriously concerned that performance this winter is in danger of falling to levels that will risk patient safety and have a strong adverse impact on patient experience.
This seems likely to manifest in the following ways:
-
busy primary care and GP services, and stretched community health services leading to increased potential for patients to opt to, or to need to, seek support from A&E
-
overcrowded A&E departments, with patient experience deteriorating as staff do not have the physical space available to provide the quality of treatment they would wish to
-
delays in ambulance handovers, meaning insufficient available ambulance capacity to deal with emergency calls and greater risk as patients conveyed in ambulances have to wait to access hospital emergency departments
-
longer waits for patients, including a significant increase in the number of waits over 12 hours which evidence shows significantly increase the risk to patient safety
-
care being provided in corridors, on trolleys and in temporary spaces which will adversely affect patient experience and potentially risk patient safety
-
insufficient capacity to provide the right care to those in mental health crisis, either presenting within an A&E setting or at other location – potential for pressure on community mental health services, mental health beds, and potential for increases in out of area placements
-
difficulty ensuring good flow throughout hospitals and at the interface with community services, with potential for delayed discharges
-
difficulties ensuring access to timely social care and other services in the community.
It is impossible to predict the precise impact the winter conditions may have. This will vary by trust and by time of day and depends on factors like weather and flu and norovirus rates. In previous years, only a few trusts were overwhelmed for short period of times (e.g. 24-48 hours) before they stabilised. It seems likely that, this winter, significantly more trusts could be overwhelmed for longer periods of time and will take longer to stabilise. We would expect this to be reflected in the statistics on operational pressures escalation levels alerts, ambulance delays and redirections, and 12 hour waits – not just the overall numbers of such incidents but the number of trusts affected by them.